144 Rickettsial Diseases
Proteobacteria are small gram-negative obligate intracellular organisms that can be divided into two classes: Alphaproteobacteria including Rickettsiaceae (genus Rickettsia) and Anaplasmataceae (with four genera: Ehrlichia, Anaplasma, Neorickettsia, and Wolbachia), and Gammaproteobacteria that include Coxiellaceae (genus Coxiella).1
The Rickettsia genus is divided into the spotted fever group (SFG), which comprises about 15 different species of human pathogens, the typhus group, and the scrub typhus group.2 The spotted fever group includes arthropod-borne diseases and comprises mainly Rickettsia rickettsii, the agent of Rocky Mountain spotted fever, and Rickettsia conorii, the agent of Mediterranean spotted fever.2 The typhus group comprises Rickettsia prowazekii, causing louse-borne epidemic typhus, and Rickettsia typhi, the agent of the fleaborne murine typhus. The scrub typhus group includes Orientia tsutsugamushi, a mite-borne disease.2 Part of the clinical manifestations and sequelae associated with most human rickettsioses are due to the bacteria’s affinity for the blood vessels’ endothelium, leading to damage to the vascular endothelium, triggering vascular inflammation, and compromising vascular permeability.3,4 Exceptions are Rickettsia akari and O. tsutsugamushi, which invade and multiply in the monocytic cells.4
Ehrlichioses are zoonoses increasingly recognized as human pathogens. The human pathogens of this family, depending on the causative species, invade various target cells of the hematopoietic and lymphoreticular systems.4 Coxiella burnetii, the agent of Q fever, infects many mammal species, including humans. The clinical presentation and evolution of Q fever seem to be related to host immune response, especially to tumor necrosis factor (TNF)-α and IL-10 production by stimulated monocytes.4,5 The ability of macrophages to kill the organisms and the clinical presentation of infection seem to depend on the immune status of the patient.4
 Rickettsial Diseases
Rickettsial Diseases
Spotted Fever Group
Rickettsia rickettsii is the causative agent of Rocky Mountain spotted fever (RMSF), an arthropod-borne disease, transmitted by Dermacentor ticks.2,6,7 RMSF occurs mainly in rural and suburban locations throughout North America, Central America, and parts of South America (Colombia, Bolivia, Brazil).8 The disease is highly seasonal, with the highest incidence during late spring and summer months.8 After a 2- to 14-day incubation period, patients typically develop fever, myalgia, and severe headaches.4 The inoculation eschar is rarely found. The major diagnostic sign, the petechial rash (Figure 144-1), usually appears 3 to 5 days after the onset of fever, although older patients and black patients might not develop the rash.4,9 The rash is usually first noted around the wrists and ankles, and then involves the palms and soles, with centripetal progression.4,8,9 Because R. rickettsii produces small-vessel injury, patients can present with other symptoms such as seizures, focal neurologic deficits, transient deafness, meningoencephalitis, gastrointestinal symptoms (abdominal pain and tenderness mimicking acute abdomen), myocarditis, pericarditis, and pneumonia.4,8 Despite widespread endothelial damage and microangiopathic thrombosis in some cases, fulminant disseminated intravascular coagulopathy (DIC) is rarely seen.8 However, fulminant RMSF has been associated with older age, black males with glucose-6-phosphate dehydrogenase (G6PD) deficiency, and possibly with alcoholism.4

Figure 144-1 Child’s right hand and wrist displaying the characteristic spotted rash of Rocky Mountain spotted fever.
(Courtesy Public Health Image Library, Centers for Disease Control and Prevention.)
Rickettsia conorii is the causative agent of several infections designated by geographic names and differentiated by serologic techniques: Marseilles fever, Mediterranean spotted fever (boutonneuse fever), Kenya tick typhus, Israeli tick typhus, Astrakhan spotted fever, and Indian tick typhus.4,10 Several serotypes merit mention:
Rickettsia akari, the etiologic agent of rickettsialpox or smallpox rickettsia, is transmitted by Allodermanyssus sanguineus.2 One week after a mite bite, a vesicle appears, then dries and leaves a black eschar (Figure 144-2). The typical presentation of a patient with rickettsialpox is fever, papular or vesicular rash, and eschar.12 The rash does not involve the palms and soles; tender lymphadenopathy is commonly found on physical examination.12,13

Figure 144-2 Rickettsialpox early lesion.
(Courtesy Dr. Daniel Caplivski, Division of Infectious Diseases, Mount Sinai School of Medicine.)
Rickettsia africae, transmitted in sub-Saharan Africa and West Indies by Amblyomma ticks, causes African tick bite fever.14 The disease is described mainly in people who hunted or traveled in a bushy area in southern Africa.14 In a high proportion of cases, several inoculation eschars (Figure 144-3) can be seen; patients often have lymphadenitis in the regions that drain the eschars.14 One week after the tick bite, 46% of patients develop fever, headache, myalgia, and a rash, which can be vesicular.14 The evolution is much milder than Mediterranean spotted fever.14

Figure 144-3 Eschar (tache noir) in a patient with Rickettsia africae.
(Courtesy Dr. Daniel Caplivski, Division of Infectious Diseases, Mount Sinai School of Medicine.)
Rickettsia parkeri infection, transmitted by Amblyomma maculatum, has been recently documented in the eastern coastal states of the United States.15 Patients present approximately 1 week after a tick bite with fever, myalgia, malaise, headache, and a maculopapular eruption that may involve the palms or soles; an eschar can be found in the majority of cases.15 R. parkeri infection seems to be a milder illness than RMSF.15
Rickettsia slovaca causes tickborne lymphadenopathy, also known as TIBOLA, a disease common in Europe and transmitted by Dermacentor marginatus ticks during winter and early spring.2,6,16–18 This disease is more prevalent in children and women; it is characterized by the presence of an eschar in the scalp and enlarged, tender, draining lymph nodes.16,18 Fever and rash are rarely observed. Postinfectious asthenia and residual alopecia at the site of the tick bite have been reported.16,18
Rickettsia helvetica has been isolated from Ixodes ricinus ticks in many European and Asian countries.19,20 The disease can be mild or self-limited with associated fever, headache, and myalgia, or it can have a more severe clinical presentation.17,19–21 Cases of fever without rash or eschar have also been reported.19
Rickettsia aeschlimannii has been isolated from Hyalomma marginatum in Africa, Corsica, and Spain and is responsible for a disease similar to Mediterranean spotted fever.22
Rickettsia australis, the etiologic agent of Queensland tick typhus, is transmitted by Ixodes holocyclus in Australia.2,23 Patients present with a rash (which can be vesicular), an inoculation eschar, and regional lymphadenopathy.23 The evolution is mild.23
Rickettsia honei causes Flinders Island spotted fever, found in continental eastern Australia and probably in Thailand.2,6,24 It is a febrile illness associated with an erythematous rash and headache; an eschar is found in 25% of patients, whereas regional adenopathy occurs in 55% of patients.2,6 R. honei subsp. marmionii, or R. marmionii, has more recently been described to cause an acute febrile illness associated with headache, myalgia, arthralgia, cough, maculopapular or petechial rash, pharyngitis, eschar, and adjacent lymphadenopathy.25,26 It has also been associated with chronic illness, but it is unclear whether the bacteria are responsible for any of the chronic symptoms or whether they are just a marker of increased immunosuppression.26
Rickettsia japonica causes Japanese or Oriental spotted fever, and it is transmitted by Haemaphysalis longicornis and Dermacentor taiwanensis in Japan and in eastern China.27–29 Patients present with fever, headache, inoculation eschar, adjacent adenopathy, and a maculopapular rash.2,6,30 Meningoencephalitis and even fulminant cases complicated by DIC and death have been reported.27–31
Rickettsia sibirica, the agent of Siberian tick typhus, is transmitted by Dermacentor marginatus and Haemaphysalis concinna.4,32 The disease has been described in Siberia and China.4 After 1 week of incubation, an ulcerated necrotic lesion appears at the inoculation site, often accompanied by regional lymphadenopathy.
Rickettsia mongolotimonae, related to R. sibirica, is transmitted by the Hyalomma asiaticum tick in Mongolia, sub-Saharan Africa, and southern Europe.33–35 The main clinical manifestation is lymphangitis associated with an inoculation eschar and satellite lymphadenopathy.33–35 Patients present with fever, severe headache, and a discrete rash.33–36
Rickettsia felis causes fleaborne spotted fever and is transmitted by the cat flea, Ctenocephalides felis; it has been documented worldwide.4,21 The disease is characterized by fever, maculopapular rash, and headache.37–39 Eschar and gastrointestinal and neurologic signs are not common.39
Typhus Group
Rickettsia typhi, the agent of murine typhus or endemic typhus, is transmitted through scratching contaminated pruritic lesions after rat flea bites.2,40 Murine typhus has been diagnosed worldwide and is prevalent in tropical and subtropical seaboard regions.41 After 1 to 2 weeks’ incubation, the disease abruptly begins with fever, nausea, myalgias, arthralgias, and headache.42–45 Gastrointestinal symptoms and a maculopapular rash that starts on the trunk, spreads peripherally, and spares the palms and soles develop later in the course of the disease.42,45 A third of patients can develop respiratory symptoms.4 Neurologic symptoms can be present, ranging from confusion and stupor to seizures and coma in severe forms.4 Severe forms of disease are described in males of African descent with G6PD deficiency and in the elderly, especially when the diagnosis is delayed; such patients can present with central nervous system abnormalities, pulmonary compromise, as well as hepatic and renal dysfunction.42,45 Splenic rupture has been reported with acute infection, patients presenting with acute abdomen.46–48 Prognosis is usually favorable, with a low fatality rate.45
Rickettsia prowazekii, the etiologic agent of epidemic typhus or exanthematic typhus, is transmitted by the human body louse, Pediculus humanus corporis (Figure 144-4).2,40,49 The human body louse lives in clothes and multiplies rapidly when cold weather and lack of hygiene allow (during war, in poor countries, and in the homeless population in developed countries).40,49 This bacterium is a potential warfare agent and has been classified in category B of biological agents by the Centers for Disease Control and Prevention (CDC).50 The disease begins abruptly with fever and headache.51 The presence of myalgia, arthralgia, and constitutional symptoms are variable.51 In more than one-third of patients, the rash can be macular, petechial, and even purpuric; the lesions are distributed mostly on the trunk and may spread centrifugally to involve the extremities; rarely, lesions are found on the soft palate and conjunctiva, but not on the face, palms, and soles; eschars are absent.51 Neurologic involvement such as delirium, stupor, confusion, and even coma is common.51 Brill-Zinsser disease, a milder form of typhus, is diagnosed during the convalescent period if the bacteria is not completely eradicated and infection persists subclinically.51,52 It is frequently underdiagnosed because the rash as well as a history of recent exposure can be lacking.51,52 The prognosis is good.

Figure 144-4 Body louse, Pediculus humanus var. corporis, as it was obtaining a blood-meal from a human host.
(Courtesy Public Health Image Library, Centers for Disease Control and Prevention).
Orientia tsutsugamushi causes scrub typhus, or tsutsugamushi disease; it is transmitted by the bite of mite larvae.40 The disease occurs in Japan, eastern Australia, eastern Russia, China, and the Indian subcontinent, mainly in autumn and spring.53 Approximately 1 week after the bite, patients present with fever, headaches, and myalgias.54 An eschar may be observed in 50% of patients and is often associated with adjacent lymphadenopathy.54 The rash is macular, faint, and transient and can be missed.4 Neurologic symptoms are relatively common and vary from confusion to delirium and coma.54 Severe forms can progress to septic shock.55 Relapses can occur and are less severe than the first episode.55
Diagnosis
The leukocyte count can be within normal limits, but a leukopenia can be observed.56 Thrombocytopenia can occur and may be marked in severe cases. Anemia can also be present, especially when hemolysis is observed (frequently in patients with G6PD deficiency).56 Coagulopathy, with decrease in clotting factors (including fibrinogen) and prolonged coagulation times, may contribute to bleeding. C-reactive protein and hepatic enzyme levels can be increased.56 Hyponatremia and hypocalcemia, as well as increased lactate dehydrogenase and creatine phosphokinase levels, usually reflect the severity of the disease and organ involvement.56
The diagnosis of rickettsioses is based on serology.57 Rickettsial antibodies can be detected by several serologic tests which have different sensitivities and specificities: complement fixation,58 indirect hemagglutination,59 latex agglutination,60 enzyme-linked immunosorbent assay (ELISA),61 immunoperoxidase assay,62 and immunofluorescence assay (IFA).63 Not all serologic tests differentiate between immunoglobulins (ig)IgG and IgM or are specific enough for the diagnosis of different spotted fever–group Rickettsiae.64 IFA is regarded as the gold standard for serologic diagnosis of rickettsial infections; its sensitivity and specificity are highest among the diagnostic methodologies, and it is able to differentiate between IgG and IgM.60,64–66 Two sera samples should be tested because the early serum is often negative. A cutoff value of 1/64 for total immunoglobulins and 1/32 for specific IgM is usually required for the diagnosis.64 Cross-reactive antibodies have been observed with infections caused by Ehrlichia, Bartonella, Legionella, and Proteus. A cross-adsorption test is used to discriminate cross-reacting antibodies between two or more antigens, but the technique is limited by the large amount of antigen needed.64 Western immunoblot assay is the most specific and sensitive serologic assay and is used for epidemiologic purposes and confirmation of serologic diagnoses obtained by conventional tests.64
In skin biopsies, preferably from petechial lesions and eschar, the bacteria can be detected before seroconversion occurs. Skin biopsies can also be used for retrospective diagnosis.2,64 Immunofluorescence and immunoperoxidase techniques can be performed on frozen or fixed samples as well as on paraffin-embedded material.64
Skin biopsy specimens, peripheral white blood cells, or suspected arthropods may be used for polymerase chain reaction (PCR) diagnosis. PCR is a highly useful tool for the diagnosis of rickettsioses, but the sensitivity of the usual PCR amplification with clinical specimens seems to be variable.67 In an effort to improve rickettsial DNA detection and to avoid false-positive results, a new technique called suicide PCR has been introduced that is more sensitive and specific than traditional methods.67
The isolation of rickettsiae can be performed from human samples (decanted plasma or skin biopsies, ideally from the eschar) and from arthropods.64 Culture is restricted to specialized laboratories with biohazard and cell culture facilities. Usually, culture of rickettsiae takes 3 to 7 days.64 This technique is fundamental for the identification of new rickettsial pathogens.
Treatment
Doxycycline is the treatment of choice for rickettsioses.68 It can be prescribed in adults and children,69 but not in pregnant women and patients with allergy to tetracycline or related antibiotics. The fever typically subsides within 1 or 2 days after treatment is started; clinical improvement might be slower in complicated cases or critically ill patients, especially if they have multiple organ dysfunction.70 The treatment should be given orally, except in patients with gastric intolerance or coma, for whom it should be administered intravenously (IV).4 A single treatment of 200 mg of doxycycline in one day is sufficient for most of the rickettsioses (but not RMSF).4 For RMSF, scrub typhus, or the severe form of spotted fever, treatment duration is usually longer, and the recommendation is to continue doxycycline, 100 mg twice daily for 2 to 3 days after the patient becomes afebrile and until evidence of clinical improvement is noted, usually at least 7 days.4,70 The pediatric dose of doxycycline is 2.2 mg/kg body weight per dose administered twice daily (orally or IV) for children weighing less than 100 lbs (45.4 kg).70 R. akari and R. prowazekii infections are treated with doxycycline, 200 mg daily for 7 days, or with chloramphenicol as alternative treatment.4 Chloramphenicol, 50-75 mg/kg/d for 10 days, is the only available alternative to doxycycline in pregnant women and allergic patients.68 Chloramphenicol is available only in an IV form in the United States. Erythromycin has been used with success for murine typhus in several cases.44,71 Rifampin (600-900 mg daily) and azithromycin (500 mg daily) are alternative treatment for scrub typhus and can also be prescribed during pregnancy.72
Severely ill patients must be treated in intensive care units (ICUs). Fluid administration should be carefully monitored. Anemia and coagulation abnormalities should be corrected. Mechanical ventilation can be required in cases of respiratory distress. Hemodialysis may be required in patients with renal insufficiency. Antiepileptic drugs should be given to treat seizures. In cases of gangrene, amputation is sometimes necessary. Glucocorticoids have not proven beneficial.73
There is no current vaccination for rickettsial diseases, and prevention is based on the avoidance of tick, flea, and body lice bites.4 Lice are fragile, so changing and boiling clothes is effective. Repellents and/or protective garments can also be used. After possible exposure, ticks can be removed by forceps followed by skin disinfection.4
 Ehrlichioses
Ehrlichioses
Human monocytic ehrlichiosis (HME) is caused by Ehrlichia chaffeensis, which is transmitted by Amblyomma americanum, the Lone Star tick, and possibly by other ticks.74,75 This disease has only been described in the United States, mainly in rural and suburban areas, from April to September.40,76 After spreading through lymphatics and blood vessels, the bacteria can be observed in the macrophages and monocytes (Figure 144-5).77,78 The clinical picture of HME varies from mild to severe in immunocompetent patients, whereas in immunocompromised patients the disease tends to be more severe.79–83 After 1 week incubation, patients present with fever, chills, headache, myalgia, and malaise.79–83 Respiratory and gastrointestinal symptoms are present less frequently.79–83 The rash is observed in approximately a third of adults and in up to 66% of children.74,80,81 The rash involves the extremities, trunk, face and (rarely) the palms and soles; it typically occurs later in the course of disease and can be maculopapular, petechial, or diffusely erythematous.84–86 Severe complications that require ICU admission include acute lung injury with severe hypoxemia, seizures, meningoencephalitis, coagulopathy, acute renal insufficiency, myocardial failure, septic shock, and coma.79–83 The prognosis of HME depends on age, immune status, and early antibiotic treatment.4,79–83
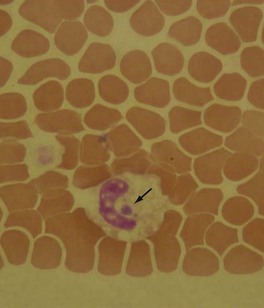
Figure 144-5 White blood cells infected with the agent of human granulocytic ehrlichiosis (Anaplasma phagocytophila).
(Courtesy Dr. Daniel Caplivski, Division of Infectious Diseases, Mount Sinai School of Medicine.)
Human granulocytic ehrlichiosis (HGE) is due to Anaplasma phagocytophila, which is transmitted by Ixodes scapularis ticks in New England and the North Central United States and by the western blacklegged tick, Ixodes pacificus, in northern California.40,56,74,76 The disease is observed in the United States and Europe from spring to fall. In the United States, the geographical distribution overlaps with that of Lyme disease and babesiosis because of the shared Ixodes tick vector74; up to 36% of patients with positive serology for A. phagocytophila also have positive serology for Borrelia burgdorferi (Lyme disease) or Babesia microti (babesiosis).87,88 After a 5- to 21-day incubation period, patients develop nonspecific manifestations including fever, chills, headache, and myalgias.89–92 Rash is rarely observed in HGE in comparison to HME.74,93 Most cases are mild, even self-limited, but serious manifestations with fatal outcome have been described.79,94 Severe cases have been described in the elderly, patients on immunosuppressive therapy, and those with chronic inflammatory illnesses or underlying malignancy.79,92,94
Canine granulocytic ehrlichiosis (CGE) is due to Ehrlichia ewingii, an uncultured bacterium transmitted by Amblyomma americanum.74 The disease occurs in immunocompromised hosts in the United States, those infected with human immunodeficiency virus (HIV), or those receiving immunosuppressive drugs.74,82 Patients present with fever, chills, headache, myalgia, and arthralgia.56,76 Rash is rare in patients with E. ewingii infection; however, it is more common in children.74,93
Canine monocytic ehrlichiosis is caused by Ehrlichia canis, which is transmitted by R. sanguineus. In 1996, a single case of infection was reported in an asymptomatic man from Venezuela who owned an infected dog.95 In 1991, an immunohistology examination identified an organism antigenically related to E. canis in tissues from a patient who died of ehrlichiosis.77 This pathogen should be considered a potential etiologic agent in compatible human illness in endemic areas.
Sennetsu neoehrlichiosis is due to Neorickettsia sennetsu. In 1953, one case was described in Japan. The bacterium was isolated from the blood, bone marrow, and lymph node of a 25-year-old man who had a mononucleosis-like disease with fever, headaches, myalgia, and anorexia.96 Sennetsu neorickettsiosis is probably underdiagnosed in southeastern Asia, as shown by the high seroprevalence in febrile patients (14%-15%) and healthy persons (17%) in Laos and in febrile patients (3%) in Thailand.97
Panola Mountain Ehrlichia and Ehrlichia ruminantium have recently been associated with human infections.98,99
Diagnosis
Leukopenia (up to 53% of cases), thrombocytopenia (up to 94% of cases), and mildly elevated hepatic enzymes are described in ehrlichioses.74,76 Diagnosis by identification of morulae (intracellular inclusion formed by clusters of bacteria) is the most rapid diagnostic method during the first week of infection, but such inclusions are rarely seen in neutrophils of patients with HGE and CGE and are even less frequent in monocytes and macrophages of patients with HME (see Figure 144-5).92 Indirect immunofluorescence antibody assay is a more sensitive diagnosis and is based on acute and convalescent serologic examination, with a fourfold rise in specific antibody titers being diagnostic.76,92,100,101 High titers (≥640) by indirect fluorescence antibody assay are also diagnostic for recent infection.101 Cross-reactivity among various species prevents definitive identification of the etiologic agent only by serology. Rapid detection and identification of Ehrlichia spp. by PCR amplification may also be performed on blood samples.101 This test is available from the CDC, state health laboratories, and research and commercial laboratories.74
Treatment
The dosage (orally or IV) for doxycycline is 100 mg twice daily for adults and 2.2 mg/kg body weight per dose twice daily for children weighing less than 100 lbs. (45.4 kg).74 The fever usually subsides within 1 to 2 days after treatment initiation; patients with more severe illness might require a longer time before clinical improvement is noted.74 The optimal duration of therapy is unclear, but it is currently recommended to treat HME for at least 3 days after fever resolution and until evidence of clinical improvement, which is usually for 5 to 7 days.74 Severe or complicated cases might require longer treatment courses.74 Patients with HGA should be treated with doxycycline for 10 to 14 days to provide appropriate length of therapy for possible co-infection with Borrelia burdogferii.74,92 Chloramphenicol may not be effective for ehrlichioses.74 Patients with mild illness due to HGA who cannot take doxycycline because of drug allergy or pregnancy can be treated with rifampin for 7 to 10 days (300 mg twice daily for adults and 10 mg/kg twice daily for children, to a maximum 300 mg per dose). Patients co-infected with Borrelia burgdorferi should also be treated with amoxicillin or cefuroxime.92 Persistence of fever for more than 2 days after initiation of doxycycline suggests the need to look for an alternative diagnosis or that the patient is co-infected with Babesia microti.92 Prevention relies on limiting exposure to tick habitats, inspection of the body for ticks after being in areas potentially infested, and removing attached ticks immediately.74 For patients who have had recent tick bites but are not ill, preventive antibiotic therapy for rickettsial infection is not indicated.74
 Q Fever
Q Fever
Q fever is caused by Coxiella burnetii and occurs worldwide except in New Zealand; humans are incidental hosts, developing an acute or chronic infection.102 The reservoir of this bacterium includes mammals, birds, and ticks.102 Humans are usually infected by aerosol from amniotic fluid, placenta, contaminated wool, or less frequently, by milk products.103 C. burnetii is a potential warfare agent and classified in category B of biological agents by the CDC.50 C. burnetii is a strict intracellular bacterium that has characteristic antigenic variations (called phase variation).104 After exposure to contaminated aerosols or products, up to 60% of patients develop asymptomatic infection diagnosed by seroconversion; 38% of cases will have self-limited disease, and only 2% necessitate hospitalization and diagnostic workup; about 0.5% of patients develop chronic Q fever.103,105,106
Patients with acute Q fever may present with a variety of symptoms that include flulike illness, pneumonia (mainly in elderly or immunocompromised patients), or acute hepatitis (mainly in younger patients).105,106 Complications associated with acute Q fever are rare and may include aseptic lymphocytic meningitis, encephalitis, encephalomyelitis, polyradiculopathy, seizures, pericarditis, myocarditis with congestive heart failure, and respiratory failure with acute respiratory distress syndrome.105 Patients infrequently present with cutaneous manifestations such as maculopapular or purpuric rash and erythema nodosum.105 Less common manifestations of acute Q fever include hemolytic anemia, thyroiditis, gastroenteritis, pancreatitis, lymphadenopathy, splenic rupture, proliferative glomerulonephritis, orchitis, and epididymitis.105 Post–Q fever chronic fatigue syndrome has also been described, and in England has been characterized by fatigue, sweats, and dyspnea on effort, while in Australia it is characterized by painful lymphadenopathy, myalgia, and arthralgia.105,107,108 In pregnant women with or without symptoms, Q fever compromises the pregnancy and can be responsible for abortion, oligoamnios, fetal death, or prematurity.109
Pregnant women, patients with cardiac abnormalities, and immunocompromised patients are at risk to progress to chronic infection.104,105,109 Chronic Q fever is defined as an infection that persists more than 6 months, with recurrent fever being the most common manifestation.105 Aneurysm or prosthetic valve infections carry a poor prognosis.105 Patients with Q fever endocarditis have chronic low-grade fever, progressive deterioration of valve function, and progressive heart failure; vegetations are rarely observed on echocardiography.105 If not diagnosed, the disease progressively worsens, and complications include cerebral emboli, hepatosplenomegaly, and glomerulonephritis.103,105 Cases of chronic osteomyelitis and cirrhosis have been also reported.105
Diagnosis
Thrombocytopenia, leucopenia, abnormal liver function tests, and elevated sedimentation rate are frequently reported.103,105 Immunologic abnormalities including elevated cryoglobulins, rheumatoid factor, anticardiolipin, and antiphospholipid antibodies may be observed, especially during chronic infection.105 Diagnosis is primarily based on serology, with the most commonly used method being the IFA with the test of phase I and phase II antigens.103 Patients seroconvert 14 days after development of symptoms.105,110 Acute Q fever is diagnosed when IgM phase II antigen titers are ≥50, IgG phase II antigen titers are ≥200, seroconversion occurs, or a fourfold increase of phase II antigen can be documented.103,105 Chronic Q fever is diagnosed when IgG to phase I antigens titer is at least 800 or IgA to phase I antigens titer is ≥ 100.105 Serology is also useful for following the clinical course of patients with acute infection and underlying disease and in those with chronic Q fever undergoing treatment.4 The other diagnostic tools are direct detection by cell culture performed in a specialized laboratory with biohazard facilities, PCR, or immunochemistry of the involved tissue (cardiac valve, liver, or blood samples).103 Liver or lymph node biopsy shows nonspecific granulomas characterized by a vacuole containing the bacteria and surrounded by a fibrinoid ring.103,105,110
Treatment
Acute Q fever can be a self-limited disease, and only symptomatic patients warrant treatment.102 In a randomized trial, tetracycline was proven to shorten fever duration.111 No clinical trials have been performed to determine the adequate length of therapy for acute Q fever; however, it is recommended to prescribe doxycycline (200 mg/d) for 3 weeks or 1 week after fever resolution.103,105 In cases with central nervous system involvement, fluoroquinolones are the drugs of choice.105,111 The new macrolides look promising for treatment of Q fever, but clinical data are limited.112–115 In patients with a valvular abnormality, it is recommended to treat acute Q fever with doxycycline (200 mg/d) and hydroxychloroquine (600 mg/d) for 12 months.116 In patients with Coxiella endocarditis, the recommended treatment is doxycycline (200 mg/d) and hydroxychloroquine (600 mg/d) for at least 18 months; IgG and IgA to phase I antigens titers should be monitored to assess the response to treatment, especially during the first year.103,105 In patients with Q fever hepatitis with slow regression of symptoms, clinical benefit has been described with the addition of prednisone to the antibiotic therapy; prednisone could be considered in patients who do not become afebrile after 3 days of antibiotic therapy and should be started at 40 mg for 48 hours, then tapered to 20 mg for 48 hours, and then 10 mg for an additional 48 hours.103 In pregnant women, cotrimoxazole (sulfamethoxazole 1600/trimethoprim 320 mg/d) should be started and continued throughout the pregnancy to decrease the risk of infection of the placenta and obstetric complications.105,109 A vaccine is available in Australia.117 Prevention of Q fever is based on veterinary control of the disease in animals.105
Key Points
Chapman AS, Bakken JS, Folk SM, Paddock CD, Bloch KC, Krusell A, et al. Diagnosis and management of tickborne rickettsial diseases: Rocky Mountain spotted fever, ehrlichioses, and anaplasmosis—United States: a practical guide for physicians and other health-care and public health professionals. Tickborne Rickettsial Diseases Working Group, CDC. MMWR Recomm Rep. 2006;55:1-27.
Wormser GP, Dattwyler RJ, Shapiro ED, Halperin JJ, Steere AC, Klempner MS, et al. The clinical assessment, treatment, and prevention of Lyme disease, human granulocytic anaplasmosis, and babesiosis: clinical practice guidelines by the Infectious Diseases Society of America. Clin Infect Dis. 2006;43:1089-1134.
Schutze GE, Buckingham SC, Marshall GS, Woods CR, Jackson MA, Patterson LE, et al. Human monocytic ehrlichiosis in children. Tick-borne Infections in Children Study (TICS) Group. Pediatr Infect Dis J. 2007;26:475-479.
Paddock CD, Finley RW, Wright CS, Robinson HN, Schrodt BJ, Lane CC, et al. Rickettsia parkeri rickettsiosis and its clinical distinction from Rocky Mountain spotted fever. Clin Infect Dis. 2008;4:1188-1196.
Mandell GL, Bennett JE, Dolin R, editors. Mandell, Douglas, and Bennett’s principles and practice of infectious diseases. 7th ed. Philadelphia: Churchill Livingstone; 2009:2495-2538.
1 Euzeby JP. List of prokaryotic names with standing in nomenclature. Available at. http://www.bacterio.cict.fr/.
2 Raoult D, Roux V. Rickettsioses as paradigms of new or emerging infectious diseases. Clin Microbiol Rev. 1997;10:694-719.
3 Sahni SK, Rydkina E. Host-cell interactions with pathogenic rickettsia species. Future Microbiol. 2009;4:323-339.
4 Mandell GL, Bennett JE, Dolin R, editors. Mandell, Douglas, and Bennett’s principles and practice of infectious diseases. 7th ed. Philadelphia: Churchill Livingstone; 2009:2399-2405.
5 Honstettre A, Imbert G, Ghigo E, et al. Dysregulation of cytokines in acute Q fever: role of interleukin-10 and tumor necrosis factor in chronic evolution of Q fever. J Infect Dis. 2003;187:956-962.
6 Raoult DOJ. Emerging rickettsioses. In: Scheld W, Craig W, Hughes J, editors. Emerging Infections. Washington, DC: ASM Press; 1999:17-31.
7 Treadwell TA, Holman RC, Clarke MJ, Krebs JW, Paddock CD, Childs JE. Rocky Mountain spotted fever in the United States, 1993-1996. Am J Trop Med Hyg. 2000;63:21-26.
8 Chen LF, Sexton DJ. What’s new in Rocky Mountain spotted fever? Infect Dis Clin North Am. 2008;22:415-432. vii-viii
9 Helmick CG, Bernard KW, D’Angelo LJ. Rocky Mountain spotted fever: clinical, laboratory, and epidemiological features of 262 cases. J Infect Dis. 1984;150:480-488.
10 Rovery C, Raoult D. Mediterranean spotted fever. Infect Dis Clin North Am. 2008;22:515-530. ix
11 Parola P, Fenollar F, Badiaga S, Brouqui P, Raoult D. First documentation of Rickettsia conorii infection (strain Indian tick typhus) in a traveler. Emerg Infect Dis. 2001;7:909-910.
12 Kass EM, Szaniawski WK, Levy H, Leach J, Srinivasan K, Rives C. Rickettsialpox in a New York City hospital, 1980 to 1989. N Engl J Med. 1994;331:1612-1617.
13 Brettman LR, Lewin S, Holzman RS, et al. Rickettsialpox: report of an outbreak and a contemporary review. Medicine (Baltimore). 1981;60:363-372.
14 Raoult D, Fournier PE, Fenollar F, et al. Rickettsia africae, a tick-borne pathogen in travelers to Sub-Saharan Africa. N Engl J Med. 2001;344:1504-1510.
15 Paddock CD, Finley RW, Wright CS, et al. Rickettsia parkeri rickettsiosis and its clinical distinction from Rocky Mountain spotted fever. Clin Infect Dis. 2008;47:1188-1196.
16 Raoult D, Lakos A, Fenollar F, Beytout J, Brouqui P, Fournier PE. Spotless rickettsiosis caused by Rickettsia slovaca and associated with Dermacentor ticks. Clin Infect Dis. 2002;34:1331-1336.
17 Nilsson K, Lindquist O, Pahlson C. Association of Rickettsia helvetica with chronic perimyocarditis in sudden cardiac death. Lancet. 1999;354:1169-1173.
18 Cazorla C, Enea M, Lucht F, Raoult D. First isolation of Rickettsia slovaca from a patient, France. Emerg Infect Dis. 2003;9:135.
19 Fournier PE, Grunnenberger F, Jaulhac B, Gastinger G, Raoult D. Evidence of Rickettsia helvetica infection in humans, eastern France. Emerg Infect Dis. 2000;6:389-392.
20 Nilsson K, Elfving K, Pahlson C. Rickettsia helvetica in patient with meningitis, Sweden, 2006. Emerg Infect Dis. 2010;16:490-492.
21 Raoult D, La Scola B, Enea M, et al. A flea-associated rickettsia pathogenic for humans. Emerg Infect Dis. 2001;7:73-81.
22 Raoult D, Fournier PE, Abboud P, Caron F. First documented human Rickettsia aeschlimannii infection. Emerg Infect Dis. 2002;8:748-749.
23 Sexton DJ, Dwyer B, Kemp R, Graves S. Spotted fever group rickettsial infections in Australia. Rev Infect Dis. 1991;13:876-886.
24 Dumler JS, Barbet AF, Bekker CP, et al. Reorganization of genera in the families Rickettsiaceae and Anaplasmataceae in the order Rickettsiales: unification of some species of Ehrlichia with Anaplasma, Cowdria with Ehrlichia and Ehrlichia with Neorickettsia, descriptions of six new species combinations and designation of Ehrlichia equi and “HGE agent” as subjective synonyms of Ehrlichia phagocytophila. Int J Syst Evol Microbiol. 2001;51:2145-2165.
25 Unsworth NB, Stenos J, Graves SR, et al. Flinders island spotted fever rickettsioses caused by “marmionii” strain of Rickettsia honei, eastern Australia. Emerg Infect Dis. 2007;13:566-573.
26 Graves S, Unsworth N, Stenos J. Rickettsioses in Australia. Ann N Y Acad Sci. 2006;1078:74-79.
27 Araki M, Takatsuka K, Kawamura J, Kanno Y. Japanese spotted fever involving the central nervous system: two case reports and a literature review. J Clin Microbiol. 2002;40:3874-3876.
28 Kodama K, Senba T, Yamauchi H, et al. Fulminant Japanese spotted fever definitively diagnosed by the polymerase chain reaction method. J Infect Chemother. 2002;8:266-268.
29 Iwasaki H, Mahara F, Takada N, Fujita H, Ueda T. Fulminant Japanese spotted fever associated with hypercytokinemia. J Clin Microbiol. 2001;39:2341-2343.
30 Kondo M, Nishii M, Gabazza EC, Kurokawa I, Akachi S. Nine cases of Japan spotted fever diagnosed at our hospital in 2008. Int J Dermatol. 2010;49:430-434.
31 Nomura T, Fujimoto T, Ebisutani C, Horiguchi H, Ando S. The first fatal case of Japanese spotted fever confirmed by serological and microbiological tests in Awaji Island, Japan. Jpn J Infect Dis. 2007;60:241-243.
32 Tarasevich IV, Mediannikov OY. Rickettsial diseases in Russia. Ann N Y Acad Sci. 2006;1078:48-59.
33 Pretorius AM, Birtles RJ. Rickettsia mongolotimonae infection in South Africa. Emerg Infect Dis. 2004;10:125-126.
34 Psaroulaki A, Germanakis A, Gikas A, Scoulica E, Tselentis Y. Simultaneous detection of “Rickettsia mongolotimonae” in a patient and in a tick in Greece. J Clin Microbiol. 2005;43:3558-3559.
35 Aguirrebengoa K, Portillo A, Santibanez S, Marin JJ, Montejo M, Oteo JA. Human Rickettsia sibirica mongolitimonae infection, Spain. Emerg Infect Dis. 2008;14:528-529.
36 Fournier PE, Tissot-Dupont H, Gallais H, Raoult DR. Rickettsia mongolotimonae: a rare pathogen in France. Emerg Infect Dis. 2000;6:290-292.
37 Zavala-Velazquez J, Ruiz-Sosa J, Sanchez-Elias R, et al. Rickettsia felis in Yucatan. Lancet. 2000;9235:1079-1080.
38 Richter J, Fournier PE, Petridou J, Haussinger D, Raoult D. Rickettsia felis infection acquired in Europe and documented by polymerase chain reaction. Emerg Infect Dis. 2002;8:207-208.
39 Renvoise A, Joliot AY, Raoult D. Rickettsia felis infection in man, France. Emerg Infect Dis. 2009;15:1126-1127.
40 Kelly DJ, Richards AL, Temenak J, Strickman D, Dasch GA. The past and present threat of rickettsial diseases to military medicine and international public health. Clin Infect Dis. 2002;34:S145-S169.
41 Azad AF, Radulovic S, Higgins JA, Noden BH, Troyer JM. Flea-borne rickettsioses: ecologic considerations. Emerg Infect Dis. 1997;3:319-327.
42 Dumler JS, Taylor JP, Walker DH. Clinical and laboratory features of murine typhus in south Texas, 1980 through 1987. JAMA. 1991;266:1365-1370.
43 Bernabeu-Wittel M, Pachon J, Alarcon A, et al. Murine typhus as a common cause of fever of intermediate duration: a 17-year study in the south of Spain. Arch Intern Med. 1999;159:872-876.
44 Koliou M, Christoforou C, Soteriades ES. Murine typhus in pregnancy: a case report from Cyprus. Scand J Infect Dis. 2007;39:625-628.
45 Civen R, Ngo V. Murine typhus: An unrecognized suburban vectorborne disease. Clin Infect Dis. 2008;46:913-918.
46 Radin R, Hirbawi IA, Henderson RW. Splenic involvement in endemic (murine) typhus: CT findings. Abdom Imaging. 2001;26:298-299.
47 Fergie J, Purcell K. Spontaneous splenic rupture in a child with murine typhus. Pediatr Infect Dis J. 2004;23:1171-1172.
48 McKelvey SD, Braidly PC, Stansby GP, Weir WR. Spontaneous splenic rupture associated with murine typhus. J Infect. 1991;22:296-297.
49 Raoult D, Roux V. The body louse as a vector of reemerging human diseases. Clin Infect Dis. 1999;29:888-911.
50 Centers for Disease Control and Prevention. Bioterrorism Agents/Diseases. Available at. http://www.bt.cdc.gov/agent/agentlist-category.asp#a.
51 Bechah Y, Capo C, Mege JL, Raoult D. Epidemic typhus. Lancet Infect Dis. 2008;8:417-426.
52 Green CR, Fishbein D, Gleiberman I. Brill-Zinsser: Still with us. JAMA. 1990;264:1811-1812.
53 Kelly DJ, Fuerst PA, Ching WM, Richards AL. Scrub typhus: The geographic distribution of phenotypic and genotypic variants of Orientia tsutsugamushi. Clin Infect Dis. 2009;48(Suppl 3):S203-S230.
54 Berman SJ, Kundin WD. Scrub typhus in South Vietnam. A study of 87 cases. Ann Intern Med. 1973;79:26-30.
55 Treanor JJ, Dolin R. Noroviruses and other caliciviruses. 6th ed. Mandell GL, Bennett JE, Dolin R, editors. Principles and Practice of Infectious Diseases. vol. 2. New York: Elsevier; 2005:2194-2201.
56 Parola P, Raoult D. Ticks and tickborne bacterial diseases in humans: An emerging infectious threat. Clin Infect Dis. 2001;32:897-928.
57 Fenollar F, Raoult D. Diagnosis of rickettsial diseases using samples dried on blotting paper. Clin Diagn Lab Immunol. 1999;6:483-488.
58 Philip RN, Casper EA, MacCormack JN, et al. A comparison of serologic methods for diagnosis of Rocky Mountain spotted fever. Am J Epidemiol. 1977;105:56-67.
59 Anacker RL, Philip RN, Thomas LA, Casper EA. Indirect hemagglutination test for detection of antibody to rickettsia rickettsii in sera from humans and common laboratory animals. J Clin Microbiol. 1979;10:677-684.
60 Kaplan JE, Schonberger LB. The sensitivity of various serologic tests in the diagnosis of Rocky Mountain spotted fever. Am J Trop Med Hyg. 1986;35:840-844.
61 Keysary A, Strenger C. Use of enzyme-linked immunosorbent assay techniques with cross-reacting human sera in diagnosis of murine typhus and spotted fever. J Clin Microbiol. 1997;35:1034-1035.
62 Suto T. Rapid and accurate serologic diagnosis of tsutsugamushi disease in Japan employing the immunoperoxidase reaction. In: Kazar J, editor. Rickettsiae and rickettsial diseases. Bratislava, Slovakia: Publishing House of the Slovak Academy of Sciences; 1985:444-452.
63 La Scola B, Raoult D. Serologic diagnosis of rickettsiosis. In: Raoult D, Brouqui P, editors. Rickettsiae and rickettsial diseases at the turn of the third millennium. Paris: Elsevier; 1999:320-329.
64 La Scola B, Raoult D. Laboratory diagnosis of rickettsioses: current approaches to diagnosis of old and new rickettsial diseases. J Clin Microbiol. 1997;35:2715-2727.
65 Newhouse VF, Shepard CC, Redus MD, Tzianabos T, McDade JE. A comparison of the complement fixation, indirect fluorescent antibody, and microagglutination tests for the serological diagnosis of rickettsial diseases. Am J Trop Med Hyg. 1979;28:387-395.
66 Philip RN, Casper EA, Burgdorfer W, Gerloff RK, Hughes LE, Bell EJ. Serologic typing of rickettsiae of the spotted fever group by microimmunofluorescence. J Immunol. 1978;121:1961-1968.
67 Fournier PE, Raoult D. Suicide PCR on skin biopsy specimens for diagnosis of rickettsioses. J Clin Microbiol. 2004;42:3428-3434.
68 Holman RC, Paddock CD, Curns AT, Krebs JW, McQuiston JH, Childs JE. Analysis of risk factors for fatal rocky mountain spotted fever: Evidence for superiority of tetracyclines for therapy. J Infect Dis. 2001;184:1437-1444.
69 Purvis JJ, Edwards MS. Doxycycline use for rickettsial disease in pediatric patients. Pediatr Infect Dis J. 2000;19:871-874.
70 Chapman AS, Bakken JS, Folk SM, et al. Diagnosis and management of tickborne rickettsial diseases: Rocky Mountain spotted fever, ehrlichioses, and anaplasmosis–United States: a practical guide for physicians and other health-care and public health professionals. MMWR Recomm Rep. 2006;55:1-27.
71 Graves SR, Banks J, Dwyer B, King GK. A case of murine typhus in Queensland. Med J Aust. 1992;156:650-651.
72 Phimda K, Hoontrakul S, Suttinont C, et al. Doxycycline versus azithromycin for treatment of leptospirosis and scrub typhus. Antimicrob Agents Chemother. 2007;51:3259-3263.
73 Breitschwerdt EB, Davidson MG, Hegarty BC, Papich MG, Grindem CB. Prednisolone at anti-inflammatory or immunosuppressive dosages in conjunction with doxycycline does not potentiate the severity of Rickettsia rickettsii infection in dogs. Antimicrob Agents Chemother. 1997;41:141-147.
74 Bakken JS, Dumler JS. Clinical diagnosis and treatment of human granulocytotropic anaplasmosis. Ann N Y Acad Sci. 2006;1078:236-247.
75 Dumler JBJ. Ehrlichial diseases of humans: emerging tick-borne infections. Clin Infect Dis. 1996;20:1102-1110.
76 Dumler JWD. Tick borne ehrlichioses. Lancet Infect Dis. 2001:21-28.
77 Dumler JS, Brouqui P, Aronson J, Taylor JP, Walker DH. Identification of Ehrlichia in human tissue. N Engl J Med. 1991;325:1109-1110.
78 Dumler JS, Dawson JE, Walker DH. Human ehrlichiosis: hematopathology and immunohistologic detection of Ehrlichia chaffeensis. Hum Pathol. 1993;24:391-396.
79 Olano JP, Walker DH. Human ehrlichioses. Med Clin North Am. 2002;86:375-392.
80 Eng TR, Harkess JR, Fishbein DB, et al. Epidemiologic, clinical, and laboratory findings of human ehrlichiosis in the United States, 1988. JAMA. 1990;264:2251-2258.
81 Schutze GE, Buckingham SC, Marshall GS, et al. Human monocytic ehrlichiosis in children. Pediatr Infect Dis J. 2007;26:475-479.
82 Paddock CD, Folk SM, Shore GM, et al. Infections with Ehrlichia chaffeensis and Ehrlichia ewingii in persons coinfected with human immunodeficiency virus. Clin Infect Dis. 2001;33:1586-1594.
83 Thomas LD, Hongo I, Bloch KC, Tang YW, Dummer S. Human ehrlichiosis in transplant recipients. Am J Transplant. 2007;7:1641-1647.
84 Paddock CD, Childs JE. Ehrlichia chaffeensis: a prototypical emerging pathogen. Clin Microbiol Rev. 2003;16:37-64.
85 Fichtenbaum CJ, Peterson LR, Weil GJ. Ehrlichiosis presenting as a life-threatening illness with features of the toxic shock syndrome. Am J Med. 1993;95:351-357.
86 Harkess JR. Ehrlichiosis. Infect Dis Clin North Am. 1991;5:37-51.
87 Magnarelli LA, Dumler JS, Anderson JF, Johnson RC, Fikrig E. Coexistence of antibodies to tick-borne pathogens of babesiosis, ehrlichiosis, and Lyme borreliosis in human sera. J Clin Microbiol. 1995;33:3054-3057.
88 Aguero-Rosenfeld ME, Donnarumma L, Zentmaier L, et al. Seroprevalence of antibodies that react with Anaplasma phagocytophila, the agent of human granulocytic ehrlichiosis, in different populations in Westchester County, New York. J Clin Microbiol. 2002;40:2612-2615.
89 Bakken JS, Krueth J, Wilson-Nordskog C, Tilden RL, Asanovich K, Dumler JS. Clinical and laboratory characteristics of human granulocytic ehrlichiosis. JAMA. 1996;275:199-205.
90 Aguero-Rosenfeld ME, Horowitz HW, Wormser GP, et al. Human granulocytic ehrlichiosis: a case series from a medical center in New York state. Ann Intern Med. 1996;125:904-908.
91 Blanco JR, Oteo JA. Human granulocytic ehrlichiosis in Europe. Clin Microbiol Infect. 2002;8:763-772.
92 Wormser GP, Dattwyler RJ, Shapiro ED, et al. The clinical assessment, treatment, and prevention of Lyme disease, human granulocytic anaplasmosis, and babesiosis: Clinical practice guidelines by the infectious diseases society of America. Clin Infect Dis. 2006;43:1089-1134.
93 Bakken J, Dumler J. Ehrlichiosis and anaplasmosis. Infect Med. 2004;21:433-451.
94 Bakken JS, Dumler JS. Human granulocytic ehrlichiosis. Clin Infect Dis. 2000;31:554-560.
95 Perez M, Rikihisa Y, Wen B. Ehrlichia canis-like agent isolated from a man in Venezuela: antigenic and genetic characterization. J Clin Microbiol. 1996;34:2133-2139.
96 Misao T, Kobayashi Y. Studies on infectious mononucleosis (glandular fever): I. Isolation of etiologic agent from blood, bone marrow, and lymph node of a patient with infectious mononucleosis by using mice. Kyushu J Med Sci. 1955;6:145-152.
97 Newton PN, Rolain JM, Rasachak B, et al. Sennetsu neorickettsiosis: a probable fish-borne cause of fever rediscovered in Laos. Am J Trop Med Hyg. 2009;81:190-194.
98 Reeves WK, Loftis AD, Nicholson WL, Czarkowski AG. The first report of human illness associated with the panola mountain ehrlichia species: A case report. J Med Case Reports. 2008;2:139.
99 Louw M, Allsopp MT, Meyer EC. Ehrlichia ruminantium, an emerging human pathogen–a further report. S Afr Med J. 2005;95:948. 950
100 Bakken JS, Haller I, Riddell D, Walls JJ, Dumler JS. The serological response of patients infected with the agent of human granulocytic ehrlichiosis. Clin Infect Dis. 2002;34:22-27.
101 Aguero-Rosenfeld ME. Diagnosis of human granulocytic ehrlichiosis: state of the art. Vector Borne Zoonotic Dis. 2002;2:233-239.
102 Tissot-Dupont H, Raoult D. Q fever. Infect Dis Clin North Am. 2008;22:505-514. ix
103 Maurin M, Raoult D. Q fever. Clin Microbiol Rev. 1999;12:518-553.
104 Raoult D, Marrie T, Mege J. Natural history and pathophysiology of Q fever. Lancet Infect Dis. 2005;5:219-226.
105 Million M, Lepidi H, Raoult D. Q fever: Current diagnosis and treatment options. Med Mal Infect. 2009;39:82-94.
106 Raoult D, Tissot-Dupont H, Foucault C, et al. Q fever 1985-1998. clinical and epidemiologic features of 1,383 infections. Medicine (Baltimore). 2000;79:109-123.
107 Ayres JG, Flint N, Smith EG, et al. Post-infection fatigue syndrome following Q fever. QJM. 1998;91:105-123.
108 Marmion BP, Shannon M, Maddocks I, Storm P, Penttila I. Protracted debility and fatigue after acute Q fever. Lancet. 1996;347:977-978.
109 Raoult D, Fenollar F, Stein A. Q fever during pregnancy: diagnosis, treatment, and follow-up. Arch Intern Med. 2002;162:701-704.
110 Fournier PE, Marrie TJ, Raoult D. Diagnosis of Q fever. J Clin Microbiol. 1998;36:1823-1834.
111 Rolain JM, Maurin M, Raoult D. Bacteriostatic and bactericidal activities of moxifloxacin against Coxiella burnetii. Antimicrob Agents Chemother. 2001;45:301-302.
112 Boulos A, Rolain JM, Maurin M, Raoult D. Measurement of the antibiotic susceptibility of Coxiella burnetii using real time PCR. Int J Antimicrob Agents. 2004;23:169-174.
113 Lever MS, Bewley KR, Dowsett B, Lloyd G. In vitro susceptibility of Coxiella burnetii to azithromycin, doxycycline, ciprofloxacin and a range of newer fluoroquinolones. Int J Antimicrob Agents. 2004;24:194-196.
114 Ralph A, Markey P, Schultz R. Q fever cases in the northern territory of Australia from 1991 to 2006. Commun Dis Intell. 2007;31:222-227.
115 Cerar D, Karner P, Avsic-Zupanc T, Strle F. Azithromycin for acute Q fever in pregnancy. Wien Klin Wochenschr. 2009;121:469-472.
116 Fenollar F, Fournier PE, Carrieri MP, Habib G, Messana T, Raoult D. Risks factors and prevention of Q fever endocarditis. Clin Infect Dis. 2001;33:312-316.
117 Gidding HF, Wallace C, Lawrence GL, McIntyre PB. Australia’s national Q fever vaccination program. Vaccine. 2009;27:2037-2041.

