Robotic Gynecologic Surgery
The da Vinci surgical system (Fig. 121–1) is a minimally invasive robotic surgical platform approved by the FDA in 2005 for gynecologic surgeries. It is currently the only commercially available robotic surgical system. Utilization of robotic gynecologic surgery is rapidly increasing in the United States. Examples of gynecologic surgeries that can be performed with robot assistance include myomectomy, simple and radical hysterectomy, lymph node dissection, tubal reanastomosis, and sacral colpopexy. Robotic surgery was first conceived by the military, but it has evolved recently to enhance minimally invasive and laparoscopic surgery in the community.
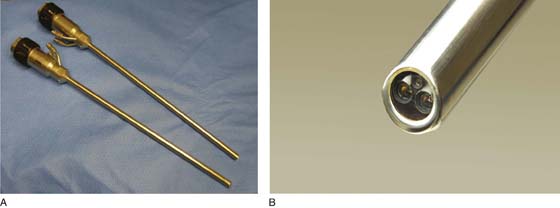
Robotic surgery offers several advantages when compared with laparoscopic surgery. First, a magnified, three-dimensional, stereoscopic vision system is used (Fig. 121–2A, B). Second, EndoWrist instruments (designed with seven degrees of motion that mimic the human hand and wrist) provide hand movements with unparalleled precision, control, and dexterity (Fig. 121–3A through C). Last, the operating surgeon sits comfortably at an ergonomically designed surgeon console and controls the EndoWrist instruments and camera with hand controls and foot pedals (Fig. 121–4A, B).
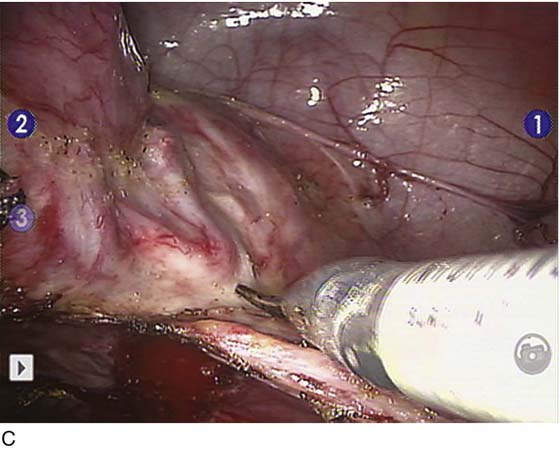
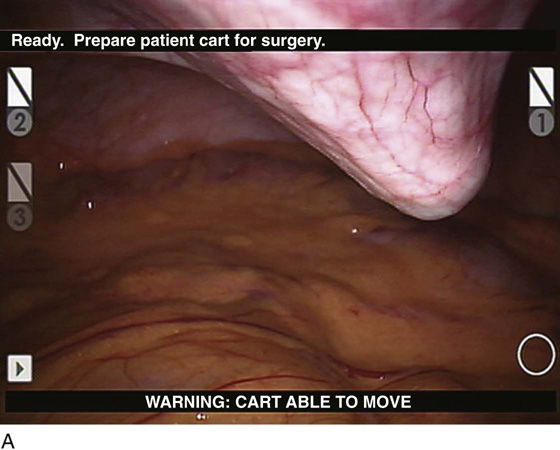
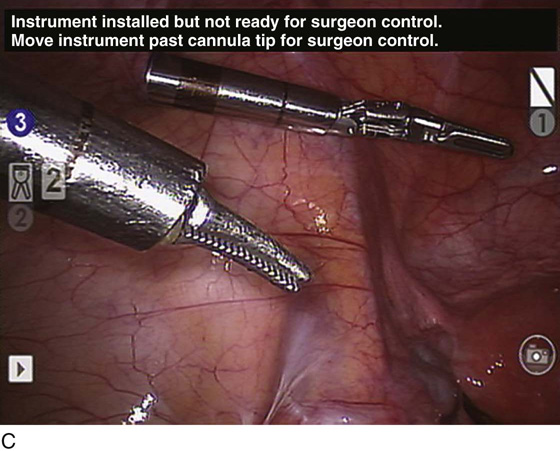
The basic setup includes a robotic master console, a patient-side robot, and a vision tower with video screen. Once anesthetized, the patient is placed in dorsal lithotomy position in Allen stirrups and then is prepped and draped (Fig. 121–5). If a hysterectomy is to be performed, usually a uterine manipulator is placed (Fig. 121–6). Port placement varies, depending upon the surgeon and the operation to be performed. The da Vinci surgical system allows for two or three surgical arms and a camera port (all controlled by the operating surgeon at the console) (Fig. 121–7). Additionally, one or two assistant ports are placed. Once the ports are placed, the patient is placed in Trendelenburg’s position; the patient side cart (with robotic arms) is docked to the ports, and instruments are inserted through the robotic arms for console surgeon control at the bedside master console (Fig. 121–8). The surgery is then performed by the surgeon sitting at the master console with one or two assistants at the bedside (one for uterine manipulation and one for suction/irrigation, retraction, introducing suture, etc).
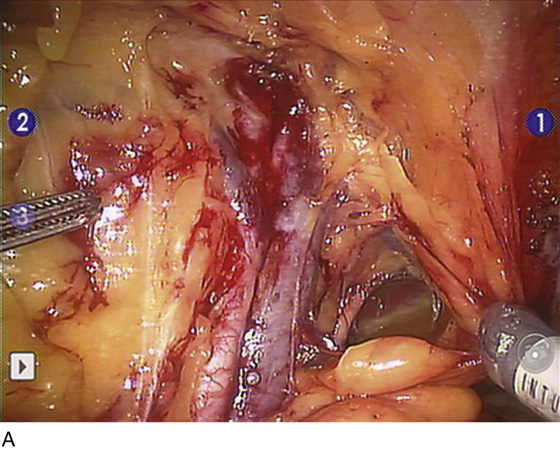
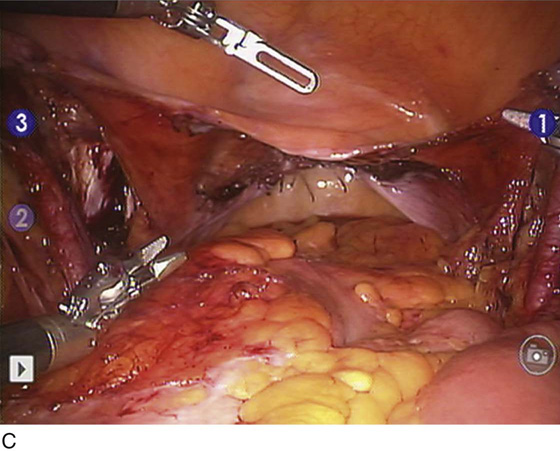
Potential patient benefits of minimally invasive robotic surgery compared with an open abdominal approach include shorter hospital stay, faster recovery, quicker return to normal activities, decreased incidence of wound infection, and less pain, blood loss, and scarring. Because robotic gynecologic surgery has been FDA approved only since 2005, data comparing it with open surgery and conventional laparoscopy are just becoming available. In general, gynecologic comparison of robotic hysterectomy (Fig. 121–9) versus conventional laparoscopic hysterectomy has shown a decreased need to convert to an exploratory laparotomy, reduced mean blood loss, and a similar rate of complications. In gynecologic oncology, lymph node counts (Fig. 121–10) have been shown to be higher with a robotic approach to both endometrial cancer and cervical cancer cases when compared with conventional laparoscopy and open surgery. Overall survival data comparisons are lacking at this time.
The number of gynecologic surgeries performed robotically in the United States is exponentially increasing. This advanced surgical technology offers potential benefit to both patients and physicians.
FIGURE 121–1 The da Vinci surgical system consists of a surgeon console (left), a patient-side robot cart (middle), and a vision tower (right). (Copyright Intuitive Surgical, Inc. Reproduced with permission.)
FIGURE 121–2 A. The endoscope vision system is available in both 0° and 30°. B. The 30° endoscope is pictured. (Copyright Intuitive Surgical, Inc. Reproduced with permission.)
FIGURE 121–3 A. EndoWrist instruments with 7° of motion that provide greater precision control and dexterity when compared with laparoscopic instruments. (Copyright Intuitive Surgical, Inc. Reproduced with permission.) B. Comparison of EndoWrist instruments versus the size of a dime puts into perspective their small size. (Copyright Intuitive Surgical, Inc. Reproduced with permission.) C. This picture shows the precise dissection and superior visualization afforded with robotic gynecologic surgery. Pictured is the usage of monopolar scissors skeletonizing the right uterine artery during a hysterectomy.
FIGURE 121–4 A. The operating surgeon sits at the surgeon console and controls the EndoWrist instruments with hand controls. B. The operating surgeon sits at the surgeon console and controls the camera with foot pedals.
FIGURE 121–5 The patient is placed in Allen stirrups in steep Trendelenburg’s position to facilitate robotic gynecologic surgery.
FIGURE 121–6 Several types of uterine manipulators can be used to facilitate gynecologic robotic surgery. The ZUMI (Zinnanti Uterine Manipulator Injector) clamp (CooperSurgical, Trumbull, CT) and CONMED VCare (Utica, NY) are shown here.
FIGURE 121–7 The operating surgeon has control of three instruments (a prograsp, a PK dissector (Gyrus ACMI, Southborough, MA) with bipolar capabilities, and monopolar scissors with hand controls). The operating surgeon also controls the camera with a foot pedal.
FIGURE 121–8 A. An 8-mm blunt tip trocar and cannula are being inserted under direct visualization to the left of the midline. The three robotic arms through which instruments are inserted are 8 mm in diameter. B. The 8-mm robotic cannula is inserted to the thick black line to provide maximum flexibility once the instrument is inserted. C. After insertion of the cannulas, two robotic instruments are placed by the bedside assistant. After insertion by the assistant, the operating surgeon takes control of the instruments.
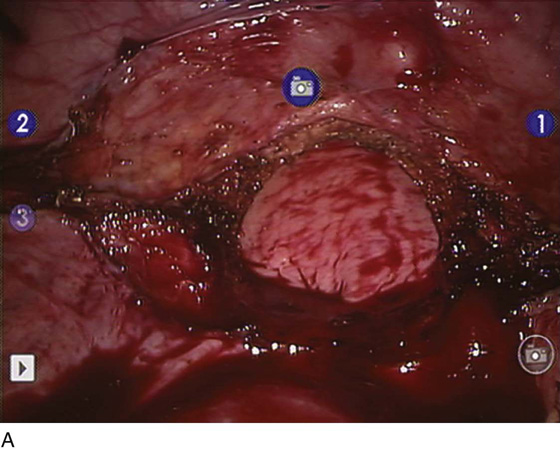
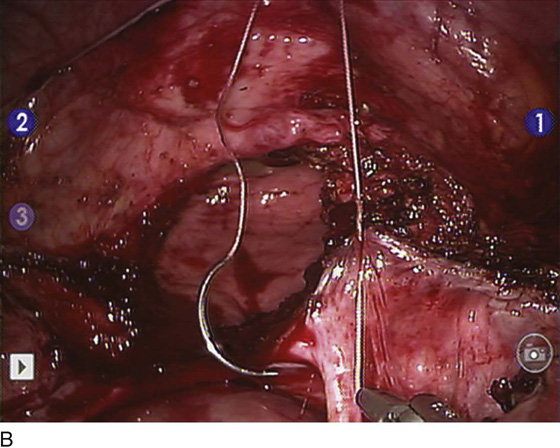
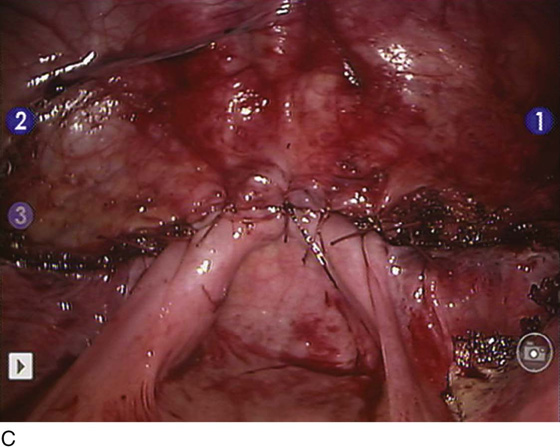
FIGURE 121–9 A. An open vaginal cuff is pictured after the removal of the uterus, cervix, ovaries, and fallopian tubes. B. Needle drivers have been inserted into two of the robotic ports, and the operating surgeon is now closing the vaginal cuff with 0 Vicryl interrupted sutures. Using robotic assistance facilitates suturing laparoscopically. C. The vaginal cuff has been reapproximated with sutures.
FIGURE 121–10 A. During endometrial cancer staging surgery, the left-sided external iliac lymph nodes are removed. After the paravesical and pararectal spaces are opened, the lymph nodes are removed from the bifurcation of the iliac vessel proximally to the recurrent circumflex vein distally. B. Exposure of the obturator nerve under the right external iliac vein is pictured. The right obturator lymph nodes have been removed. C. Endometrial cancer staging surgery has been performed with removal of the uterus, cervix, ovaries, fallopian tubes, and pelvic/para-aortic lymph nodes. The lymph nodes were placed in an endopouch bag and were taken out through the vagina before its closure.

 James Pavelka
James Pavelka