Chapter 24 Rigid Bronchoscopy with Y Stent Insertion at Left Secondary Carina
Case Description
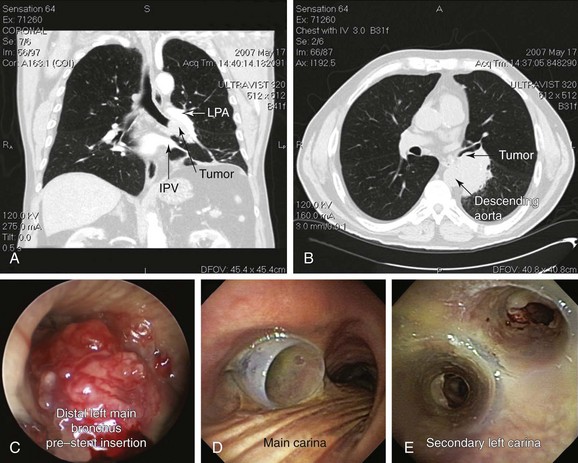
A 75-year-old man with a 120–pack-year history of smoking and COPD (FEV1 52% predicted, DLCO 39% predicted) developed progressive dyspnea, a weak and hoarse voice, and hemoptysis. His usual exertional dyspnea had progressed to the point that he now required assistance with activities of daily living. Chest CT showed a 6 × 5 × 7 cm left infrahilar mass involving the distal left main bronchus (LMB) and the entrance to the left upper and lower lobe bronchi (Figure 24-1, A and B). In addition, mediastinal lymphadenopathy was significant in stations 7 (subcarinal) and 4 L (left lower paratracheal). Flexible bronchoscopy showed an immobile left vocal cord and near complete obstruction in the distal LMB characterized by extrinsic compression and exophytic endoluminal tumor with hypervascular mucosa (Figure 24-1, C). Examination of the airways distal to the tumor was possible using forced saline lavage and showed patent distal segments but significant involvement of the left secondary carina (LC2). Rigid bronchoscopy was performed under general anesthesia with spontaneous assisted ventilation. Endobronchial needle aspiration (EBNA) with rapid on-site evaluation (ROSE) revealed non–small cell lung cancer (NSCLC). Nd:YAG laser photocoagulation and bronchoscopic debulking partially restored patency to left upper and lower lobe bronchi. However, tumor infiltration, cartilaginous collapse, and extrinsic compression required insertion of a large Y silicone stent (16 mm diameter tracheal limb, 12 mm bronchial limbs) placed within the left main bronchus (Figure 24-1, D and E).
Case Resolution
Initial Evaluations
Physical Examination, Complementary Tests, and Functional Status Assessment
This patient required considerable assistance at home. His functional impairment was consistent with a Karnofsky Performance Scale score (KPS) of 50. At the time of hospitalization, however, KPS was only 20 (severely disabled, where hospitalization was necessary but death was not imminent).1 His Eastern Cooperative Oncology Group (ECOG) performance scale, which may be a better predictor of prognosis than KPS,2,3 was 3 (i.e., the patient was capable of only limited self-care and was confined to bed or chair for more than 50% of waking hours). Assessment of this patient’s performance status is essential for guiding therapeutic interventions because this degree of impairment, due to lung cancer or comorbid conditions (e.g., chronic obstructive pulmonary disease [COPD]), may preclude resection or, alternatively, chemoradiotherapy.4 In fact, this patient was not operable based on his pulmonary function tests and functional status. Relevant to his case, however, is that the combination of interventional bronchoscopy and external beam radiation therapy (EBRT) might improve survival, symptoms, and quality of life, as has been previously shown in patients with lung cancer, central airway obstruction, and KPS less than 50.
The patient’s weak voice and hoarseness are explained by unilateral (left) vocal cord immobility as noted on bronchoscopy (see video on ExpertConsult.com) (Video V.24.1![]() ). This was likely due to unilateral recurrent laryngeal nerve (RLN) injury, which caused the affected vocal fold to rest in the paramedian position. The contralateral vocal fold may or may not provide adequate glottic closure during phonation. If closure is not achieved, the residual glottal gap results in air escape with a weak voice secondary to a “leaky valve” phenomenon.5 In unilateral RLN injury, the glottic aperture is usually adequate, and related dyspnea and stridor are rare. Glottal incompetence, however, increases the risk for aspiration, particularly with thin liquids. Cough, which requires transient tight glottic closure, may also be affected; this is important in cases of airway stent insertion with risk for mucus plugging and difficulty raising secretions. Associated sensory loss from RLN involvement may also cause dysphagia, a symptom not seen in our patient. With regard to staging, RLN involvement is consistent with T4 disease. In conjunction with N2 disease on computed tomography (CT) scan (involvement of stations 7 and 4 L), this patient’s clinical stage is at least IIIB, and estimated median survival time is 10 months and 5 years for 7% despite multimodality treatment.6
). This was likely due to unilateral recurrent laryngeal nerve (RLN) injury, which caused the affected vocal fold to rest in the paramedian position. The contralateral vocal fold may or may not provide adequate glottic closure during phonation. If closure is not achieved, the residual glottal gap results in air escape with a weak voice secondary to a “leaky valve” phenomenon.5 In unilateral RLN injury, the glottic aperture is usually adequate, and related dyspnea and stridor are rare. Glottal incompetence, however, increases the risk for aspiration, particularly with thin liquids. Cough, which requires transient tight glottic closure, may also be affected; this is important in cases of airway stent insertion with risk for mucus plugging and difficulty raising secretions. Associated sensory loss from RLN involvement may also cause dysphagia, a symptom not seen in our patient. With regard to staging, RLN involvement is consistent with T4 disease. In conjunction with N2 disease on computed tomography (CT) scan (involvement of stations 7 and 4 L), this patient’s clinical stage is at least IIIB, and estimated median survival time is 10 months and 5 years for 7% despite multimodality treatment.6
Comorbidities
This patient had moderate, Global Obstructive Lung Disease (GOLD) stage II COPD. Although no other comorbidities were reported, careful examination and review of systems are warranted because COPD is associated with hypertension, coronary heart disease, stroke, obstructive sleep apnea, depression, anxiety, and cognitive dysfunction, which could preclude or complicate interventions under general anesthesia.4
Support System
The patient had good social support from his daughter and his wife. Early discussions about quality of life and symptom concerns are warranted because patients suffering from cancer will commonly develop pain, dyspnea, cough, and fatigue during the course of their illness.7 These conversations took place with the patient and his family because a diagnosis of cancer has a significant psychological and emotional impact on family members and caregivers as well.8
Patient Preferences and Expectations
This gentleman had expressed his desire for diagnosis and was ready to consider all available treatment options. He was very clear, however, that he did not want to live “being dependent on machines,” and he wanted to make all decisions regarding his care. In the United States, most patients diagnosed with cancer want a shared or active role in the decision-making process, usually with greater participation than what actually occurs. Role preferences (active vs. passive), however, vary greatly during decision making, and repeated assessments are required to meet patients’ expectations and improve their satisfaction with treatment decisions.9
Procedural Strategies
Indications
This patient required tissue diagnosis. We elected to proceed with rigid bronchoscopy under general anesthesia to restore airway patency with laser and silicone stent insertion and to diagnose the airway lesion using endobronchial biopsy, bronchial washing, and/or endobronchial needle aspiration. Chemoradiotherapy currently constitutes the standard of care for patients with inoperable locally advanced non–small cell lung cancer (NSCLC).10 This treatment, however, is usually restricted to patients who maintain a good performance status.11
Central airway obstruction (CAO) in the setting of NSCLC is associated with a very poor prognosis. In one study, median and 1 year survival of patients with malignant CAO were reportedly as low as 3.4 months and 15%, respectively.12 However, patients with advanced NSCLC with locally treated CAO combined with systemic chemotherapy might have survival rates similar to those patients without CAO treated with chemotherapy alone.13 Interventional bronchoscopic procedures in this patient with inoperable disease are expected to restore airway patency and improve lung function, dyspnea, and functional status, thus allowing initiation of systemic therapy, which could improve his survival.14
Contraindications
No absolute contraindications to rigid bronchoscopy were noted. Although COPD treatment should be optimized before elective interventions to reduce perioperative complications, our patient had stable disease at the time of evaluation and was being treated with short-acting β2-agonists and long-acting anticholinergic agents in accordance with international guidelines.15
Expected Results
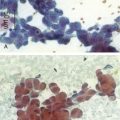
For diagnosis, endobronchial needle aspiration (EBNA) with rapid on-site evaluation (ROSE) was performed. In patients with visible endobronchial lesions such as this, the diagnostic yield increases from 76% with conventional procedures alone to 96% with EBNA in addition to conventional procedures (washings, brushings, and biopsy).16
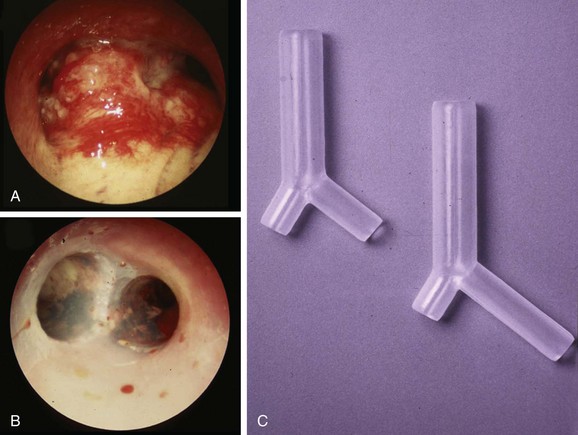
For restoring airway patency in our patient with near complete obstruction in the distal left main bronchus (LMB), left secondary carina (LC2) involvement, and a mixed pattern of obstruction (extrinsic and endoluminal exophytic), a straight metal or silicone stent would not have restored patency to the obstructed lobar bronchi. Therefore we decided to insert a silicone Y stent. This type of stent can be used for patients with fixed or dynamic CAO from benign or malignant disease, but the most common uses are to restore airway patency, to improve dyspnea and quality of life for patients with malignant CAO involving the mainstem bronchi and the lower trachea (Figure 24-2), and to reduce recurrent infection in patients with tracheoesophageal or bronchoesophageal fistulas.17–20 Y stents are also effective in restoring airway patency, and they improve symptoms in patients with severe diffuse tracheobronchomalacia, but with a high rate of nonfatal complications.21,22 In our patient, a Y silicone stent insertion was planned to restore and maintain LMB and left upper lobe (LUL) and left lower lobe (LLL) airway patency, which would allow the following:
1. Initiation of systemic therapy: By improving functional status, this patient could become a candidate for systemic treatment; in fact, evidence suggests that patients with advanced NSCLC and CAO who undergo successful interventional bronchoscopy to relieve airway obstruction might have survival similar to that of patients without CAO.13
2. Improved exercise capacity and dyspnea: A significant improvement in symptoms in up to 94% of patients undergoing central airway stent insertion has been reported, although 40% of patients required multiple procedures. This raises questions about the costs per quality of life-years in patients with advanced disease.14
Team Experience
Studies reporting an association between results of interventional bronchoscopy, procedure-related complications, and the required level of technical expertise have not yet been performed. It is known, however, that survival and complications after such procedures are worse for malignant than for benign CAO, and it was suggested that these patients should be considered distinct populations to be analyzed and reported separately.23 One can only hypothesize that referral to an experienced bronchoscopist and oncologic team will result in reduced complications, more rapid diagnosis, greater restoration of airway patency, and earlier discharge from the hospital.
Risk-Benefit Analysis
For diagnosis, we chose to perform EBNA before proceeding with laser photocoagulation. In our experience, EBNA has a lower risk of bleeding and provides immediate diagnosis when ROSE is available. In contrast with endobronchial biopsy, however, tissue architecture is not seen.16 With regard to restoring airway patency, the risks of further physiologic compromise and massive bleeding were considered to be outweighed by the benefit of restoring airway patency, the ability to diagnose the lesion, and improved functional status and the offer of systemic therapy. Alternatives to our approach should be considered on a case-by-case basis.
Therapeutic Alternatives for Restoring Airway Patency
These include endobronchial and systemic therapies.
• Endobronchial brachytherapy (EBB): This technique has proven efficacy in patients with endoluminal tumor and a substantial extrabronchial component. It is based on the principle of inverse square law, which states that dose rate decreases as a function of the inverse square of the distance to the source center, making it possible to achieve a high irradiation dose in the center of the irradiation source with a fast decrease toward the periphery. EBB offers significant palliation with rates of recanalization ranging from 60% to 90%, and symptomatic improvement is seen in 70% to 80% of patients. The variability in reported results is explained by patient selection, different treatment schemata, and the use of additional treatments. For palliation of NSCLC symptoms, however, a Cochrane meta-analysis concluded that EBB alone was less effective than EBRT. For patients previously treated by EBRT who are symptomatic from recurrent CAO, however, EBB may be considered.24 EBB is usually performed via flexible bronchoscopy. Effects are delayed, and complications include hemoptysis, which could be fatal in up to 21% of patients, as well as fistula formation, radiation bronchitis (10%), and bronchial stenosis. This modality was not considered optimal for our patient because of his severe airway obstruction and marginal pulmonary function. Furthermore, EBB for this tumor would have to be extensive, including the LMB along with the LUL and the LLL. Treatment in the upper lobes is associated with the highest incidence of hemoptysis, probably because of the proximity of great vessels.
• Photodynamic therapy (PDT): This treatment can be performed via flexible bronchoscopy and is approved for local regional palliation for advanced NSCLC. This modality is most effective when more than 50% narrowing results from mucosal disease.25 The outcome of PDT seems to be best, however, when patients have a relatively good performance status.26 In addition, associated risks of phototoxicity for approximately 4 weeks post intervention (≈20%) and a therapeutic effect that is delayed for at least 48 hours make it less than ideal in our patient. PDT might actually worsen airway obstruction during the initial post-treatment period because of sloughing of airway mucosa and retained tumor debris. Similar to EBB, PDT is contraindicated in patients at high risk for fatal massive hemoptysis.
• Cryotherapy: This approach causes thrombosis and necrosis of tumor tissues and could have been used for the exophytic, endobronchial component of this patient’s CAO. No risk for airway fire or perforation is present, but cryotherapy can cause cold-induced bronchospasm—a matter of particular risk in our patient with COPD. Cryotherapy has been shown to be most effective when performed in combination with EBRT.27 Similar to PDT and EBB, the effect is delayed and initially might worsen airway obstruction, causing post obstructive pneumonia due to sloughed necrotic tissue.
• Electrocautery and argon plasma coagulation (APC): These techniques remove the exophytic endoluminal component and provide superficial cauterization (3 to 6 mm), which may not suffice to stop large airway bleeding. APC has a risk for gas embolization, which is relevant in our patient because of the vascular pattern of his airway tumor. Argon gas is heavy, inert, and much less soluble in the body than carbon dioxide. As gas is forced into the airway wall, causing perforation, it collects in a blood vessel and passes into the systemic circulation, causing embolism.28 Erosion from tumor also presents a risk to major vessels. Systemic, life-threatening gas embolism has been reported as a complication of endobronchial APC.29
• Fully or partially covered metal stent insertion: This alternative may be used in cases of malignant CAO. In patients with significant comorbidities precluding general anesthesia, it is a suitable alternative in that stents can be placed via flexible bronchoscopy with or without fluoroscopy.30 Metal stents are more costly than silicone stents and can be difficult to remove. Furthermore, a straight stent would not palliate this patient’s lobar bronchial obstruction.
• Flexible bronchoscopy using laser: This procedure could be performed but would be very time-consuming in this patient because of his extensive intraluminal disease. Furthermore, this would only assist with management of the endobronchial component, and stent insertion would still be necessary to palliate extrinsic obstruction. Because of severe bleeding or bronchial obstruction from tissue debris, pulmonary hygiene may be difficult in this patient with COPD.
• Systemic therapies such as EBRT and systemic chemotherapy: These treatments might be appropriate once a final tissue diagnosis is available. If NSCLC is confirmed, this tumor would be a clinical stage IIIB.6 Current evidence shows that for individuals with unresectable disease, a good performance score, and minimal weight loss, treatment with combined chemoradiotherapy results in better survival than radiotherapy alone. Concurrent chemoradiotherapy seems to be associated with improved survival compared with sequential chemoradiotherapy.31 Restoration of airway patency could improve the performance score and accelerate appropriate initiation of systemic therapy. Initiation of EBRT as a primary treatment without attempts to restore airway patency is of doubtful benefit in this patient. EBRT is only variably effective for cancer-induced CAO, especially when CAO results in atelectasis. In a study of 330 patients, EBRT palliated hemoptysis in 84% of patients and superior vena cava syndrome in 86% of patients, but atelectasis in only 23%.32 EBRT after effective laser treatment, however, could potentially improve survival.33 A factor that limits most EBRT treatments is unwanted exposure of the normal lung parenchyma, heart, spine, and esophagus.
Cost-Effectiveness
The costs of interventional procedures providing immediate palliation of airway patency are probably small compared with the costs of repeated systemic therapies, but these economic factors might be institution, insurer, and country specific. Silicone stent insertion requires rigid bronchoscopy under general anesthesia in an operating theater, which increases costs. Risk is associated with general anesthesia, especially in patients with significant cardiopulmonary disorders. After taking into account the type of CAO (mixed extrinsic compression and exophytic endoluminal), indications, contraindications, tissue interactions, response time, and expected results of various bronchoscopic interventions, we thought that neodymium-doped yttrium aluminum garnet (Nd:YAG) laser therapy followed by silicone stent insertion would offer rapid improvement in symptoms, so that systemic therapy could be initiated. A multimodality bronchoscopic approach is likely to be more effective than a single modality for symptomatic palliation of lung cancer–related CAO. In a study comparing Nd:YAG laser, stent insertion, PDT, or brachytherapy alone versus a combination of bronchoscopic interventions such as laser and stent insertion, or versus laser and stent insertion closely followed by brachytherapy, significant improvement in survival was noted in the multimodality group. One-year and 3-year cumulative survival rates for the two groups were 51.3% versus 50% and 2.3% versus 22%, over 14 months’ follow-up.34
Techniques and Results
Anesthesia and Perioperative Care
Concern for hypoxemia and hypoventilation during induction exists because of the already critical bronchial narrowing.35 If possible, induction should be cautious and preferably provided without neuromuscular blockers, which might cause complete loss of muscular tone in the posterior membrane and may worsen an already critically narrowed airway.36 Spontaneous-assisted ventilation can be provided through an open circuit during the rigid bronchoscopic procedure.37 In case of a large air leak resulting in an inability to ventilate and oxygenate satisfactorily, the mouth and the nose can be packed with gauze. In case of bleeding from the large tumor in the distal LMB, the patient should be quickly turned toward his left lateral decubitus. A large tamponade balloon may have to be inserted into the LMB to protect the contralateral bronchial tree. Because Nd:YAG laser is used, fire safety precautions are followed and the fraction of inspired oxygen (FiO2) is reduced to less than 0.4 before and during laser activation.
Anatomic Dangers and Other Risks
The left pulmonary artery is anterior, the descending aorta is posterior, and the inferior pulmonary vein and left atrium are medial to the distal LMB (see Figure 24-1). Therefore, laser treatment should be performed carefully in this area to avoid direct application onto the posterior and medial walls. In hypervascular tumors, the absorption of laser energy is high for Nd:YAG laser, and perforation risk is present. Airway obstruction from blood and tumor debris may cause hypoxemia. Technical considerations during stent insertion include concern for (1) perforation of the medial wall of the main bronchus, resulting in bronchomediastinal fistula and possible mediastinal misplacement of the stent; (2) perforation of the posterior membrane, which may cause aortic laceration; and (3) hypoventilation and hypoxemia, which occur when the large stent does not unfold satisfactorily.
Results and Procedure-Related Complications
After induction of general anesthesia, the patient was intubated with a 13 mm Efer-Dumon rigid ventilating bronchoscope. Inspection of the trachea and the right bronchial tree was unremarkable. On the left side, the tumor was highly friable, invading the posterior wall and obstructing the distal LMB, as well as the entrance to the left upper and lower lobes (see Figure 24-1). Once the blood clot covering the tumor was removed, we performed EBNA to the submucosal tumor. Bleeding after EBNA stopped after instillation of 60 mL of saline. ROSE revealed NSCLC. Nd:YAG laser photocoagulation was followed by rigid bronchoscopic debulking in the distal LMB. The tumor involved the LC2 and lobar bronchi. Airway patency to the LUL was restored, but the tumor extended into the LLL bronchus. Once passed, the basal segments were open. Because of the tumor’s location in the distal LMB and its extension to the LC2 and lobar bronchi, a large Y silicone stent was inserted within the LMB, so that its bronchial limbs extended into the LUL and LLL. The stent had a 16 mm diameter tracheal limb and 12 mm diameter bronchial limbs. The more vertical limb entered the LLL, and the more horizontal limb was shortened to less than 2 cm so that it would enter the LUL (see Figure 24-1). Silicone Y stents are usually deployed into the trachea and LMB and RMB using the “push” technique or the “pullback” technique. With the push technique, the stent is ejected from the bronchoscope above the carina and then is pushed down with an open rigid grasping forceps placed at stent bifurcation. With the pullback technique, both bronchial limbs are placed within one bronchus (usually the one most involved with disease) then are pulled back slowly until the shorter limb pops out. The stent can then be adjusted using forceps. In our patient, both bronchial limbs were simultaneously present at the entrance to the LUL bronchus. The stent was pulled proximally to deploy the vertical (right) limb into the relatively straight LLL bronchus. The tracheal limb of the Y stent was now in the LMB (see video on ExpertConsult.com) (Video V.24.2![]() ). No perioperative complications were noted; the patient was extubated, recovered, and was discharged home the next day.
). No perioperative complications were noted; the patient was extubated, recovered, and was discharged home the next day.
Long-Term Management
Referral
The optimal treatment for stage IIIB NSCLC depends on several variables, including extent of disease, patient age, comorbidities, performance scores, and weight loss.31 Because of this, a thorough evaluation is warranted before patients are committed to potentially toxic treatments. After discussion in our multidisciplinary chest conference, given his lack of weight loss and improved performance status, concurrent chemoradiotherapy therapy was offered.
Follow-up Tests and Procedures
Complete staging included a whole body positron emission tomography (PET)/CT scan and brain magnetic resonance imaging (MRI) showing no extrathoracic disease. He was started on concurrent chemoradiotherapy. Follow-up bronchoscopies at 4 and 6 months post stent insertion revealed patent airways and no evidence of stent migration or obstruction by mucus or granulation. Stent insertion does not have to be permanent. In one report, airway stents were removed in 50% of patients with malignant CAO after a median of 31.7 days after successful systemic therapy.38 In cases where systemic therapy is unsuccessful, stent insertion maintains airway patency, relieves dyspnea, and improves quality of life.
Quality Improvement
We discussed whether our patient should undergo routine surveillance flexible bronchoscopy to identify stent-related complications or progression of tumor. Although evidence against this practice has been found,39 because of the particular location of this stent at LC2 and its unknown long-term consequences, we chose to perform surveillance bronchoscopy every 3 months and as needed on the basis of symptoms. In general, the risk of stent migration is rare, with an estimated incidence of 1% to 5%,12 and such migration may be even less common with Y stents. Impairment in mucociliary clearance may promote retained secretions and stent obstruction in about a third of cases. No published experience has described the use of Y stents for LMB/LUL/LLL obstruction.
In general, flexible bronchoscopies are reportedly necessary to remove secretions in up to 40% of patients with indwelling stents.14 Additional rigid bronchoscopic procedures, however, are seldom required in patients with malignant CAO, in part because of limited survival.12 We recognized the risk of stent revision in this patient because of his increased risk for fistula, in part secondary to tumor involvement, but also related to radiation therapy.
Discussion Points
1. Describe two techniques used to deploy a Y stent.
2. Describe the indications for stent insertion before initiation of systemic therapy in this particular patient.
3. List three potential complications resulting from stent insertion at the left secondary carina.
Expert Commentary
This 75-year-old male had moderate COPD but was severely debilitated, with an ECOG performance score of 3 due to a stage IIIB non–small cell lung cancer in the left infrahilar area with complete obstruction of the distal left main bronchus. He also had left vocal cord paralysis. CT scan noted lymph node metastases in stations 4 L (left lower paratracheal) and 7 (subcarinal). If we assume that the vocal cord paralysis is due to direct extension of the primary cancer, then the lesion would be T4, and the clinical stage would be T4N2M0 (assuming no distinct metastases) or stage IIIB. If vocal cord paralysis was due to N2 lymph node metastases, the clinical stage would be T3N2M0, stage IIIA.6 With IIIA or IIIB, the patient is inoperable owing to poor performance status, borderline pulmonary function, and multiple-station mediastinal nodal involvement.
We are told that the initial biopsy (EBNA) was called non–small cell lung cancer (NSCLC). Although this was adequate to proceed with endobronchial treatment, it is not adequate for optimal decision making regarding chemotherapy. Sufficient tissue is needed to determine whether the NSCLC is squamous cell, adenocarcinoma, or large cell because histology dictates optimal chemotherapy choices.40
One of the most exciting advances in lung cancer in the past few years has been the identification of sensitizing mutations, or so-called driver mutations. These have been most commonly identified in adenocarcinoma.41 Currently, the most important mutations to be elucidated are the tyrosine kinase domain of epidermal growth factor receptor (EGFR) and anaplastic lymphoma kinase (ALK).
Sensitizing mutations in EGFR (exon 19 deletion or exon 21 transition) and ALK are associated with an excellent clinical response to therapy with specific tyrosine kinase inhibitors and improvement in overall survival compared with standard chemotherapy.42,43 Accordingly, it is now the responsibility of the bronchoscopist to obtain adequate tissue samples for both histologic diagnosis and molecular testing. A simple aspiration cytology demonstrating NSCLC is inadequate and unacceptable as of this writing. Obtaining appropriate tissue specimens at the time of bronchoscopy is the responsibility of the bronchoscopist and provides an opportunity to make a significant contribution to the multidisciplinary management of the patient with lung cancer.
The large majority of centrally located NSCLC is of squamous cell histology and seldom contains the sensitizing mutations previously mentioned. However, mutations and gene amplifications are being identified and are likely to influence future treatment decisions. The usual treatment for unresectable stage IIIA and IIIB disease consists of concurrent chemotherapy and radiotherapy if the patient has a performance status of 0 or 1* and minimal weight loss (≤5%) over the previous 3 months.31 This patient had a performance status of 2 after endobronchial treatment. In this situation, treatment would have to be decided on an individual basis. Endobronchial disease is best treated with concurrent therapy rather than with radiation or chemotherapy alone or sequentially. However, concurrent therapy is more toxic than sequential therapy, especially in terms of esophageal toxicity. External beam radiotherapy is considered the standard method of irradiation rather than endobronchial brachytherapy (EBB), especially when combined with chemotherapy. In this patient with N2 disease in stations 4R and 7, EBB would not be appropriate for treating the nodal disease. Recent trials with concurrent chemoradiotherapy for definitive treatment of stage IIIA/B disease have reported a median survival time of 20 to 24 months, 2 year survival of 40% to 50%, and 5 year survival of approximately 20%.44,45 The patient under discussion was deemed suitable for concurrent chemoradiotherapy.
* The ECOG score, also called the World Health Organization (WHO) or Zubrod score, runs from 0 to 5, with 0 denoting perfect health and 5 death; 0—asymptomatic (fully active, able to carry on all predisease activities without restriction), 1—symptomatic but completely ambulatory (restricted in physically strenuous activity but ambulatory and able to carry out work of a light or sedentary nature).
1. Schag CC, Heinrich RL, Ganz PA. Karnofsky performance status revisited: reliability, validity, and guidelines. J Clin Oncol. 1984;2:187-193.
2. Oken MM, Creech RH, Tormey DC, et al. Toxicity and response criteria of the Eastern Cooperative Oncology Group. Am J Clin Oncol. 1982;5:649-655.
3. Buccheri G, Ferrigno D, Tamburini M. Karnofsky and ECOG performance status scoring in lung cancer: a prospective, longitudinal study of 536 patients from a single institution. Eur J Cancer. 1996;32A:1135-1141.
4. Sin DD, Man SF. Chronic obstructive pulmonary disease as a risk factor for cardiovascular morbidity and mortality. Proc Am Thorac Soc. 2005;2:8-11.
5. Havas T, Lowinger D, Priestley J. Unilateral vocal fold paralysis: causes, options and outcomes. Aust N Z J Surg. 1999;69:509-513.
6. Goldstraw P, Crowley J, Chanksy K, et al. The IASLC Lung Cancer Staging Project: proposals for the revision of the TNM stage groupings in the forthcoming (seventh) edition of the TNM classification of malignant tumours. J Thorac Oncol. 2007;2:706-714.
7. Podnos YD, Borneman TR, Koczywas M, et al. Symptom concerns and resource utilization in patients with lung cancer. J Palliat Med. 2007;10:899-903.
8. Duhamel F, Dupuis F. Guaranteed returns: investing in conversations with families of patients with cancer. Clin J Oncol Nurs. 2004;8:68-71.
9. Tariman JD, Berry DL, Cochrane B, et al. Preferred and actual participation roles during health care decision making in persons with cancer: a systematic review. Ann Oncol. 2010;21:1145-1151.
10. Trodella L, D’Angelillo RM, Ramella S, et al. Multimodality treatment in locally advanced non-small cell lung cancer. Ann Oncol. 2006;17:ii32-ii33.
11. Spira A, Ettinger DS. Multidisciplinary management of lung cancer. N Engl J Med. 2004;350:379-392.
12. Lemaire A, Burfeind WR, Toloza E, et al. Outcomes of tracheobronchial stents in patients with malignant airway disease. Ann Thorac Surg. 2005;80:434-438.
13. Chhajed PN, Baty F, Pless M, et al. Outcome of treated advanced non-small cell lung cancer with and without central airway obstruction. Chest. 2006;130:1803-1807.
14. Wood DE, Liu YH, Vallières E, et al. Airway stenting for malignant and benign tracheobronchial stenosis. Ann Thorac Surg. 2003;76:167-174.
15. Global Initiative for Chronic Obstructive Pulmonary Disease, Executive Summary: Global strategy for the diagnosis, management, and prevention of COPD. www.goldcopd.com, 2006. Accessed September 5, 2010
16. Mazzone P, Jain P, Arroliga AC, et al. Bronchoscopy and needle biopsy techniques for diagnosis and staging of lung cancer. Clin Chest Med. 2002;23:137-158.
17. Cavaliere S, Venuta F, Foccoli P, et al. Endoscopic treatment of malignant airway obstructions in 2,008 patients. Chest. 1996;110:1536-1542.
18. Mitchell JD, Mathisen DJ, Wright CD, et al. Resection for bronchogenic carcinoma involving the carina: long-term results and effect of nodal status on outcome. J Thorac Cardiovasc Surg. 2001;121:465-471.
19. Dutau H, Toutblanc B, Lamb C, et al. Use of the Dumon Y-stent in the management of malignant disease involving the carina: a retrospective review of 86 patients. Chest. 2004;126:951-958.
20. Shiraishi T, Kawahara K, Shirakusa T, et al. Stenting for airway obstruction in the carinal region. Ann Thorac Surg. 1998;66:1925-1929.
21. Murgu SD, Colt HG. Complications of silicone stent insertion in patients with expiratory central airway collapse. Ann Thorac Surg. 2007;84:1870-1877.
22. Ernst A, Majid A, Feller-Kopman D, et al. Airway stabilization with silicone stents for treating adult tracheobronchomalacia: a prospective observational study. Chest. 2007;132:609-616.
23. Ernst A, Simoff M, Ost D, et al. Prospective risk-adjusted morbidity and mortality outcome analysis after therapeutic bronchoscopic procedures: results of a multi-institutional outcomes database. Chest. 2008;134:514-519.
24. Cardona AF, Reveiz L, Ospina EG, et al. Palliative endobronchial brachytherapy for non-small cell lung cancer. Cochrane Database Syst Rev. (2):2008. CD004284
25. Edell ES, Cortese DA. Photodynamic therapy: its use in the management of bronchogenic carcinoma. Clin Chest Med. 1995;16:455-463.
26. Moghissi K, Dixon K, Stringer M, et al. The place of bronchoscopic photodynamic therapy in advanced unresectable lung cancer: experience of 100 cases. Eur J Cardiothorac Surg. 1999;15:1-6.
27. Vergnon JM, Schmitt T, Alamartine E, et al. Initial combined cryotherapy and irradiation for unresectable non-small cell lung cancer: preliminary results. Chest. 1992;102:1436-1440.
28. Kono M, Yahagi N, Kitahara M, et al. Cardiac arrest associated with use of an argon beam coagulator during laparoscopic cholecystectomy. Br J Anaesth. 2001;87:644-646.
29. Reddy C, Majid A, Michaud G, et al. Gas embolism following bronchoscopic argon plasma coagulation: a case series. Chest. 2008;134:1066-1069.
30. Saad CP, Murthy S, Krizmanich G, et al. Self expandable metallic airway stents and flexible bronchoscopy: long-term outcomes analysis. Chest. 2003;124:1993-1999.
31. Jett JR, Schild SE, Keith RL, et al. American College of Chest Physicians. Treatment of non-small cell lung cancer, stage IIIB: ACCP evidence-based clinical practice guidelines (2nd edition). Chest. 2007;132:266S-276S.
32. Slawson RG, Scott RM. Radiation therapy in bronchogenic carcinoma. Radiology. 1979;132:175-176.
33. Eichenhorn MS, Kvale PA, Miks VM, et al. Initial combination therapy with YAG laser photoresection and irradiation for inoperable non-small cell carcinoma of the lung. Chest. 1986;89:782.
34. Santos RS, Raftopoulos Y, Keenan RJ, et al. Bronchoscopic palliation of primary lung cancer: single or multimodality therapy? Surg Endosc. 2004;18:931-936.
35. McMahon CC, Rainey L, Fulton B, et al. Central airway compression: anaesthetic and intensive care consequences. Anaesthesia. 1997;52:158-162.
36. Pullerits J, Holzman R. Anaesthesia for patients with mediastinal masses. Can J Anaesth. 1989;36:681-688.
37. Perrin G, Colt HG, Martin C, et al. Safety of interventional rigid bronchoscopy using intravenous anesthesia and spontaneous assisted ventilation: a prospective study. Chest. 1992;102:1526-1530.
38. Witt C, Dinges S, Schmidt B, et al. Temporary tracheobronchial stenting in malignant stenoses. Eur J Cancer. 1997;33:204-208.
39. Matsuo T, Colt HG. Evidence against routine scheduling of surveillance bronchoscopy after stent insertion. Chest. 2000;118:1455-1459.
40. Scagliotti GV, Parikh P, von Pawel J, et al. Phase III study comparing cisplatin plus gemcitabine with cisplatin plus pemetrexed in chemotherapy-naïve patients with advanced non-small-cell lung cancer. J Clin Oncol. 2008;26:3543-3551.
41. Travis WD, Brambilla E, Noguchi M, et al. International Association for the Study of Lung Cancer/American Thoracic Society/European Respiratory Society International multidisciplinary classification of adenocarcinoma. J Thorac Oncol. 2011;6:244-285.
42. Mok T, Wu YL, Throngprasert S, et al. Gefitinib or carboplatin—paclitaxel in pulmonary adenocarcinoma. N Engl J Med. 2009;361:947-957.
43. Kwak EL, Bang YJ, Camidge DR, et al. Anaplastic lymphoma kinase in non-small-cell lung cancer. N Engl J Med. 2010;363:1693-1703.
44. Hanna N, Neubauer M, Yiannoutsos C, et al. Phase III study of cisplatin, etoposide and concurrent chest radiation with or without consolidation docetaxel in patients with inoperable stage III non-small-cell lung cancer: the Hoosier Oncology Group and US Oncology. J Clin Oncol. 2008;26:5755-5760.
45. Albain KS, Swann RS, Rusch V, et al. Radiotherapy plus chemotherapy with or without surgical resection for stage III non-small-cell lung cancer: a phase III randomized controlled trial. Lancet. 2009;374:379-386.