9 Rheumatological disease
Approach to the patient
Clinical features in musculoskeletal assessment
Drugs in rheumatology
Non-steroidal anti-inflammatory drugs (NSAIDs) (Table 9.1)
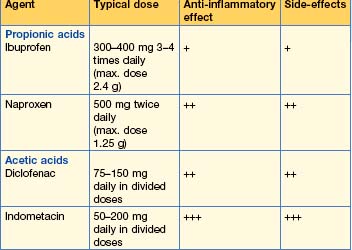
NSAIDs are inhibitors of both cyclo-oxygenase 1 and 2 isoenzymes and thereby inhibit the prostaglandin pathway (Fig. 9.1). Typical agents used for rheumatological disorders are shown in Table 9.1, although there are many others.
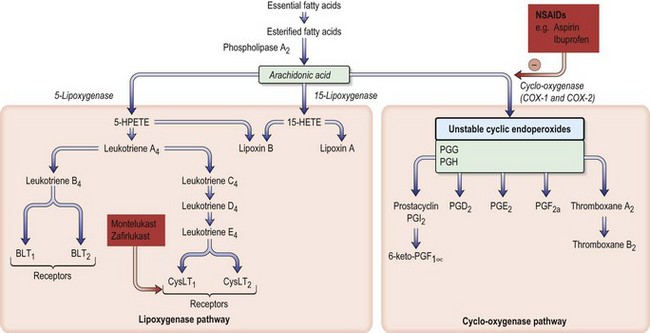
Fig. 9.1 Arachidonic acid metabolism and the effect of drugs. The sites of action of NSAIDs (e.g. aspirin, ibuprofen) are shown. The enzyme cyclo-oxygenase occurs in three isoforms: COX-1 (constitutive), COX-2 (inducible) and COX-3 (in brain). BLT, B leukotriene receptor; cysLT, cysteinyl leukotriene receptor; PG, prostaglandin.
NSAID should be used for the shortest possible time at the lowest effective dose.
Glucocorticoids
Systemic corticosteroids
These are potent anti-inflammatory agents.
Joint aspiration and injection for diagnosis and therapy (Box 9.3)
Aspiration
Aspiration should always be performed in patients with unexplained large joint effusions to obtain a diagnosis; for symptomatic relief in a patient with known arthritis; and to monitor response to treatment in an infected joint.
Box 9.3 Joint aspiration
This is a sterile procedure, which should be carried out in a clean environment.
Explain the procedure to the patient; obtain consent.
Joint injection
N.B. No more than three injections per joint should be performed in 1 year.
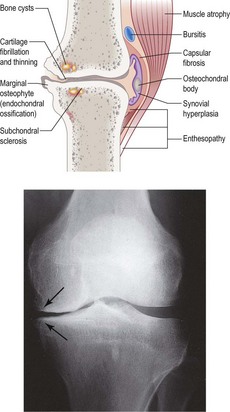
Osteoarthritis (OA)
Investigations
Management
Inflammatory arthritis
Rheumatoid arthritis (RA)
Clinical features
Investigations
Management
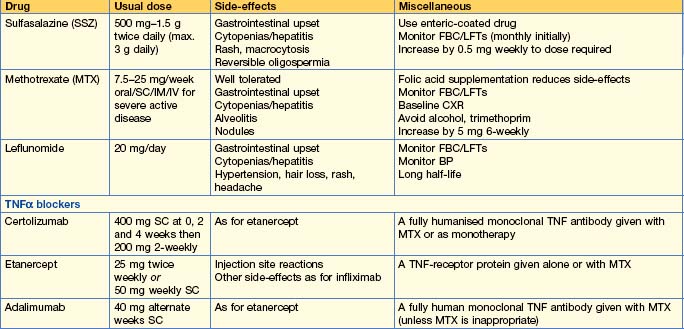
• Drugs used less commonly
Special situations
| Drug | Pregnancy | Breast feeding |
|---|---|---|
| Steroids | P | P |
| Hydroxychloroquine | P | A |
| Sulfalazine | P (stop in men 3 months before attempting conception due to oligospermia) | P |
| Methotrexate | A (stop 6 months prior to attempting conception) | A |
| Leflunomide* | A | A |
| Gold | A | A |
| Azathioprine | P | A |
| Ciclosporin | P | A |
| Anticytokine therapy | A (insufficient data) | A (insufficient data) |
| Cyclophosphamide | A | A |
| Mycophenolate | A (insufficient data) | A (insufficient data) |
| Rituximab | A | A |
P, use permissible; A, avoid use. *Because of long half-life drug elimination, treat with colestyramine 8 g 3 times daily for 11 days prior to conception or starting another DMARD.
N.B. These drugs are all potentially dangerous. Follow manufacturer’s advice.
Seronegative spondyloarthropathies
This group of conditions is characterized by:
Management
• Drug therapy
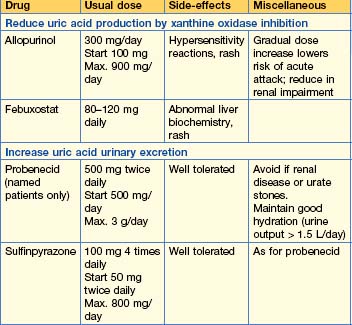
Crystal arthropathy
Gout
Clinical features
Management
Autoimmune rheumatic disorders
Systemic lupus erythematosus (SLE)
Management
• NSAIDs
Antiphospholipid syndrome (APS)
Management
Sjögren’s syndrome
Management
Management of associated features
Hydroxychloroquine 200–400 mg/day can improve arthralgia, myalgia and possibly fatigue. NSAIDs can help arthralgia. Severe manifestations, such as vasculitis, glomerulonephritis, neurological problems and interstitial lung disease, are treated in a similar way to SLE with major organ involvement (see above) using steroids (e.g. prednisolone 1 mg/kg) and immunosuppression with azathioprine, cyclophosphamide or mycophenolate (Table 9.2).
Systemic sclerosis (SS)
Management
Polymyositis/dermatomyositis
Management
Vasculitis
Large-vessel vasculitis
Giant cell arteritis (GCA)
• Treatment
Polymyalgia rheumatica (PMR)
Medium-vessel vasculitis
Polyarteritis nodosa (PAN)
Small-vessel vasculitis
Septic arthritis
Non-gonococcal septic arthritis
Management – See Chapter 20 (Emergencies in medicine p. 710)
Table 9.5 Antibiotics used in septic arthritis and osteomyelitis
| Organism | Antibiotic |
|---|---|
| Gram-positive organism (staphylococcus, streptococcus) | IV flucloxacillin 1–2 g 4 times daily and oral fusidic acid 500 mg 3 times daily If penicillin allergy — replace flucloxacillin by erythromycin 1 g IV 4 times daily or clindamycin 600 mg IV 3 times daily If MRSA suspected — use vancomycin to replace flucloxacillin |
| Gram-negative organism | Cefotaxime IV 1 g twice daily |
| No organism seen | IV flucloxacillin 1–2 g 4 times daily and oral fusidic acid 500 g 3 times daily, or cefotaxime IV 1 g twice daily in sexually active, ?gonococcus in immunosuppressed, elderly and IV drug users Penicillin allergy as above |
MRSA, meticillin-resistant Staphylococcus aureus.
Gonococcal septic arthritis
Management
Non-drug therapy is as for non-gonococcal septic arthritis but surgical drainage is rarely required.
Other types of infective arthritis
Bacteria, viruses and fungi can cause arthritis.
Osteomyelitis
Investigations
Management
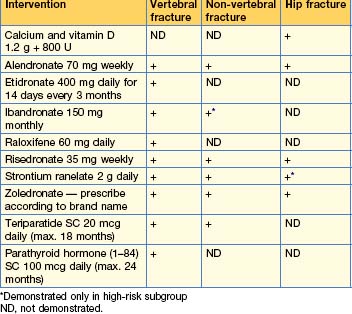
Osteoporosis
This is a skeletal disease characterized by low bone mass and micro-architectural deterioration of bone tissue with consequent susceptibility to fractures. A variety of medical conditions and steroids can predispose to osteoporosis, but in most patients the main risk factors are post-menopause and age > 65 years. Patients are asymptomatic unless there is a fracture; the commonest sites are hip, thoracolumbar spine and wrist. Spinal fractures can be asymptomatic.
Management
• General measures
 hour before breakfast, as food decreases absorption. Pamidronate has an analgesic effect and is useful for acute fracture pain.
hour before breakfast, as food decreases absorption. Pamidronate has an analgesic effect and is useful for acute fracture pain.Osteomalacia
Management
Paget’s disease
Management
• Drug therapy
Little MA, Raza K. Autoimmune rheumatic disorders. Medicine. 2010;38(2):67-124.
Mathews CJ, Weston VC, Jones A, et al. Bacterial septic arthritis in adults. Lancet. 2010;375:846-855.
Rosen CJ. Vitamin D insufficiency. N Engl J Med. 2011;364:248-254.
Scott DL, Wolfe F, Huizinga TWJ. Rheumatoid arthritis. Lancet. 2010;376:1094-1108.