CHAPTER 22 Saline Implants
Getting a Good Result
Summary/Key Points
Patient Selection
Given that nothing needs or should be done to the breast parenchyma and there is no change in the risk of breast cancer from the procedure1 a routine mammogram should not be required of patients preoperatively if there is otherwise no reason for one. If the patient needs a mammogram based on their age, physical findings, or some other reason, then they should have one done before the procedure.1
Physical findings of the breast that would preclude the patient from primary cosmetic breast augmentation as a sole procedure include active breast disease or undiagnosed palpable abnormality of the breast. Previous treatment for breast cancer or radiation treatment would put the patient in the category of breast reconstruction. Ptosis of the breast beyond about 2 cm into Grade II2 is a cosmetic contraindication to primary breast augmentation in my experience. Two centimeters or less can be compensated for using a properly placed breast implant and is usually of more benefit than any type of mastopexy procedure as long as the patient is willing to accept the increase in volume and understands that an implant will not truly lift the breast but only fills it out.
One of the listed complications of cosmetic surgery that is perhaps too common but can be avoided is the aesthetic risk of dissatisfaction with the result. This is best avoided by telling the patient what a breast augmentation can do and can’t do and what the patient can choose for her own reasons and what is being done based on experience of the surgeon on how to get the best result (Table 22.1).
| The key to consistent natural results with saline-filled implants requires thinking dimensionally as in fitting a woman for clothes or fitting an orthopedic implant and giving up thinking in terms of volume alone. This can all be done preoperatively and should not require choices made during surgery. |
| Avoiding visible rippling requires: |
The other area that is often missed in the evaluation of patient selection is whether the patient has adequately prepared for the recovery. Contrary to efforts by some to convince the patient that they can return to normal activity the next day,3 I recommend treating breast augmentation as an orthopedic procedure and require that the patient has a week off from any and all required activities other than taking care of herself. This helps to magnify the consequences of the procedure and the importance of the recovery in the overall result as well as help to avoid precipitous surgery and poorly thought out choices. It also allows for the enormous variation in perceived pain and recovery difficulty among patients after what is ostensibly the same procedure.
Indications
Their major disadvantage is their inherent watery or ripply feel.
Silicone gel-filled breast implants have several disadvantages:
Their major advantage is their inherent natural or tissue-like feel.
Preoperative Planning
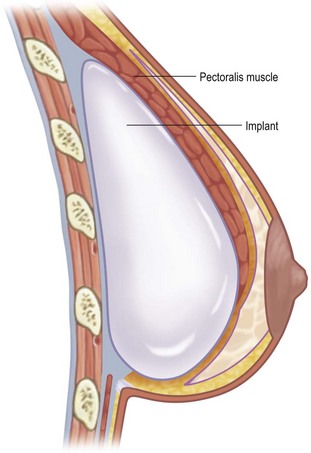
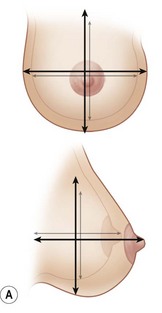
Degree of coverage starts from a rating of near zero and completely inadequate in a woman with thin or very soft skin, virtually no subcutaneous fat, and essentially no breast tissue. This is a situation comparable to someone whose ribs are sticking out or a woman who has had an aggressive subcutaneous mastectomy or full mastectomy. Perfect coverage would be rated a 3 with thick elastic skin, normal or more subcutaneous fat, and average breast tissue. In that situation, the woman is not going to be able to feel the implant to any significant degree and it won’t matter whether it’s saline-filled or gel-filled. In between the extremes are where most patients fall and there are those who have adequate coverage laterally but inadequate in the inferior pole, particularly in the somewhat ptotic or pseudo-ptotic (Fig. 22.1).
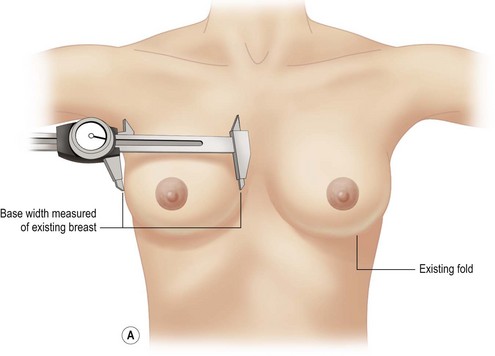
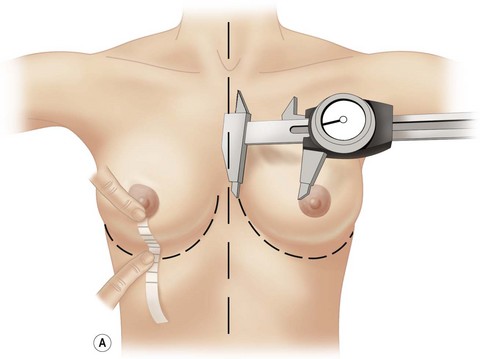
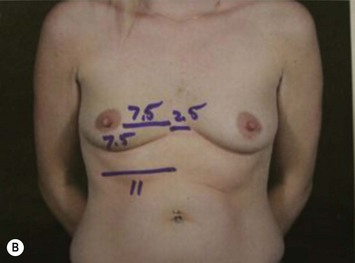
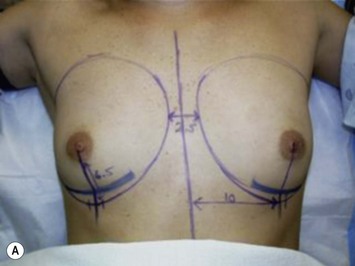
The patient has chosen saline implants and the profile of the implant. The width of the implant is determined by the width of the breast (Figs 22.2 and 22.3). Therefore, the correct implant is known before the procedure and can be confidently placed without using sizers, sitting the patient up during the procedure, or making choices for the patient on the operating table (Fig. 22.4A–C).
The only other marking required preoperatively is the position of the inframammary crease in the upright position. On the operating table, the distance from the medial border of the breast to the nipple (or medial edge of the areola) can be measured under no tension and compared to the distance from the nipple (or inferior edge of the areola) under tension. With few exceptions related to extreme lateral positioning of the nipple–areola, comparing these two measurements determines whether a round implant of the width of the inner diameter of the breast will fit and seat properly behind the nipple–areola. If the distance to the inframammary crease is too short, the crease must be lowered to the appropriate level and re-established and healed in the new position (Fig. 22.2A, B).
During the preoperative consultation, the physical characteristics of the breast should be noted and pointed out to the patient (see Box 22.1).
Box 22.1 Physical characteristics of the breast
With the characteristics listed in Box 22.1, it can be determined whether a round implant will fill out the breast adequately, the width of the implant that will fit it, whether the inframammary crease will need to be adjusted, how much soft tissue coverage is available to make the saline-filled implant less palpable, and any issues the patient needs to be aware of that will not be corrected by a breast implant alone.
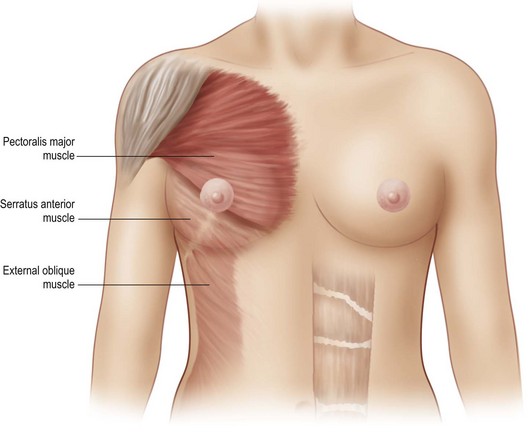
Operative Technique
For my patients, this means that the procedure will be done as an outpatient in my accredited office surgical suite or a hospital or other outpatient surgical facility. It will be done under intravenous sedation and local anesthesia or general anesthesia.2 The breast implant will be placed through an inframammary crease incision in the subpectoral plane with adequate release of the pectoralis major muscle out of the lower pole of the breast.3–5 The width (and therefore part of the determinate of the volume) of the implant will be determined by the width of the breast. The inframammary crease level will be adjusted if the distance from the nipple to the medial edge of the breast (under no tension) doesn’t match the distance from the nipple to the existing inframammary crease (under tension).
The patient gets to choose the surgeon, the facility, the method of anesthesia, whether the implant is saline-filled or gel-filled, and the profile of the implant (Table 22.2).
| Today, the patient gets to choose whether she wants a saline-filled or gel-filled breast implant device. |
| With experience and proper attention to detail, saline-filled breast implants can be made to look just like a gel-filled implant. |
| Palpable feel of the saline-filled implant, ‘rippling’ that is felt and not seen in the upright position, cannot be avoided with a saline-filled device but can be graded and predicted at least for the immediate postoperative period. |
| Comparing the choice of saline-filled to gel-filled implants should not be described as which one is ‘better’, but should be discussed as what are the advantages and disadvantages of each and how important those factors are to the patient. |
| Gel-filled breast implants have one major advantage: |
| They feel more natural regardless of coverage. |
| And one major disadvantage: |
| There is no simple way to verify integrity. |
| Saline-filled breast implants have several minor advantages: |
Anesthesia options
Most breast surgery today is still done under general anesthesia and this is quite acceptable and reasonable. This requires the services of an anesthesiologist or anesthetist and adds a significant component to postoperative treatment of pain, nausea, and vomiting. These problems are minimized by intravenous sedation and long acting local anesthetics but many methods are available today to deal with postoperative nausea and vomiting.4
Dissection of the pocket
The incision is carried directly down through the superficial fascial layer and through the fascia overlying or extending from the pectoralis major muscle. This fascia must be released along the level of the old or new IMC (one of the dual planes described by Tebbetts),3–5 and access can be gained to the relatively free subpectoral plane with minor origins of the pectoralis released but not beyond the medial border and not beyond the lower pole up to about the 3:30 to 4 o’clock position (if the patient’s right breast is viewed as a clock).
Hemostasis and irrigation
Hemostasis is critical. Local anesthetics with epinephrine can potentially mask this and operative drains are not generally worth the drawbacks unless hemostasis cannot be assured. Irrigation with plain saline and antimicrobial solutions until clear should confirm this. The ‘no-touch’ technique6 is utilized when handling the implant. The operative gloves are washed off or changed and then washed off and only the operative surgeon minimally touches the implant until it is bathed in antimicrobial solution. The filling tube is then placed and the air carefully sucked out. The implant can then be rolled up to allow it to pass through a 2 cm incision with the fill tube in place.
IMC fixation
Whether or not the IMC was moved downward to accommodate the diameter of the round implant, it is desirable to make sure the lower side of the IMC incision is fixed to the chest wall7. This can be accomplished using 2-0 or 3-0 absorbable sutures by suturing the superficial fascia and lower dermis to the fascia over the ribs of the chest wall. This is reinforced by the elastic strap of the brassiere during the postoperative recovery. The incision is closed first at the superficial fascial level from the upper side to the already sutured down lower side and then at the dermal level. Incisional tape is used to seal the skin level.
Pitfalls and How to Correct
IMC stretch/deformity
The IMC may be left in position if the position is correct for a round implant to be properly positioned. It must be lowered if the vertical radius of the implant compared to the medial radius requires it. This must be done deliberately and then the new IMC position controlled during the healing process. Experience with breast reconstruction and procedures such as the Ryan flap7 advancement approach to the IMC suggest that the IMC can be controlled by suturing the flap of skin/fat/fascia below an IMC incision to the chest wall and using an elastic strap to help it heal there.
Postoperative Care
Saline-filled implant deflations are easy to detect and replacement scheduling can often be initiated over the phone with a preoperative check to verify and discuss the options of simple replacement or replacement of both sides either of which are not overly complicated with a pre-existing IMC incision (Figs 22.5–22.7).
1 Deapen D. Breast implants and breast cancer: a review of incidence, detection, mortality, and survival. Plast Reconstr Surg. 2007;120(7 Suppl 1):70S-80S.
2 Cooter RD, Rudkin GE, Gardiner SE. Day case breast augmentation under paravertebral blockade: a prospective study of 100 consecutive patients. Aesth Plast Surg. 2007;31(6):666-673.
3 Tebbetts JB. Achieving a predictable 24-hour return to normal activities after breast augmentation: part I. Refining practices by using motion and time study principles. Plast Reconstr Surg. 2002;109(1):273-290.
4 Tebbetts JB. Achieving a predictable 24-hour return to normal activities after breast augmentation: Part II. Patient preparation, refined surgical techniques, and instrumentation. Plast Reconstr Surg. 2002;109(1):293-305.
5 Tebbetts JB. Dual plane breast augmentation: optimizing implant-soft-tissue relationships in a wide range of breast types. Plast Reconstr Surg. 2006;118(7 Suppl):81S-98S.
6 Mladick RA. ‘No-touch’ submuscular saline breast augmentation technique. Aesth Plast Surg. 1993;17(3):183-192.
7 Ryan JJ. A lower thoracic advancement flap in breast reconstruction after mastectomy. Plast Reconstr Surg. 1982;70(2):153-160.