31 Rheumatoid Arthritis of the Cervical Spine
KEY POINTS
Introduction
Rheumatoid arthritis (RA) is a chronic inflammatory disease that commonly presents with polyarthropathy, systemic symptoms, and cervical spine involvement. Some reports state that RA was first described by A.J. Landre-Beauvais, whereas others credit Robert Adams. Robert Adams described it as a separate entity from gout in the nineteenth century in Dublin. The term rheumatoid arthritis was coined by A.B. Garrod, and its predilection for the cervical spine was first highlighted by his son, A.E. Garrod.1
Epidemiology and Natural History
The prevalence of RA is up to 1% to 3% of the United States population. It is commonly seen in those 40 to 70 years of age, and the male to female ratio is approximately 1:3. Symptomatic cervical spine disease is present in 40% to 80% of patients with RA. Up to 86% of patients have radiographic evidence of cervical spine involvement. In a study that evaluated patients with RA undergoing hip and knee arthroplasty, over 60% had cervical spine involvement.2
Pathophysiology
Rheumatoid arthritis is a chronic immune-mediated response. Unknown antigens, perhaps viral, trigger a cell-mediated response resulting in the release of various inflammatory mediators. The inflammatory response is put into motion by the CD4+ lymphocytes, which activate the B lymphocytes to produce immunoglobulins that are found in the rheumatoid synovium. The rheumatoid synovium contains two distinct cell types: type A cells are morphologically similar to macrophages and type B cells are similar to fibroblasts. Type A cells are mainly for phagocytosis, whereas type B cells are highly metabolic and are equipped with organelles for protein synthesis. These cells produce multiple inflammatory mediators, such as TNF-α, metalloproteinases, collagenases, progelatinases, and IL-1.3 These mediators are targets for DMARDs.
Atlantoaxial instability is the most commonly seen (40% to 70%) affliction in the rheumatoid spine. The formation of periodontoid pannus leads to erosion of the transverse, alar, and apical ligaments. The weight of the head combined with flexion and extension at this level leads to stretching and eventual rupture of these ligaments. The odontoid itself and the lateral atlantoaxial articulations are commonly eroded as well, leading to further instability. Depending on the pattern and location of bony and ligamentous erosion, the subluxation may present as anterior, posterior, lateral, or rotational. Anterior is the most common (70%). Anterior subluxation of 0 to 3 mm is normal in adults, 3 to 6 mm is suggestive of instability and rupture of the transverse ligaments, and greater than 9 mm suggests gross instability and incompetence of all periodontoid stabilizing structures. Posterior subluxation is rare and may be associated with a defect in the anterior C1 arch or fracture or erosion of the odontoid. Lateral subluxation is defined as 2 mm of lateral displacement at the atlantoaxial articulation.
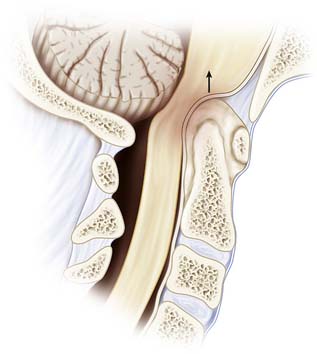
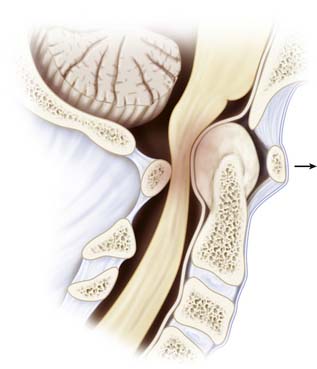
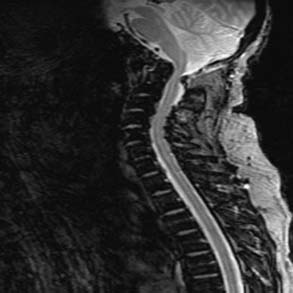
Cranial settling, or basilar invagination, is a late finding that is due not only to ligamentous and capsular erosion, but mainly to bone and cartilage destruction of the atlantoaxial and atlantooccipital articulations (Figure 31-1). Cranial settling carries an ominous prognosis. Anterior compression of the medulla oblongata can lead to injury to cranial nerve nuclei, syringomyelia, or obstructive hydrocephalus. Sudden death may also occur due to brainstem compression or vertebrobasilar dysfunction.
Clinical Presentation
Careful examination is necessary, as neurological deficit can be masked by weakness from peripheral joint involvement. Myelopathy is progressive and often goes unnoticed because of peripheral involvement. Fine motor skill deterioration may be mistaken for hand involvement, or decreasing ambulatory status may be mistaken for large joint involvement. As patients become more myelopathic, prognosis worsens. The Ranawat grading system for neural assessment may be used to appropriately classify the severity of myelopathy and can be used as a prognostic tool (Table 31-1).
| Grade | Severity |
|---|---|
| I | Normal |
| II | Weakness, hyperreflexia, altered sensation |
| IIIA | Paresis and long-tract signs, ambulatory |
| IIIB | Quadriparesis, nonambulatory |
Radiographic Analysis
Plain Radiographs
Radiographic criteria for RA, as defined by Bland, include atlantoaxial subluxation of 2.5 mm or more, multiple subaxial subluxations, disc space narrowing without osteophytes, vertebral erosions, eroded (pointed) odontoid, basilar impression, apophyseal joint and facet erosions, osteopenia, and secondary osteosclerosis from occiput to C2, which may indicate degenerative change.
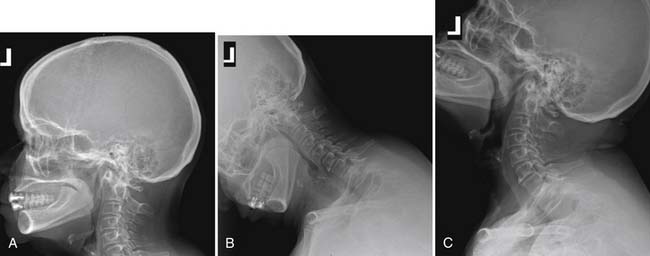
The lateral neutral, flexion, and extension films are an effective screening tool for detecting cervical involvement in RA. They allow for identification of static and dynamic instability in the upper and lower cervical spine. Anterior atlantodental interval (AADI) and posterior atlantodental interval (PADI) can be determined from these views. These two values are used to determine atlantoaxial instability. The AADI is measured from the posterior aspect of the anterior arch of the atlas to the anterior surface of the dens. Anatomically, the transverse ligament holds the odontoid process against the anterior arch of the atlas and acts as the primary stabilizer of the atlantoaxial articulation. As the transverse ligament attenuates, there is more motion between the odontoid and atlas, which manifests on flexion/extension films as dynamic instability. An AADI greater than 6 mm has been used as a sign of instability, whereas an AADI greater than 9 mm has been considered an indication for surgery. However, the use of the AADI in management has been questioned, as erosive changes and anatomic abnormalities may be present. Boden et al 4 showed that the PADI may be more reliable and a better predictor of neurological recovery after surgical stabilization. Patients with a PADI greater than 14 mm experienced a higher rate of neurological recovery, while those with a PADI less than 10 mm had no recovery (Figure 31-2). Posterior subluxation may also be seen on lateral radiographs and should raise the suspicion of an absent or fractured odontoid. The open-mouth view is useful to identify lateral subluxation, which is defined as greater than 2 mm of lateral displacement at the C1-2 lateral articulation.
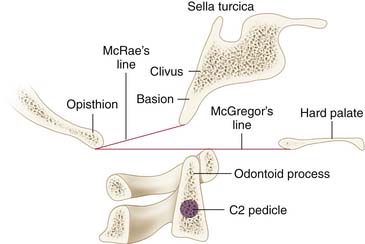
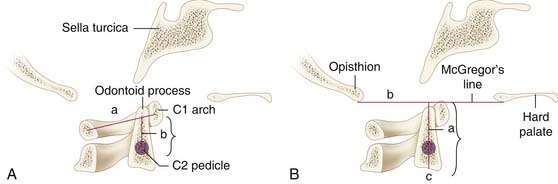
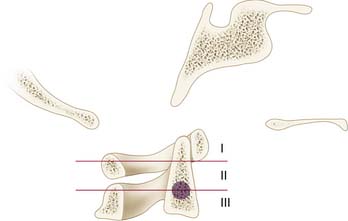
Several radiographic measures have been described to define cranial settling or basilar invagination5 (Figure 31-3). McRae’s line is defined on the lateral radiograph as a line that connects the margins of the foramen magnum. If the odontoid tip migrates above this line, it is considered cranial settling. Chamberlain’s line runs from the hard palate to the posterior edge of the foramen magnum. If the odontoid tip migrates 6 mm above this line, it is considered cranial settling. McGregor’s line runs from the hard palate to the opisthion or posterior base of the occiput. Cranial settling is defined as odontoid tip migration greater than 4.5 mm above this line. Erosive changes in the odontoid have made these relationships difficult to reliably measure. Therefore, the Ranawat method was designed to assess the extent of collapse at the atlantoaxial articulation. In this technique, the distance along the odontoid was measured from the C2 pedicle to the transverse axis of the ring of C1. A distance of less than 15 mm in males and 13 mm in females is considered to be cranial setting. Redlund-Johnell also described a technique that measured the vertical line from the midpoint of the caudad margin of C2 to McGregor’s line; cranial settling is diagnosed when the distance is less than 34 mm in males and 29 mm in females (Figure 31-4). Clark et al defined the “station of the atlas,” which describes the relationship of the anterior ring of C1 to the body of the odontoid, which is divided into thirds. The atlas usually lies at station I which corresponds to the proximal third (Figure 31-5). Riew et al stated that no single measurement alone was reliable; however, the combination of the Ranawat, Clark, and Redlund-Johnell methods yielded sensitivity and negative predictive value of 94% and 91%, respectively.
Computed Tomography
Computed tomography may also be used, especially in patients in whom MRI is contraindicated. CT adds valuable information about bony anatomy and osseous erosions. The use of contrast media helps provide information about inflammatory soft tissue changes and helps differentiate between effusions and hypervascular pannus.
Management
Nonoperative Management
The treatment of RA has been revolutionized by the introduction of newer pharmacological therapies that target the inflammatory mediators responsible for disease. The treatment of RA previously consisted of patient education, physical therapy, NSAIDs, remittive agents (gold, penicillamine, hydroxychloroquine, etc.), corticosteroids, and immunosuppressive agents (i.e., methotrexate).The newer drugs that are used in conjunction with the aforementioned regimen include antagonists to tumor necrosis factor-alpha (TNF-α) and interleukin-1 (IL-1).6
Surgical Indications
Goals of surgical treatment are to relieve pain, and to achieve spinal stability through a solid fusion, and to decompress the involved neural structures. Surgery should be considered in any of the previously mentioned instability patterns (atlantoaxial instability, subaxial subluxation, and cranial settling) with or without pain, myelopathy, or neurological deficits.7 Indications include progressive neurological deficit, mechanical neck pain in the setting of instability, radiographic risk factors of impending neurological injury (PADI less than 14 mm in the setting of atlantoaxial instability), cranial settling (as demonstrated by the combination of Clark station, Redlund-Johnell and Ranawat criteria), and a cervicomedullary angle less than 135 degrees.
Shen et al 8 described an algorithm for the patient who is neurologically normal. In these patients, observation is acceptable if the plain radiograph lateral view shows a PADI of greater than 14 mm and there is minimal evidence of cranial settling. For patients with a PADI less than 14 mm, an MRI should be obtained to look for the true SAC (scrutinizing odontoid erosion and periodontoid pannus). If the SAC is less than 13 mm or the cervicomedullary angle is less than 135 degrees, prophylactic arthrodesis should be considered. In patients with atlantoaxial instability and associated cranial settling, they recommend a more aggressive approach because of a higher morbidity and mortality associated with this subgroup of patients. In the subaxial spine, a posterior canal diameter greater than 14 mm in the neurologically normal patient can be observed, whereas those with a posterior canal diameter less than 14 mm on x-ray should obtain an MRI. If the SAC is less than 13 mm or there is significant subluxation, stabilization should be considered.
Operative Management
Atlantoaxial Subluxation
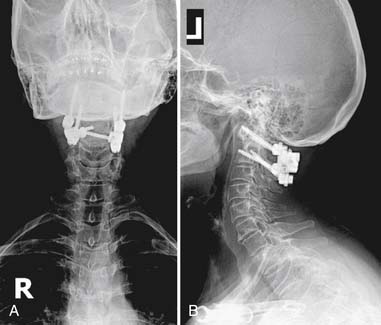
Several methods have been described for atlantoaxial stabilization. The Gallie wiring technique was first described in 1939 for fracture fixation. Various approaches have been taken to instrument the upper cervical spine. The Gallie technique consists of passing sublaminar wires rostrally beneath the lamina of C1 or atlas and then around the spinous process of C2, with the addition of a clothespin-shaped bone graft. The Brooks-Jenkins modification of the Gallie technique consists of sublaminar wires beneath the lamina of atlas and axis, with two cortical bone graft struts as opposed to one. The atlas can be instrumented using hooks and claws as well. Harms described a rigid posterior construct for stabilization of the upper cervical spine.9 This construct consists of C1 lateral mass screws and C2 pars interarticularis screws or C2 pedicle screws. Recently, pedicle screw fixation of C2 has become more common. The pedicle lies posterior and medial to the transverse foramen. The pedicle projection lies 5 mm caudal to the superior laminar edge of the axis and 7 mm lateral to the lateral border of the spinal canal. The pedicle axis is directed 30 degrees medial to the sagittal plane and 20 degrees rostral to the axial plane. The inferior pedicle width is approximately 3 mm less than the width of the superior pedicle. Therefore, to avoid vertebral artery injury and to maintain adequate purchase in the C2 pedicle, the screw should be directed to the superior medial portion of the pedicle.
The lateral C1-C2 articulation can also be fixed via the transarticular screw technique of Magerl. The transarticular screw traverses the isthmus of the axis and enters the posterior aspect of the atlantoaxial joint on its way to the lateral mass of the atlas (Figure 31-6). There are various contraindications to the transarticular screws, mostly focusing on the cord of the vertebral artery. When the transverse foramina are high-riding, this prevents placement of transarticular screws. The vertebral artery passes in a groove through the axis before entering the transverse foramina of the atlas. If the depth of the groove exceeds 5 mm, the remaining height of the lateral mass and pedicle width of C2 are both less than 2 mm. This would make it impossible to safely pass a 3.5 mm screw. Also, if the isthmus of the axis is less than 5 mm in height or width, the chance of penetration into the vertebral artery by a 3.5 millimeter transarticular screw increases. To be aware of these anatomical variations, it is necessary that preoperative CT scans (and CT angiograms) with 3D reconstructions be done prior to transarticular screw placement. An additional complication of transarticular screws is hypoglossal nerve injury. The twelfth cranial nerve courses anterior to the lateral tip of the C1 lateral mass. If the screws are too long or the lateral mass is overdrilled, injury to this nerve may occur, resulting in motor paresis of the tongue.10
Subaxial Subluxation
Lateral mass screw techniques as described by Roy-Camille, Magerl, Anderson, and Ahn have been used and result in adequate fixation, either unicortical or bicortical. The distance from the posterior midpoint of the lateral mass to the transverse foramen ranges from 9 to 12 mm. The lateral border of the artery lies 6 degrees lateral to the posterior midpoint of the lateral mass. Therefore, lateral mass screws are started at the posterior midpoint of the lateral mass and directed at least 10 degrees lateral to the sagittal plane. Trajectory parallels the facet joint, aiming toward the anterosuperior lateral corner of the lateral mass. Practically, this can be accomplished by laying the drill bit against the adjacent caudal spinous process. This will help ensure the required lateral angulation and anterosuperior trajectory. This will carry the tip of this screw superior to the exiting nerve root and lateral to the vertebral artery.
Conclusion
Management for rheumatoid arthritis of the cervical spine has improved. This is mainly due to earlier diagnosis and screening, early surgical referral, and aggressive medical management. Surgical outcomes have improved, primarily due to newer techniques, improved preoperative and postoperative management, appropriate patient selection, and improved surgical timing. Most authors recommend surgery in patients with neurological deficits. Those without neurological compromise should be investigated and followed carefully. Once a patient becomes myelopathic, the long-term mortality increases and the potential for neurological recovery decreases. Cervical spine involvement is common in patients with rheumatoid arthritis. Management is complicated and a multidisciplinary approach must be used.
1. Chin K. Surgical management of rheumatoid arthritis. In: Herkowitz, Garfin, Eismont, Bell, Balderston. The spine. Philadelphia: Elsevier, 2006.
2. Borenstein D. Arthritic disorders. In: Herkowitz, Garfin, Eismont, Bell, Balderston. The spine. Philadelphia: Elsevier, 2006.
3. Casey A.T., Crockard H.A., Pringle J., O’Brien M.F., Stevens J.M. Rheumatoid arthritis of the cervical spine: current techniques for management. Orthop. Clin. North Am.. 2002;33(2):291-309.
4. Boden S.D., Dodge L.D., Bohlman H.H., Rechtine G.R. Rheumatoid arthritis of the cervical spine: a long-term analysis with predictors of paralysis and recovery. J. Bone Joint Surg. Am. 1993;75(9):1282-1297.
5. Nguyen H.V., Ludwig S.C., Silber J., Gelb D.E., Anderson P.A., Frank L., Vaccaro A.R. Rheumatoid arthritis of the cervical spine. Spine J.. 2004;4(3):329-334.
6. Doan T., Massarotti E. Rheumatoid arthritis: an overview of new and emerging therapies. J. Clin. Pharmacol.. 2005;45(7):751-762.
7. Kim D.H., Hilibrand A.S. Rheumatoid arthritis in the cervical spine. J. Am. Acad. Orthop. Surg.. 2005;13(7):463-474.
8. Shen F.H., Samartzis D., Jenis L.G., An H.S. Rheumatoid arthritis: evaluation and surgical management of the cervical spine. Spine J.. 2004;4(6):689-700.
9. Harms J., Melcher R.P. Posterior C1-C2 fusion with polyaxial screw and rod fixation. Spine. 2001;26(22):2467-2471.
10. Puschak T.J., et al. Relevant surgical anatomy of the cervical, thoracic, and lumbar spine. In: Vaccaro, Betz, Zeidman. Principles and practice of spine surgery. Philadelphia: Mosby, 2003.