Rotation Flaps
Introduction
Although rotation flaps are pivotal flaps in their movement, most are also advanced by stretching of the flap. Depending on the degree of stretching, the vector of greatest wound closure tension may be along a line extending from the base to the apex of the distal flap. When no advancement is used in movement of rotation flaps, the greatest wound closure tension is perpendicular across the distal border of the flap, not across the long length of the flap.1,2
Studies by Larrabee and Galt have demonstrated minimal benefit at the defect site of extending the arc of rotation flaps beyond 90° from the axis of the defect.2 This is to say, wound closure tension is not reduced at the defect site by increasing the pivotal movement of the flap by more than 90° from the axis of the defect. However, there is often some benefit in extending the incision to accommodate redraping of skin.
The secondary defect created by rotation flaps represents a transformation and a translocation of the primary defect.3 The surface area encompassed by the primary defect is equivalent to the surface area of the secondary defect.3 The geometry of the secondary defect is determined by the size of the flap. The larger the flap, the longer and narrower is the secondary defect. The narrower the width of the secondary defect, the less is the tension required to close the wound and the less is the secondary movement of tissue adjacent to the donor site. Another way of stating this is that the greater the length of the arc and thus the larger the flap, the less is the wound closure tension across the repair of the secondary defect.
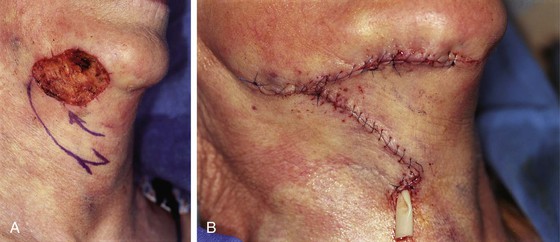
Rotation flaps are best suited for repair of defects that are triangular. Design of the classic rotation flap is seen in Figure 7-1. A standing cutaneous deformity will develop at the base of the flap. A Burow triangle can be removed to facilitate repair of the donor site wound. A back cut4 at the base of the flap shifts the position of the pivotal point and changes the location of the standing cutaneous deformity.5–7 When a rotation flap is converted to a two-dimensional form, it appears as in Figure 7-2. As can be seen in the illustration, a problem encountered with rotation flaps is the unequal length of the flap’s border, labeled B in the drawing, compared with the width of the primary and secondary defects, labeled A in the drawing. A common method to equalize this discrepancy is to excise an equalizing Burow triangle at some point along the periphery of the curvilinear incision. The triangle’s base is equal in width to the width of the base of the defect, labeled C in Figure 7-2. Excision of the triangle of skin results in equalizing of the length of the two sides of the incision. An alternative solution to the management of the discrepancy in length of wound margins is to modify the movement of the flap from one that is purely pivotal to one that is both pivotal and advancement. By advancing the flap while at the same time rotating it around its pivotal point, the flap is stretched to equalize the discrepancy (Fig. 7-3). In so doing, the surgeon takes advantage of the distensibility (Fig. 7-4, side B) and the compressibility (Fig. 7-4, side A) of the skin along the wound margins. Repair is then accomplished by use of the principle of halving by suturing on the bias (Fig. 7-4C, D). This is accomplished by placing a suture to appose the two borders of the wound at the halfway point along the length of the flap. Succeeding sutures are placed in a manner that continues to equally divide the remaining distances along the flap’s border. An experienced surgeon will learn to suture on the bias from one end of the flap to the other without resorting to planned halving sutures.
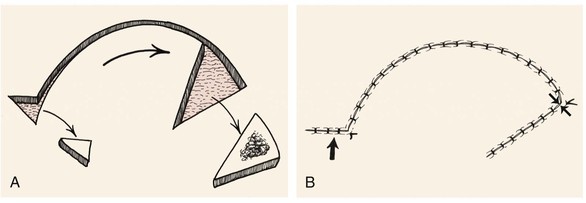
FIGURE 7-1 A, Rotation flap with excision of an equalizing Burow triangle. B, Opposing arrows indicate point of greatest wound closure tension. Large arrow indicates closure site of the equalizing Burow triangle excision.
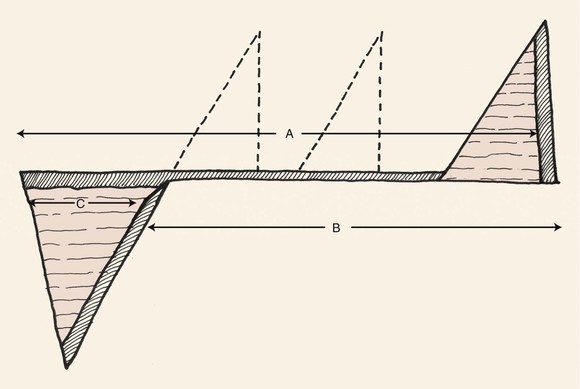
FIGURE 7-2 Rotation flap converted to two-dimensional form. Discrepancy between border of rotation flap (side B) and width of primary and secondary defects (side A) is equalized by excision of a triangle of skin (Burow triangle) at some point along curvilinear periphery of incision (side A) with base equal in width to maximum width of defect (side C).
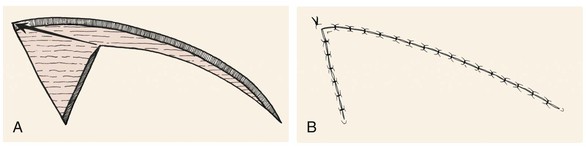
FIGURE 7-3 A, B, Need for excision of a Burow triangle is often avoided by advancement of distal tip of rotation flap and repair of wound by suturing on bias.
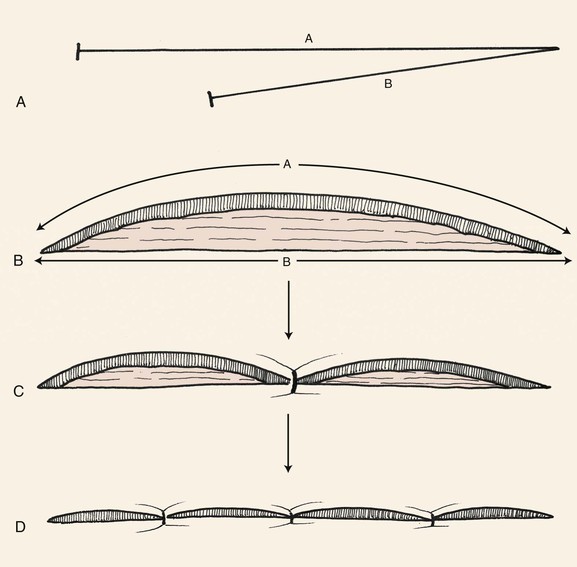
FIGURE 7-4 A, B, Surgeons take advantage of distensibility of side B and compressibility of side A to achieve wound closure without excision of an equalizing Burow triangle by advancing and stretching side B to reach most distal border of defect. C, D, Wound is repaired by principle of halving sutures.
As a general rule, in designing rotation flaps on the face, the length of the flap (Fig. 7-2, side B) should be four times the width of the base of the triangular defect (Fig. 7-2, side C). When this ratio is used, excision of an equalizing Burow triangle is usually not required. Undermining of the base of the flap along with its pivotal point enables advancement of the flap toward the defect during wound closure. Advancement reduces wound closure tension and often necessitates a smaller flap with less movement about its pivotal point than when the flap’s pedicle is not widely undermined and advanced. In addition to reducing the overall size of the flap, undermining limits the development of a standing cutaneous deformity by advancing a portion of the deformity peripherally away from the flap’s base.
Increasing the degree of undermining of the flap without lengthening the border of the flap does not significantly decrease wound closure tension. Likewise, enlarging the flap beyond the length of four times the width of the defect does not significantly decrease wound closure tension.8 When a single flap is used for wound repair, the arc of the flap may be adjusted for a number of considerations. For instance, the arc of the flap may be shortened to maintain the incision along or inside hair-bearing tissue. The arc may be extended more than four times the width of the defect when the defect is located in areas of limited skin mobility.
To avoid a standing cutaneous deformity at the base of a rotation flap used to repair a defect, the defect should ideally assume the configuration of an inverted triangle. The triangle should have the height-to-width proportion of 2 : 1 (Fig. 7-5). In addition, if the arc of rotation of the flap is to be a completely symmetric curve, the height of the triangular defect should be 0.5 to 1 times the radius of the curve of the flap (Fig. 7-6). To create the ideal condition for use of a rotation flap, the defect can be enlarged by removing normal tissue and converting the defect into a triangle with a height-to-width ratio of 2 : 1 (Fig. 7-7).9
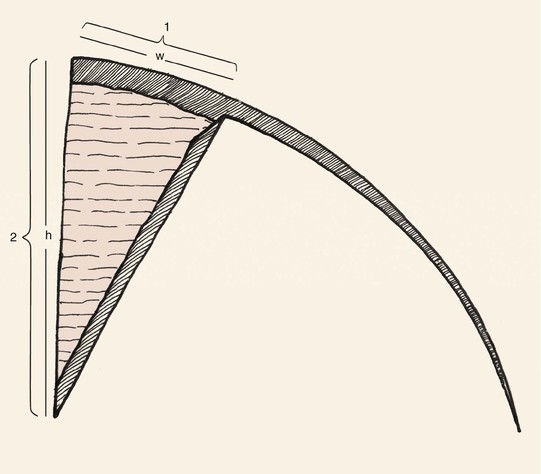
FIGURE 7-5 To minimize standing cutaneous deformity that develops at base of rotation flap, most ideal configuration of triangular defect has height-to-width ratio of 2 : 1.
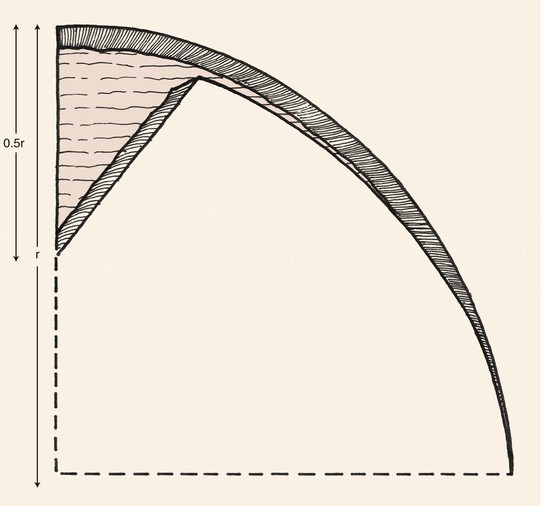
FIGURE 7-6 For symmetric rotation flap, height of triangular defect should be 0.5 to 1 times the radius of curvature of flap’s border.
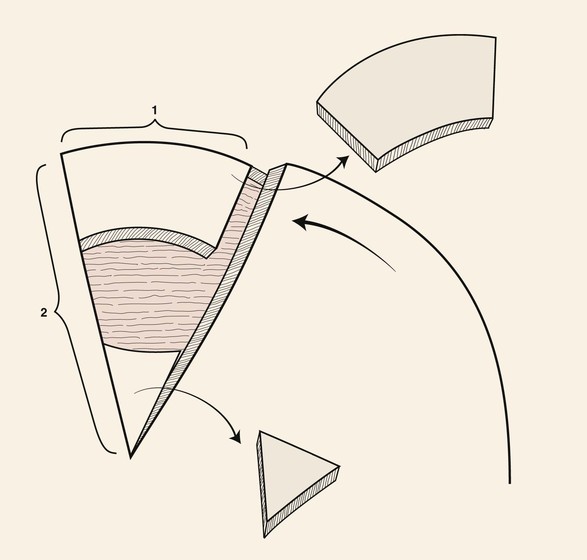
FIGURE 7-7 To create ideal condition for use of rotation flap, defect enlarged by removing normal tissue and converting defect into triangle with height-to-width ratio of 2 : 1.
There are several advantages of using rotation flaps. The flap has only two sides; as a result, the surgeon can sometimes position the arced incision in an aesthetic border. The flap is broad based, and therefore its vascularity tends to be reliable. There is great flexibility in design and positioning of the flap.10–12 Design of inferiorly based rotation flaps promotes lymphatic drainage and reduces flap congestion and edema. Similarly, arterial and venous disruptions may be minimized and sensory innervation may be maximized by appropriately positioning the base of the flap.
Rotation flaps should not be selected as a first option in situations in which design of the flap will necessitate placement of incisions that cross RSTLs or aesthetic borders at right angles. This will likely result in an inadequately camouflaged scar along a portion of the donor site. Rotation flaps are not a good choice to repair central upper cheek skin defects in men because hair-bearing skin of the sideburn is moved medially into the non–hair-bearing area of the cheek covering the malar eminence. Except for the dorsal nasal flap, rotation flaps are not often used in repair of nasal defects because donor site scars do not follow the boundaries separating the nasal aesthetic units. The skin of the nasal tip is inelastic, making the use of rotation flaps difficult. Small defects over the dorsum of the nose are best repaired with transposition flaps, such as a bilobe or rhombic flap. Furthermore, rotation flaps transferred from the cheek to the sidewall of the nose usually have an unacceptable result because of the necessary bridging of the flap across the nasofacial sulcus. This partially obliterates this important landmark. Similarly, rotation flaps from the cheek are inappropriate for reconstruction of lateral lip defects because the arc of the flap must extend across the melolabial fold and crease at right angles. The melolabial crease is a prominent aesthetic border, and incisions crossing it perpendicularly often create unsightly scars.
Applications
Scalp
Rotation flaps are the preferred method to repair most scalp defects with use of local tissue. Because of its spherical topography, the scalp accommodates curvilinear incisions well and the flaps can be constructed sufficiently large without the need to regard RSTLs or aesthetic borders. Rotation flaps are transferred by a pivotal motion rather than depending on stretching of tissue for movement as required by advancement flaps. Because of the inelasticity of scalp tissue, any movement of tissue by advancement is limited. Whenever possible, multiple rotation flaps are preferred to the use of a single flap for scalp reconstruction. Each flap is designed to pivot on an independent pivotal point. When two rotation flaps are used, the flaps may be designed to pivot in opposite directions, creating a T configuration of the wound repair. Most defects left after micrographic surgery are round or oval. When this configuration is present, it is best to use two flaps that pivot in the same direction, either clockwise or counterclockwise. Each flap is designed with an opposite orientation on either side of the defect. The two flaps are apposed with a Z-shaped repair. This type of repair is known as an O-Z repair. In designing a double rotation flap in an O-Z pattern, the optimum design for wound closure is an acute-angled flap with a length equal to four times the radius of the defect being closed. Use of more than one rotation flap is advantageous because it recruits scalp tissue for reconstruction from different locations and the burden of closing the secondary defect is shared by the number of flaps used. Two or three rotation flaps work best for reconstruction of scalp defects. When three flaps are used, each is responsible for repair of one-third of the surface area of the defect. Wound closure is accomplished by pivoting all three flaps in the same direction. Repair of the defect has the appearance of a pinwheel, and wound closure configuration resembles the closing of a camera lens.13
Face
Rotation flaps work extremely well in repair of cheek defects larger than 3 or 4 cm in the lower preauricular area, where recruitment of the upper posterior cervical skin is required for wound closure. The curvilinear incision is positioned juxtaposed to the earlobe and along the hairline of the postauricular scalp. If necessary, the incision extends along the border of the trapezius muscle. An incision in this area of the neck produces a favorable scar even though it does not follow RSTLs. A Z-plasty at the base of the flap often facilitates closure of the secondary defect without the need for excision of an equalizing (Burow) triangle. In cases in which patients use tobacco or have been irradiated in the region of the defect, cervical rotation flaps may be elevated beneath the superficial fascia and the platysmal muscle. This will enhance the vascularity of the flap.14
Nose: Dorsal Nasal Flap
The dorsal nasal flap is a modified rotation flap that recruits redundant skin from the glabella. The flap can be used to repair skin defects of the nasal tip, dorsum, and sidewall. Elliott15 detailed the banner and bilobe flaps for nasal repair, designing them as interpolated flaps that require inset. Rieger16 described the basic design of the dorsal nasal flap used currently. The flap uses the entire dorsal nasal skin to facilitate repair. Further refinements of the flap were offered by Rigg,17 who introduced the concept of limiting the area of nasal skin used for construction of the flap. He advocated a back cut of the flap toward the medial canthus. Marchac and Toth18 designed the flap with an axial vascular pattern by incorporating a constant branch of the angular artery in the pedicle. This enabled a longer descent of the glabellar back cut to the level of the medial canthus. The greater back cut facilitates flap transfer, reducing wound closure tension and distortion of the nostril margin.
The dorsal nasal flap enables the surgeon to repair caudal and midnasal defects measuring 2.5 cm in diameter or less with matching adjacent tissue. There is insufficient nasal skin to repair larger defects in this manner. The flap is ideally suited for elderly patients with skin defects located centrally on the tip. By necessity, the flap is designed with a large surface area to maximize tissue movement and to decrease wound closure tension at the donor site. Excessive cephalic rotation of the nasal tip and alae is prevented by the large size of the flap, which incorporates the majority of the remaining nasal skin. It is imperative to assess nasal skin laxity when use of the flap is being considered and to plan for some degree of secondary movement at the margins of the nasal alae and tip. Skin laxity in the glabella and dorsal nasal regions is best determined by the “pinch test.” This test consists of grasping the skin between the surgeon’s thumb and index finger and determining the degree of redundancy.19 For success, sufficient skin laxity is present when the surgeon can gather 1 or 2 cm of skin on the nasal bridge and glabella. Greater laxity is necessary as the size of the defect increases.
Commonly, the dorsal nasal flap is designed as a laterally based rotation flap with a back cut (Fig. 7-8). The pedicle is centered in the region of the medial canthus. A curvilinear line is drawn laterally from the defect to the junction of the cheek and the nose. From this point, the line is directed superiorly, passing 0.5 cm medial to the medial canthus and extending to the superior aspect of the glabella within a glabellar crease. Because the flap is transferred primarily by pivoting, the effective length of the flap diminishes progressively as the flap rotates about its pivotal point (medial canthus). The height of the flap and thus the arc of pivotal movement must be sufficient to compensate for this shortening. Supplemental flap height is gained from the glabellar extension. The higher the extension, the greater the height of the flap, and the easier it will be to close the primary defect. From the nasofrontal angle, the glabellar extension is approximately  to 2 times the vertical height of the nasal defect. From the superior point of the glabellar extension, a line angles inferiorly toward the contralateral medial canthus, creating a 30° to 45° angle back cut. The back cut remains just superior to the level of the medial canthal tendon to protect the axial vessels from the angular artery located inferior to the tendon. In designing the flap, it is helpful to triangulate the defect by excising the standing cutaneous deformity in such a manner that the excision lays within the alar groove or above and parallel to it. Incisions for the flap should not extend below the alar groove or obliteration of the concave topography will occur between the ala and the nasal sidewall.
to 2 times the vertical height of the nasal defect. From the superior point of the glabellar extension, a line angles inferiorly toward the contralateral medial canthus, creating a 30° to 45° angle back cut. The back cut remains just superior to the level of the medial canthal tendon to protect the axial vessels from the angular artery located inferior to the tendon. In designing the flap, it is helpful to triangulate the defect by excising the standing cutaneous deformity in such a manner that the excision lays within the alar groove or above and parallel to it. Incisions for the flap should not extend below the alar groove or obliteration of the concave topography will occur between the ala and the nasal sidewall.

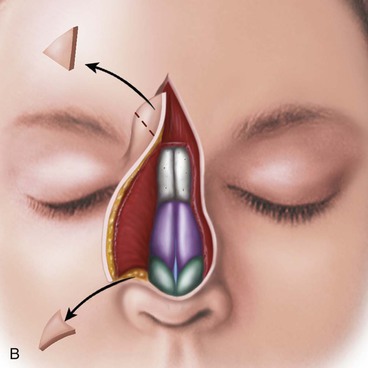
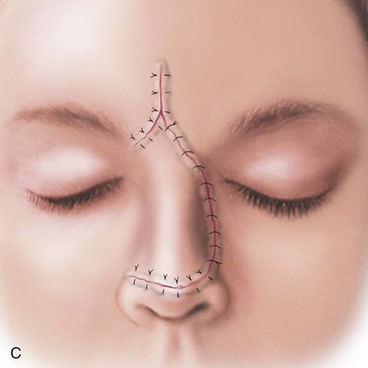
FIGURE 7-8 A, Dorsal nasal flap is a modified rotation flap based on branches of angular artery. Glabellar portion (shaded) dissected in subcutaneous tissue plane. B, Nasal portion dissected beneath nasal musculature. Standing cutaneous deformity excised in or parallel to alar groove. C, Glabellar donor site wound closed in V-Y configuration. (From Baker SR: Nasal cutaneous flaps. In Baker SR, editor: Principles of nasal reconstruction, ed 2, New York, Springer, 2011.)
I occasionally use a modified design of the dorsal nasal flap for midline skin defects of the upper dorsum (Fig. 7-9). The design is such that the lateral border of the flap remains anterior to the thin skin of the medial canthal region to avoid mismatch in skin thickness. I call this design a dorsal heminasal flap. The design limits the arc of tissue movement; the modified flap can be used only for smaller (less than 2 cm) skin defects of the nasal bridge that are at least 1 cm cephalic to the nostril margin and not inferior to the tip-defining points.19 The dorsal heminasal flap does not necessarily require a glabellar incision. The lateral incision is along the junction of the nasal sidewall and dorsum and therefore recruits skin only from the nasal bridge.
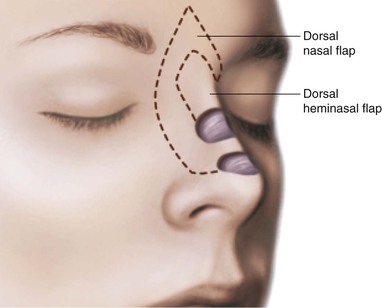
FIGURE 7-9 Dorsal nasal and heminasal flaps. The heminasal flap is used to repair more cephalic skin defects. Its borders remain anterior to thin skin of medial canthal region. (From Baker SR: Nasal cutaneous flaps. In Baker SR, editor: Principles of nasal reconstruction, ed 2, New York, Springer, 2011.)
Reduction rhinoplasty may occasionally facilitate repair of a nasal skin defect by creating a relatively greater amount of skin redundancy. The patient in Figure 7-10 presented with a 3 × 2-cm skin defect of the upper dorsum and a marked convexity and overprojection of the upper and middle nasal vaults.20 She desired a reduction of the nasal bridge. An aesthetic rhinoplasty was performed concomitant with a modified dorsal nasal flap. Reducing the volume of the bony and cartilaginous nasal skeleton created greater skin redundancy, which enabled partial wound closure by advancement of nasal skin medially. This in turn reduced the size requirement of a modified dorsal nasal flap used to repair the remaining portion of the defect. The standing cutaneous deformity resulting from bilateral medial advancement of the nasal sidewall skin was excised in the midline immediately inferior to the caudal border of the skin defect.

FIGURE 7-10 A, A 3 × 2-cm skin defect of nasal dorsum. B, Reduction of nasal bridge projection created relatively greater amount of skin redundancy. Defect partially closed by medial advancement of nasal skin. Modified dorsal nasal flap designed to repair remaining portion of defect. C, Flap in position. Standing cutaneous deformity resulting from medial advancement of nasal sidewall skin excised in midline, immediately inferior to caudal border of transferred flap. D-G, Preoperative views before removal of skin cancer and postoperative views 10 months after surgery. No revision surgery performed. (From Johnson TM, Swanson NA, Baker SR, et al: The Reiger flap for nasal reconstruction. Arch Otolaryngol Head Neck Surg 121:634-637, 1995.)
Surgical Technique
Preparation of the patient for surgery and preoperative and postoperative care are discussed in detail in Chapter 5. All facial reconstruction using rotation flaps is performed as an ambulatory surgical procedure. In the majority of cases, monitored anesthesia consisting of intravenous administration of midazolam and fentanyl is used. Rotation flaps of the face are usually designed so that they are inferiorly and medially based. The border of the flap is positioned in an aesthetic border when possible and in RSTLs when an aesthetic border is not in the immediate vicinity of the defect. On occasion, additional skin is removed adjacent to the defect so that the margin of the flap can be positioned along such borders.
The entire face is then prepared and draped. A skin marking pen is used to design the flap and to mark areas adjacent to the defect that will require excision. When micrographic excision has been used to remove a skin tumor, the entire margin of the defect is excised with incisions perpendicular to the skin margin. Additional skin in the vicinity of the defect is usually excised to create a triangular defect that will allow movement of the flap into position. Depending on the size and location of the defect, skin may also be excised to enable the flap to extend to adjacent aesthetic borders or RSTLs. All of these excisions are made before the flap is dissected. All incisions are vertical to the surface of the skin with no beveling. The borders of the flap are incised, and the flap is then sharply undermined in the subcutaneous plane. In addition, all sides of the donor defect are undermined for a distance of at least 2 cm. An exception to this rule is when borders of the donor site are relatively fixed, such as the melolabial fold, alar-facial sulcus, or eyelid. These areas are undermined 4 or 5 mm so that wound edge eversion can occur, but without distortion of adjacent facial structures. All undermining is accomplished with sharp dissection in the subdermal plane. Hemostasis is established with monopolar electrocautery.
Patients having large rotation flaps should be checked within 24 hours after surgery to ensure that no hematoma has formed beneath the flap or at the donor site. Patients are instructed to avoid strenuous exercise for 2 weeks after surgery and are asked to avoid sun and extreme temperature exposures for at least 1 month postoperatively. Suture removal should be accomplished in 5 to 7 days after facial flaps and 10 to 14 days after cervical and scalp flaps. Facial scars resulting from repair with rotation flaps can often be improved in appearance with dermabrasion. Dermabrasion is usually accomplished 6 weeks after the initial surgery. Because of the curvilinear configuration of rotation flaps, trap-door deformity may occur. Injection of the affected area with triamcinolone 10 mg/mL in the deep subcutaneous tissue will often accelerate resolution of the deformity. Physical massage of the flap beginning 4 weeks postoperatively will assist in reducing postoperative edema. Surgical revision of the flap or scars should not be entertained for 9 to 12 months after the initial flap transfer.
Case Reports
Case 1
A 3-year-old girl suffered a third-degree burn injury to the left parietal scalp, resulting in permanent alopecia measuring 10 × 4-cm (Fig. 7-11). The options for correction of the alopecia included hair transplantation and excision with reconstruction by a scalp flap. It was elected to perform a serial excision of the affected area. Because of the lateral location of the alopecia, only a single large rotation flap could be effectively transferred to cover the proposed resection of the scarred scalp. Therefore, the majority of the remaining hair-bearing scalp was included in a large rotation flap designed so that it was based posteriorly and laterally on the occipital and postauricular arteries. The perimeter of the arc of the flap was five times the width of the portion of scalp planned for resection. A single back cut at the base of the flap was incorporated into the design to reduce wound closure tension. The flap was elevated in the subgaleal tissue plane, and the remaining scalp and all of the forehead skin were undermined in a similar plane to reduce wound closure tension (Fig. 7-12). The area of scalp involved with alopecia and planned for resection was not removed until the rotation flap was pivoted and the donor site for the flap closed. The portion of scarred scalp that was covered by the rotation flap was then resected and the wound repaired after placement of a Penrose drain beneath the scalp flap. Approximately 90% of the area of alopecia was excised in a one-stage procedure by this approach (see Fig. 7-12).

FIGURE 7-11 A, A 10 × 4-cm area of alopecia from burn injury of scalp. B, Large rotation scalp flap with back cut designed to repair anticipated defect after excision of scarred scalp.
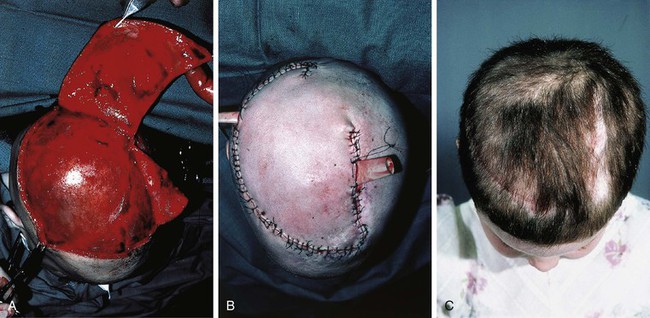
FIGURE 7-12 Same patient shown in Figure 7-11. A, Flap elevated in subgaleal tissue plane. B, Area of alopecia excised and flap transferred. C, Postoperative view at 2 months.
Case 2
Figure 7-13 shows a circular defect 5 cm in diameter resulting from micrographic excision of a basal cell carcinoma involving the anterior parietal and frontal scalp. The defect included loss of the periosteum of the skull in the depths of the wound. This defect could have been repaired with a single rotation scalp flap. However, whenever possible, multiple rotation flaps are preferred to a single flap for scalp reconstruction. Each flap is designed to pivot on an independent pivotal point. An O-Z repair was elected for reconstruction of the defect. The two flaps were laterally based and designed with an opposite orientation so that they wound pivot in a clockwise direction. Each flap was designed with an acute angle and with a length equal to four times the radius of the defect.

FIGURE 7-13 A, A 5-cm circular full-thickness scalp defect. Dotted lines indicate incision line for rotation flaps. B, Each flap pivoted in clockwise direction for O-Z wound closure. C, Postoperative view at 6 months.
Use of more than one rotation flap for reconstruction of the scalp is advantageous because it recruits scalp tissue for reconstruction from different locations and the burden of closing the secondary defect is shared by the number of flaps used. This concept was applied to the repair of the patient shown in Figure 7-14. This patient presented with a circular defect 9 cm in diameter in the same location as that of the patient shown in Figure 7-13. Because the defect was considerably larger, three rotation scalp flaps were designed to repair the defect rather than using an O-Z repair. Each flap was responsible for repair of one-third of the surface area of the defect. Wound closure was accomplished by pivoting all three flaps in the same direction and resembled the closing of a camera lens; the final suture line had the appearance of a pinwheel.
Case 3
A 48-year-old woman developed a recurrent basal cell carcinoma of the right temple. It had been treated twice in the past but had recurred. The tumor was resected by micrographic surgery, and she presented with a 4 × 3-cm skin defect of the right lateral eyebrow and forehead (Fig. 7-15). The two preferred options for repair of this large defect were a full-thickness skin graft and a local flap harvested from the adjacent temple skin. Because of the large size of the defect, the donor site of any local flap using skin from the central forehead would be difficult to close primarily. That option would also create a scar located more centrally on the face. A large rotation skin flap from the temple was selected for repair. This flap was selected because of the circular configuration of the defect and the possibility of incorporating both pivot and advancement in the tissue movement of the flap. By undermining laterally as far as the skin overlying the malar eminence, considerable advancement of the skin could be added to the pivotal movement of the flap, thus reducing wound closure tension. The majority of the donor site scar could also be aligned within the horizontal creases of the forehead.

FIGURE 7-15 A, A 4 × 3-cm skin defect of forehead including eyebrow. Rotation flap designed for repair. B, Flap incised. Standing cutaneous deformity excised laterally along bony orbital rim. C, Flap in place.
The flap was elevated in the subcutaneous tissue plane to avoid injury to the temporal branch of the facial nerve. The standing cutaneous deformity was excised parallel to the superior bony orbital rim just lateral to the defect, curving slightly toward the lateral canthus. Figure 7-16 shows the appearance of the forehead 1 year later. The medial portion of the scar resulting from the repair is slightly depressed and is diagonal to the horizontal creases of the forehead. The lateral portion of the scar is barely visible because it is located in RSTLs.

FIGURE 7-16 A, B, Same patient shown in Figure 7-15. Postoperative view at 1 year. No revision surgery performed.
Case 4
A 65-year-old woman underwent resection of a superficial melanoma of the right cheek resulting in an irregularly shaped 6 × 5-cm skin defect of the malar eminence (Fig. 7-17). Reconstruction options for repair of the defect included a full-thickness skin graft, unipedicle advancement flap, transposition or bilobe flap, and rotation cheek flap. Although a large superiorly and laterally based transposition flap could have effectively reconstructed this defect, a rotation flap with a small back cut was selected for repair. The flap was designed to recruit skin from the lateral cheek and upper cervical region. The anticipated standing cutaneous deformity was marked with horizontal lines (Fig. 7-17A). The flap was dissected in the subcutaneous tissue plane to protect the facial nerve branches to the orbicularis oculi and frontalis muscle. The defect was lateral to the lower eyelid, so it was not necessary to arch the border of the flap above the level of the lateral canthus. When the skin defect is more medial adjacent to the lower eyelid, it is advisable to extend the arc of the rotation flap above the level of the lateral canthus when designing the flap. This will give added height to the flap, which in turn will reduce wound closure tension in the area of the eyelid skin. The incision for the flap extended to the auricle in RSTLs and tucked beneath the earlobe, a structure that assisted in hiding a portion of the donor site scar. It was necessary to extend the incision for the flap along the border of the sternocleidomastoid muscle.

FIGURE 7-17 A, A 6 × 5-cm skin defect of cheek in area of malar eminence. Rotation flap designed for repair. Anticipated standing cutaneous deformity marked by horizontal lines. B, Flap in place. C, D, Postoperative views at 2 years. No revision surgery performed.
Figure 7-18 shows a smaller skin defect (3 × 2-cm) in a location similar to that of the previous case; however, a portion of the lower eyelid skin was involved with the defect. A rotation skin flap was designed to repair the defect. The arc of the border of the flap was designed to extend well above the level of the eyelid defect to accommodate the reduction in effective length of the flap as it pivoted around its base. This ensured that the flap would have sufficient height to reach the superior and medial borders of the eyelid defect without placing excessive wound closure tension along the suture line of the eyelid repair. A deep suture of 4-0 polypropylene was used to anchor the border of the flap to the periosteum of the lateral bony orbital rim superior to the lateral canthus to fix the flap in position and to reduce wound closure tension along the inferior eyelid. The standing cutaneous deformity was excised lateral to the defect parallel to RSTLs.

FIGURE 7-18 A, A 3 × 2-cm skin defect of malar eminence and lateral lower eyelid. Rotation flap designed with arc of flap extending above level of lateral canthus to accommodate reduction in effective height of flap as flap pivots and to minimize wound closure tension along eyelid suture line. B, Flap in place. Buried suspension suture placed in periosteum of lateral orbital bony rim. C, Postoperative view at 6 months. No revision surgery performed.
Rotation flaps can be used anywhere on the face; however, they look best when they are designed so that the resulting scar is in or approximates the location of RSTLs of the face or lie along borders of facial aesthetic regions. Defects larger than 3 cm located on the medial cheek or over the malar eminence may require sizeable rotation flaps. This necessitates extensive dissection and a potentially greater raw surface area for bleeding to occur than when comparable defects are repaired with transposition flaps (Fig. 7-19). More important, rotation flaps used to repair superior medial cheek defects require incisions perpendicular to RSTLs of the upper cheek. This often results in unsightly scars. For this reason, I favor transposition flaps over rotation flaps for medially located cheek defects. However, rotation flaps work extremely well for repair of skin defects in the range of 3 to 6 cm located in the preauricular region, where superior and posterior cervical skin can be recruited into the flap (Fig. 7-20). The patient shown in Figure 7-21 had a squamous cell carcinoma of the skin that was removed, creating a 6 × 6-cm skin defect. A large cervicofacial rotation flap was designed so that the upper posterior neck skin could be pivoted and advanced toward the defect. The curvilinear incision was placed juxtaposed to the earlobe and along the anterior border of the trapezius muscle near the hairline. An incision in this area of the neck often produces a favorable scar even though it does not follow RSTLs. A Z-plasty at the base of the flap facilitated closure of the secondary defect without the need for excision of a Burow triangle.

FIGURE 7-19 A, Melanoma in situ marked by horizontal lines for excision. Rotation flap designed for repair. Anticipated standing cutaneous deformity (SCD) marked by vertical lines. B, Skin lesion excised. Rotation flap reflected downward to expose large raw surface area. C, Flap pivoted toward recipient site. D, E, Standing cutaneous deformity forms at base of flap and requires excision. F, G, Postoperative views at 2 years. Scar is perpendicular to RSTLs, causing an unsightly appearance.

FIGURE 7-20 A, A 3.5 × 2-cm preauricular skin defect. Rotation flap with Z-plasty designed for repair. Anticipated standing cutaneous deformity (SCD) marked for excision. B, Flap in place. C, D, Preoperative and 2-month postoperative views. No revision surgery performed.
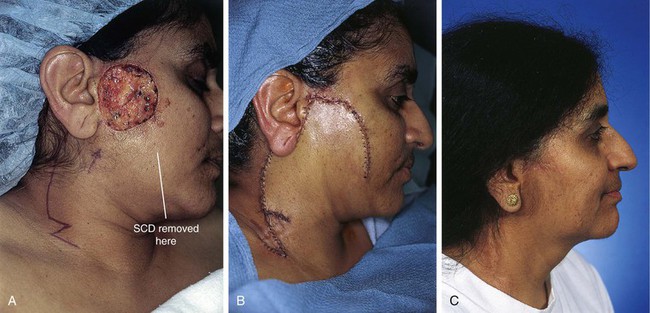
FIGURE 7-21 A, A 6 × 6-cm skin defect of posterior cheek. Large cervical rotation flap designed. Z-plasty at base of flap eliminates need to excise an equalizing Burow triangle. Standing cutaneous deformity (SCD) excised from inferior medial aspect of defect. B, Flap in place. SCD removed. C, Postoperative view at 1 year. (From Baker SR: Local cutaneous flaps. Otolaryngol Clin North Am 27:139, 1994.)
Case 5
Rotation flaps are a useful method of repairing defects involving neck skin because of the redundancy of cervical skin relative to the face. In addition, the importance of placing incisions in RSTLs is less in the neck compared with the face. This is because cervical incisions perpendicular to RSTLs can be partially hidden by clothing and tend not to form hypertrophic or depressed scars compared with similar incisions on the face. Figure 7-22 shows a 10 × 7-cm skin defect of the inferior cheek and upper neck after removal of a basal cell carcinoma in a 65-year-old woman. Lax skin of the neck provides an excellent source for creating skin flaps with advancement, transposition, rotation, or a combination of these flap designs. In this case, a large rotation flap based medially was used to repair the defect. The flap was dissected in the subcutaneous tissue plane, and the standing cutaneous deformity was excised at the medial border of the defect with a horizontal orientation so the resulting scar would remain parallel to the body of the mandible. A Z-plasty was designed at the base of the flap to reduce the need for excision of a Burow triangle along the peripheral border of the wound. However, it was not necessary to implement the Z-plasty as the discrepancy of border lengths between the flap and the remaining cervical skin was sewn out by use of the principle of suture halving. This technique is discussed in an earlier portion of the chapter. In contrast, Figure 7-23 shows a defect of the chin and submental skin repaired with a much smaller rotation flap. In spite of a Z-plasty at the base of the flap, it was necessary to excise a sizeable equalizing Burow triangle along the border of the flap. The wound closure of this excision is represented by the extension of the suture line medially from the flap. Because the rotation flap had a shorter border length compared with the flap design in Figure 7-22, there was less wound margin available to equalize the discrepancy in lengths of the wounds by the principle of suture halving.
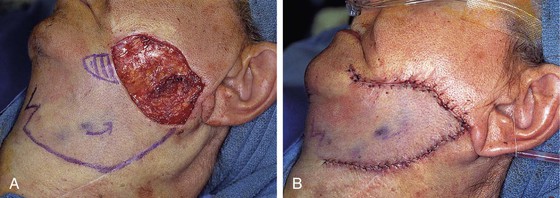
FIGURE 7-22 A, A 10 × 7-cm skin defect of cheek and neck. Rotation flap designed for repair. Vertical lines represent anticipated standing cutaneous deformity as flap pivots. B, Flap in place. Z-plasty at base of flap not necessary to correct discrepancy of wound border lengths.

FIGURE 7-23 A, A 3 × 2.8-cm skin defect of chin and neck. Rotation flap with Z-plasty at base of flap designed for repair. Dotted line represents location of an equalizing Burow triangle excision. B, Flap in place.
Figure 7-24 shows a superior neck skin defect repaired with a rotation flap. As in the previous two flaps discussed, a Z-plasty was designed at the base of the flap. Because this flap had a longer arc to its border than the flap shown in Figure 7-23, it was not necessary to excise an equalizing triangle of skin along the border of the flap. However, in contrast to the larger flap shown in Figure 7-21, the Z-plasty designed at the base of the flap was necessary to avoid excision of such a triangle of skin. The three skin defects of the superior neck discussed in this section support the axiom that the larger the rotation flap, the less likely is the need to excise an equalizing Burow triangle along the border of the flap.
Case 6
As discussed in Case 5, rotation flaps are an effective way of reconstructing skin defects located in the superior aspect of the neck because redundant skin in the submental area can be used to create sizeable flaps. Rotation flaps can also be very useful to repair skin defects of the lower neck. An example of this is shown in Figure 7-25. A 53-year-old woman had micrographic surgery to remove a basal cell carcinoma from the right shoulder. The defect measured 7.5 × 6.3-cm and involved the skin of the lower neck and supraclavicular region. This defect could have been repaired with an advancement, transposition, or rotation skin flap. A rotation flap was designed to recruit redundant skin from the supraclavicular fossa. A Z-plasty incision was designed at the base of the flap to facilitate closure of the secondary defect and to avoid the need to excise a Burow triangle. The flap was elevated in the subcutaneous tissue plane, and the donor site was closed under moderate wound closure tension. Excision of the standing cutaneous deformity was performed at the lateral border of the defect parallel to the clavicle. Because of excessive wound closure tension, a limited hypertrophic scar formed along the advancing border of the flap. The scar hypertrophy regressed in response to triamcinolone injections.
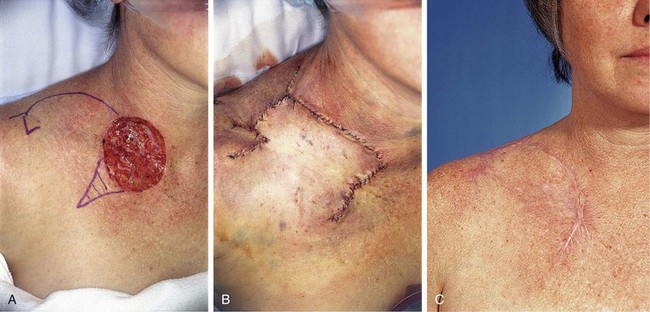
FIGURE 7-25 A, A 7.5 × 6.3-cm skin defect of inferior neck. Rotation flap designed for repair. Anticipated standing cutaneous deformity marked with vertical lines. B, Flap in place. Z-plasty eliminated need to excise an equalizing Burow triangle. C, Postoperative view at 8 months. No revision surgery performed.
Case 7
The patient shown in Figure 7-26 presented with a 1.2 × 1.2-cm circular skin defect of the upper lip after micrographic surgery for basal cell carcinoma. The options for repair of this defect included bilateral advancement flaps, a transposition flap from the cheek, a subcutaneous tissue pedicle island advancement flap, and a rotation flap from the lateral tissues of the lip. A rotation flap was selected for repair and was designed so that the border of the flap was positioned in the melolabial crease with a back cut at the level of the oral commissure. The standing cutaneous deformity resulting from pivoting of the flap was excised inferior to the defect. The flap was elevated superficial to the orbicularis oris and was based on the subcutaneous tissue of the oral commissure and on the skin of the lower lip. After the flap was dissected, a Z-plasty at the base of the flap was used to eliminate the need to excise an equalizing Burow triangle. The flap design enabled strategic placement of the wound closure suture line in the melolabial crease (Fig. 7-26C).

FIGURE 7-26 A, A 1.2 × 1.2-cm skin defect of lateral upper lip. Rotation flap designed for repair. Horizontal lines represent anticipated standing cutaneous deformity (SCD). Back cut designed to facilitate pivotal movement. B, Flap in place. Z-plasty designed to eliminate need to excise an equalizing Burow triangle. C, Majority of wound closure suture line positioned in melolabial crease for maximum scar camouflage. D-G, Preoperative and 3-year postoperative views. Hypopigmentation causes noticeable scar. No revision surgery performed.
A skin defect of the upper lip in a location similar to that of the previously discussed defect measured 1.5 × 2.0-cm and was also repaired with a rotation flap (Fig. 7-27). The arc of the border of the flap was positioned in the melolabial crease, and the standing cutaneous deformity resulting from the pivotal movement of the flap was excised inferior to the defect. Similar to the previously discussed case, a Z-plasty designed at the base of the flap was used to facilitate flap transfer without the need for excising an equalizing Burow triangle of skin. Postoperatively, the patient developed a hypertrophic scar of the vertical portion of the repair extending from the vermilion to the nose. This was corrected with a Z-plasty 5 months later. The result of the revision surgery is shown in Figure 7-27C, D.

FIGURE 7-27 A, A 1.5 × 2.0-cm skin defect of upper lip. Rotation flap designed with Z-plasty at base. B, Flap in place. C, D, Postoperative views at 1 year. Z-plasty performed on vertical portion of scar.
Although rare relative to the upper lip, skin cancers of the lower lateral lip do occur and can be repaired with cutaneous rotation lip flaps similar in design to those already discussed. In such circumstances, flaps are designed to be based superiorly, recruiting the remaining skin of the lateral lower lip and the commissure area into the flap. Like inferiorly based flaps, superiorly based flaps are designed so that their borders lie within or parallel to the melolabial crease. An example of this type of flap is seen in Figure 7-28. The defect resulted from excision of a morpheaform basal cell carcinoma and was repaired with a cutaneous rotation flap from the skin of the upper lip and medial cheek. As in the upper lip defects previously discussed, the standing cutaneous deformity was excised along the vermilion-cutaneous border, and the majority of the flap border remains parallel to the melolabial crease to provide maximum scar camouflage.

FIGURE 7-28 A, A 5 × 3-cm skin defect of lower lip. Rotation flap designed for repair. Arc of flap positioned parallel to melolabial crease. Anticipated standing cutaneous deformity (SCD) marked for excision along border of upper vermilion. B, Flap in place. C, Postoperative view at 1.5 years. No revision surgery performed.
References
1. Larrabee, WF, Jr. Design of local skin flaps. Otolaryngol Clin North Am. 1990; 23:899.
2. Larrabee, WF, Jr., Galt, JA. A finite element model of skin deformation. III. The finite element model. Laryngoscope. 1986; 96:413.
3. Dzubow, LM. Facial flaps: biomechanics and regional applications. Norwalk, Ct: Appleton and Lange; 1990.
4. Esser, JF. Studies in plastic surgery of the face. Ann Surg. 1917; 65:297.
5. Larrabee, WF, Jr., Sutton, D. The biomechanics of advancement and rotation flaps. Laryngoscope. 1981; 91:726.
6. Dzubow, LM. Indications for a geometric approach to wound closure following Mohs surgery. J Dermatol Surg Oncol. 1987; 13:480.
7. Dzubow, LM. The dynamics of flap movement: the effect of pivotal restraint on flap rotation and transposition. J Dermatol Surg Oncol. 1987; 13:1348.
8. Buckingham, ED, Quinn, FB, Calhoun, KH. Optimal design of O-to-Z flaps for closure of facial skin defects. Arch Facial Plast Surg. 2003; 5:92.
9. Ahuja, RB. Geometric considerations in the design of rotation flaps in the scalp and forehead region. Plast Reconstr Surg. 1988; 81:900.
10. Saad, MN, Maisels, DO. Further applications of the rotation advancement technique. Br J Plast Surg. 1972; 25:116.
11. Golomb, FM. Closure of the circular defect with double rotation flaps and Z-plasties. Plast Reconstr Surg. 1984; 74:813.
12. Album, MJ. Repair of large scalp defect by bilateral rotation flaps. J Dermatol Surg Oncol. 1978; 4:906.
13. Baker, SR. Options for reconstruction in head and neck surgery. In: Cummings CW, Fredrickson FM, Harker LA, et al, eds. Otolaryngology—head and neck surgery, update I. St. Louis: Mosby; 1989:192.
14. Kroll, SS, Reece, GP, Robb, G, Black, J. Deep-plane cervicofacial rotation-advancement flap for reconstruction of large cheek defects. Plast Reconstr Surg. 1994; 94:88.
15. Elliott, RA, Jr. Rotation flaps of the nose. Plast Reconstr Surg. 1969; 44:147.
16. Rieger, RA. A local flap for repair of the nasal tip. Plast Reconstr Surg. 1967; 40:147.
17. Rigg, BM. The dorsal nasal flap. Plast Reconstr Surg. 1973; 52:361.
18. Marchac, D, Toth, B. The axial frontonasal flap revisited. Plast Reconstr Surg. 1985; 76:686.
19. Rohrich, RJ, Muzaffar, AR, Adams, WP, Jr., et al. The aesthetic unit dorsal nasal flap: rationale for avoiding a glabellar incision. Plast Reconstr Surg. 1999; 104:1289.
20. Johnson, TM, Swanson, NA, Baker, SR, et al. The Reiger flap for nasal reconstruction. Arch Otolaryngol Head Neck Surg. 1995; 121:634.