76. Sarcoidosis
Definition
Sarcoidosis is a chronic multisystem inflammatory disease characterized by noncaseating granulomas as well as lymphocytic alveolitis.
Incidence
In the United States the overall incidence of sarcoidosis ranges from 5:100,000 to 40:100,000. Among Caucasians the incidence is about 11:100,000, but among African Americans the incidence is about 34:100,000. Internationally the incidence varies with the country as well as the degree of development of the country. For example, in Sweden the incidence is about 20:100,000, whereas in Japan the incidence is about 1.3:100,000. Sarcoidosis has been reported in most countries. In developing countries it is frequently misdiagnosed as tuberculosis. This disease affects men more frequently than women by a 2:1 ratio.
Etiology
The true cause of sarcoidosis is not known. There is evidence of both genetic and environmental causative factors. Sarcoidosis is not a malignant disease, nor is it an autoimmune disease.
Possible Pathogenic Causes of Sarcoidosis
• Chlamydia
• Epstein-Barr virus
• Mycobacteria species
• Mycoplasma species
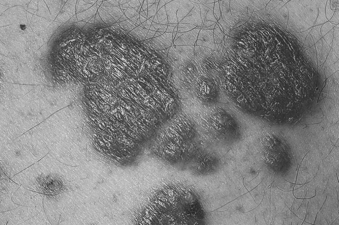 |
| Sarcoidosis. Erythematous annular plaques. |
Signs and Symptoms
• Alveolitis
• Anorexia
• Bell’s palsy
• Deafness
• Depressed gag reflex
• Dysphagia
• Elevated monocyte count
• Fatigue
• Hepatomegaly
• Hilar lymphadenopathy
• Hoarseness
• Interstitial nephritis
• Iritis
• Night sweats
• Nonproductive cough
• Peripheral lymphadenopathy
• Shortness of breath
• Skin lesions
• Splenomegaly
• T-cell lymphadenopathy
• Vertigo
• Vocal cord paralysis
• Weight loss
Medical Management
Symptomatic treatment is the only therapeutic measure most patients require. Corticosteroids currently remain the primary course of treatment, but noncorticosteroidal medications are increasingly being used. Methotrexate is often used in place of drugs such as prednisone. Other alternative medications include hydroxychloroquine, cyclosporine, pentoxifylline, and azathioprine. Sarcoidosis that proves refractory to any of these pharmacologic agents may be treated with infliximab and/or thalidomide. Cutaneous manifestations may be treated with tetracycline.
Pulmonary manifestations characterized by asymptomatic pulmonary function tests and/or chest x-rays may not require treatment. Symptomatic/abnormal pulmonary function test results and symptomatic chest x-ray findings generally signify that treatment is needed. Treatment is especially indicated with objective evidence of recent lung function deterioration. Administration of corticosteroids may produce some measure of improvement, but only a small degree. For endobronchial involvement, inhaled corticosteroids may be given.
Surgical intervention is limited. Bilateral lung transplantation is the most viable option for the patient with sarcoidosis in whom the disease has produced significant fibrosis. Transplantation is also an option for the sarcoidosis patient who is in Stage IV of the disease and should be seriously considered when the patient’s forced vital capacity (FVC) and forced expiratory volume in 1 second (FEV 1) fall below 50% and 40%, respectively, of the patient’s expected values.
Complications
• Cardiomyopathy
• Cor pulmonale
• Cranial nerve palsies
• Diabetes insipidus
• Encephalopathy
• End-stage lung disease
• Heart block
• Hypothalamic and/or pituitary dysfunction
• Lymphocytic meningitis
• Pericardial effusions
• Progressive pulmonary fibrosis
• Pulmonary hypertension
• Renal failure
• Right-side heart failure
• Seizures
• Sudden death
Anesthesia Implications
The first concern for the anesthetist whose patient has sarcoidosis centers on the degree of pulmonary involvement. Often there is significant disparity between expressed symptoms and the degree of pathologic changes. The patient’s pulmonary function tests (PFTs) should be determined preoperatively, when possible. In addition, the patient’s diffusing capacity and arterial blood gas analysis should be completed preoperatively to delineate the degree of hypoxemia and the impact the disease will have on the delivery of volatile anesthetics. Sarcoidosis produces significant loss of lung compliance, in this case producing restrictive lung disease. Both inspiratory and expiratory phases of the ventilation cycle should be prolonged to reduce the potential for barotrauma and air trapping. The inspiratory phase can be lengthened by selecting the pressure-controlled ventilation setting of most modern anesthesia machines along with lower peak inspiratory pressure settings for the inspiratory phase. The expiratory phase should be set for a ratio (I:E) of 1:2.5 or 1:3 to allow for more complete excursion. The loss of compliance along with decreased diffusing capacity produced by sarcoidosis may significantly alter the speed with which the depth of anesthesia can be changed. The anesthetist and the patient should have a preoperative discussion regarding the potential necessity of continuing mechanical ventilatory support into the postoperative period. Even when extubated, the patient must still be closely observed for a relatively longer time for signs of laryngeal edema and airway compromise, particularly for the patient with significant granulomatous infiltrates of the larynx. Patients with laryngeal involvement have been documented to suffer significant airway edema and compromise up to 36 hours postoperatively.
The second major concern for the anesthetist involves the degree of cardiac involvement. Cardiac involvement may be primary—directly the result of myocardial granuloma infiltration—or secondary—the result of the extensive pulmonary effects of the disease. Granulomatous infiltration of the myocardium may result in conduction abnormalities, such as first-degree atrioventricular conduction delay, bundle branch block, or even complete or third-degree heart block. It may also produce ventricular dysrhythmias, pericarditis, supraventricular tachycardia, ventricular aneurysms, or even sudden cardiac death. Myocardial effects of pulmonary manifestations may result in right-sided or congestive heart failure. The patient with sarcoidosis should have a 12-lead electrocardiograph evaluation performed preoperatively to detect any change in cardiac conduction abnormalities, along with a two-dimensional echocardiogram assessment to detect mechanical functional abnormalities resulting from the disease. Both studies should ideally be completed shortly before the anticipated surgery, preferably less than 30 days preoperatively, to alert the patient and anesthetist to any pathologic changes. The patient may require placement of a pacemaker or internal cardiac defibrillator before the proposed surgical procedure, or the device may have already been implanted. Even though implanted for protective purposes, the internal defibrillator may have to be inactivated during surgery because the device may be triggered by electrocautery.
The patient with sarcoidosis may experience dysphagia and a depressed gag reflex as a result of granulomatous infiltration of cranial nerves (CN) IX and X, respectively. General anesthesia, when used, should be achieved via classic rapid sequence induction standards, with the patient’s head elevated about 30 degrees to reduce the potential for aspiration. Extubation on completion of anesthesia requires that the patient be in very good control of his or her airway with return of protective reflexes. Humidified oxygen in the postoperative period will help soothe some of the airway irritation. The anesthetist must recall the greater potential for delayed airway compromise, particularly if the initial laryngoscopy and intubation were difficult to any degree. Signs and symptoms of laryngeal edema and/or airway compromise should be aggressively pursued and managed with dexamethasone and racemic epinephrine administration along with heightened observation and reintubation if necessary.
Intraoperatively, the patient with sarcoidosis may require placement of a pulmonary artery balloon floatation catheter and/or transesophageal cardiography probe to obtain more accurate data regarding fluid resuscitation and/or hemodynamic requirements. The patient may also benefit from placement of a peripheral arterial catheter for more accurate, beat-to-beat blood pressure monitoring, which will also facilitate serial arterial blood gas sampling perioperatively.
The patient with sarcoidosis is typically treated with long-term corticosteroid administration. The anesthetist should take care to follow the established administration routine for perioperative steroid coverage.
Sarcoidosis may occasionally affect the kidneys. The anesthetist should be alert for the potential for renal insufficiency in the patient with sarcoidosis. The patient should have a complete metabolic panel obtained preoperatively to ascertain any electrolyte and/or fluid balance abnormalities.







