24
Rheumatic Disorders
1. Identify causes of arthritis.
2. Discuss different types of arthritis.
3. Discuss similarities and differences for osteoarthritis and rheumatoid arthritis.
4. Discuss the effects and benefits of exercise with arthritis.
5. Discuss common methods of management and rehabilitation of arthritic conditions.
6. Discuss principles of joint protection.
7. Discuss general pharmacologic interventions for arthritic conditions.
8. Discuss the different surgical options for arthritic conditions.
9. Discuss pathophysiology and management of rheumatic disorders.
Arthritis affects the lives of 37 million Americans, and it is the leading cause of disability in American adults. The Centers for Disease Control and Prevention (CDC) estimate that by the year 2020 nearly 60 million people will be affected by rheumatic disease, a blanket term covering the more than 100 different conditions that may cause pain, stiffness, and sometimes swelling in or around joints.2,15 Individuals affected with arthritis can suffer from pain, joint stiffness, swelling, and overall decrease in functional ability.23 The causes of arthritis are not fully understood, but there are certain characteristics that can predispose an individual to developing arthritis, include obesity, inactivity, age, and gender.15,23 Though the prevalence of arthritis increases with age, it is more commonly found in women than in men.15,23
ARTHRITIS
Osteoarthritis
Osteoarthritis (OA) is the most common form of arthritis and generally the most painful and disabling joint disorder.2,15,19,26 There is no single cause of osteoarthritis; however, it may be a combination of biomechanical, metabolic, and genetic factors.24,26 Prevalence of OA has been shown to increase with age and is more common in women older than 45 years of age. Risk factors associated with OA include obesity, trauma, infection, and repeated joint overuse.2,15,19,26
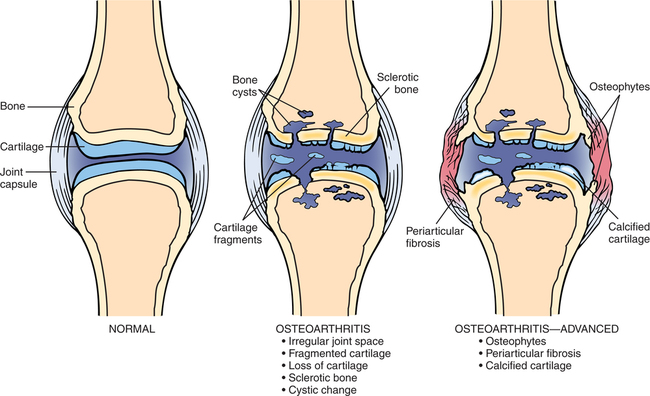
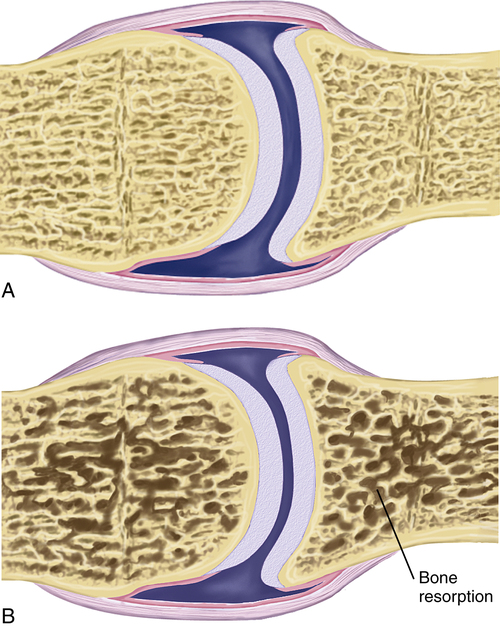
OA primarily affects the articular cartilage (which is composed of type II collagen, chondrocytes, and proteoglycans) that surrounds the subchondral bone (Fig. 24-1).2,24 Patients with OA have decreased synthesis and increased catabolism of the cartilage matrix. OA initially damages the cartilage, causing it to become thinner and thereby decreasing proteoglycan synthesis. Initially chondrocytes can maintain the cartilaginous matrix (which consists of proteoglycans and collagen), but after time focal synovial membrane inflammation develops, releasing cytokines, which increase the release of metalloproteinases.2 Metalloproteinase further breaks down cartilage collagen and proteoglycans.2,15 Generally OA is not considered to have any inflammatory response, but new research shows signs of inflammation can exist.2,15
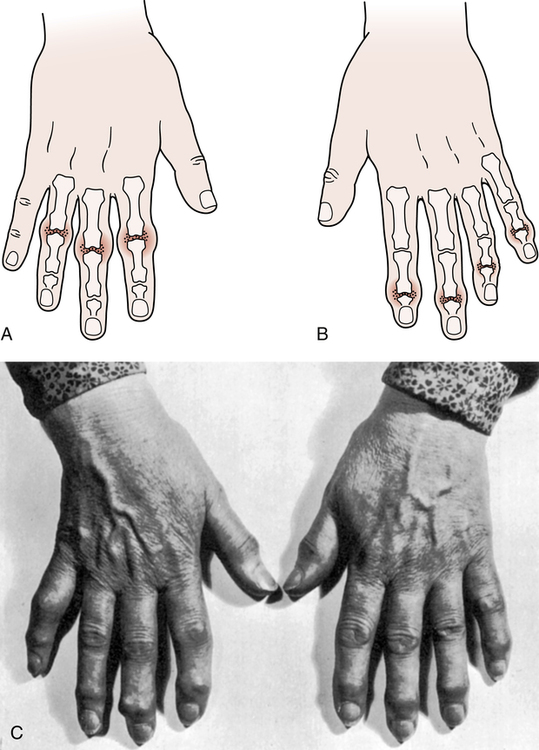
Osteoarthritis most commonly effects weight-bearing joints, such as the knee, hip, or spine.2,15,23,24 Joints in the hands can also be affected: the first carpometacarpal joint, distal and proximal interphalangeal joints (DIP and PIP joints, respectively), and the first metatarsophalangeal joint are other common sites for OA.24 In patients with OA of the hands, Bouchard and Heberden nodes, bony overgrowths at the PIP joints and the DIP joints, are often present (Fig. 24-2).19,24,27 Pain associated with OA usually occurs with activity and is relieved with rest.19,24 Other signs of OA include morning stiffness lasting 20 to 30 minutes, joint locking, a gel sensation in the joint, a bony appearance of the joint, crepitus, and effusion.19,24 Radiographic imaging can show a progression of subchondral bone sclerosis and cysts, osteophytes, and joint space narrowing.13,24 Carpal tunnel syndrome can even be caused by both osteoarthritis and rheumatoid arthritis (RA).27
Management of Osteoarthritis
Although there is no cure for OA, preventive measures can be taken to slow down the progression of the disease or better manage the symptoms. Obesity places extra stress on joints and is a key risk factor that can be prevented or remedied with proper diet and exercise.19,24 The addition of vitamin D and calcium to a patient’s diet can also reduce the occurrence and progression of OA.19 Muscle weakness and repetitive motions or trauma contribute to the onset of OA.24 Studies also have shown that immobilizing the joint for longer than 30 days can increase the risk of cartilage damage.4 Given the positive and negative effects of changes in behavior it is imperative to educate the patient on joint protection, health behavior changes, and the importance of exercise to the management of arthritis.
Education is the most important component to the management of OA. Patients must be educated on the progression of the disease and management of pain with supportive devices, alteration in activities of daily living (ADLs), or thermal modalities. Exercise and weight control are key components to a patient’s success with OA.2,24
Research has shown that every pound of body weight increases the forces in the knee by 2 to 3 pounds during single leg stance.38 Exercise, specifically flexibility, and strength training, has been shown to decrease pain and improve function in individuals with OA.24 Maintaining flexibility is an important first step because it helps decrease stiffness and allows for more comfortable movement.2 Slow progression of the exercise program is important so as to not exacerbate symptoms. Patients should be progressed to 15 minutes of stretching without an increase in symptoms before initiating strength training.2,24 Strength training improves the ability to absorb shock, support joints, and protect from injury.2,26 When choosing an appropriate exercise it is important to keep in mind how much stress in being placed on the joint. Closed-chain weight-bearing exercises can create shear and compressive forces across the lower extremity joints and may be a contraindication pending severity of OA. Open-chain exercises, therefore, are encouraged in patients with OA.
Rheumatoid Arthritis
Rheumatoid arthritis is the second most common form of arthritis, and while it can be equally disabling as OA, it can also lead to increased mortality. This increased mortality has been shown in some research to have systemic causes.12 The progression of RA also leads to difficulty with ADLs and disability. Along with most arthritic conditions, RA affects women more commonly than men and occurs at 20 to 40 years of age.2,14,19 Both genetic and environmental factors have been linked as causes of RA.14,19
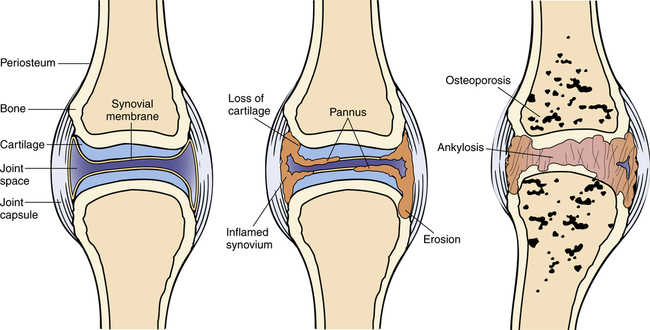
Although the exact etiology of RA is unknown, it is believed to start with a viral or bacterial infection that triggers an autoimmune response.2,14 The immune response causes the body to attack its own tissue, leading to breakdown of joints.2,14 RA affects the synovium lining, which then expands, damaging the extracellular matrix, cartilage, and bone.2,14,26 This autoimmune response also activates T cells, which secrete cytokines, causing expansion of the synovial layer. Cytokines increase activation of fibroblast-like cells and macrophages leading to breakdown of cartilage and bone (Fig. 24-3).2,14
Early signs and symptoms associated with RA include fatigue, weight loss, fever, and musculoskeletal pain. Later signs or symptoms include pain, tenderness, swelling, redness, and stiffness in specific joints.2,7,14,19 Unlike OA, RA morning stiffness can last hours and even all day. Fatigue in patients with RA may cause the patient to need to rest through the day.2 Extraarticular manifestations can affect the lungs, heart, blood vessels, eyes, skin, and other organs.2,7,19 It is important for the physical therapist assistant (PTA) to be able to distinguish the main differences between OA and RA (Table 24-1).
Table 24-1
Differential Diagnosis between Rheumatoid Arthritis and Osteoarthritis
| Differential | Rheumatoid Arthritis | Osteoarthritis |
| Joints affected | Any joint | DIP > PIP Spine Hip Knee |
| Age | Any age Most common ages 20-60 years |
More common >40 years |
| Gender | More common in women | More common in men <45 years and women >45 years |
| Relative severity | More than OA | Less than RA |
| Disease pathogenesis | Autoimmune: Immune system attacks body | Condition of wear and tear with aging or injury |
| Joint involvement | Symmetric | Asymmetric |
| Joint destruction | Due to inflammation | Due to biomechanical stress |
| Deformities | Swan neck Ulnar deviation Wrist subluxation Boutonniere deformity |
Heberden nodes Bouchard nodes |
| Erythrocyte sedimentation rate | Markedly increased | Mild increase |
| Connective tissue flexibility | Increased | Decreased |
| Morning stiffness | >1 hour | <30 minutes |
| Rheumatoid factor | Positive in 70% | Negative |
| Imaging | Juxtaarticular osteoporosis, erosions | Osteophytes Eburnation Reduced joint space |
| Management | Physical therapy/occupational therapy NSAIDs Gold Penicillamine |
Paracetamol Weight loss Joint replacement Exercise |
| NSAID response | Usually some relief | Variable relief |
A unique feature of RA is the rheumatoid nodules, which occur on bony prominences, extensor surfaces, or pressure points.2,19 There are several common physical changes that occur36:
Management of Rheumatoid Arthritis
When treating a patient with RA, education and prevention are vital. Some important objectives of physical therapy all have a common theme of prevention: prevent pain, deformities, loss of normal function, and loss of normal social, physical, and work capabilities. An exercise routine should start with stretching and range of motion (ROM) exercises in pain-free ranges,2,14 and patients with RA should be informed not to overstretch an inflamed tissue to avoid any tears. To prevent contractures and muscular atrophy it is crucial to maintain full ROM of joints through a graded exercise routine.14 Muscle conditioning is also a key component of management, and strength can be increased through isometric and dynamic exercise. Application of heat before exercise can result in better performance.19 Generally during an acute exacerbation, isometric exercises are recommended. During subacute and chronic phases patients can implement dynamic exercise. Do note that vigorous activity should be avoided during an exacerbation of symptoms. Any exercise that causes pain longer than 1 hour after exercise should be eliminated.19
The current management approach with medication is to start early with disease-modifying antirheumatic drugs (DMARDs) because they have been shown to slow RA progression. Nonsteroidal antiinflammatory drugs (NSAIDs) are the most commonly used drugs to decrease pain and swelling and increase ROM. Corticosteroids are also used for swelling, pain, and fatigue and tend to decrease symptoms faster. Biological response modifiers block cytokines, therefore decreasing the breakdown of cartilage and bone.14 More in-depth explanation of the pathophysiology of these drugs will be explained later.
Reactive Arthritis
Reactive arthritis, or Reiter syndrome, is most commonly an abrupt onset of arthritis in young men presenting with the triad, conjunctivitis, urethritis, and oligoarticular arthritis.7,18,19 Conjunctivitis is also known as pinkeye, which is inflammation of the conjunctiva (outermost layer of eye and inner surface of eyelid). Urethritis is inflammation of the urethra and presents as painful urination. Oligoarthritis is a form of arthritis with inflammation in two to four joints. Reiter syndrome usually presents within days or weeks of a dysenteric or sexually transmitted infection.18,19 The arthritis is usually asymmetrical and involves the weight-bearing joints, such as the toes, ankles, and knees, then ascends to the axial skeleton and upper extremities.7,18,19 Other symptoms present with Reiter syndrome are oral ulcers, penile lesions, keratoderma blennorrhagicum, and plantar heel pain.7,19 Approximately 80% of individuals with Reiter syndrome are positive for human leukocyte antigen B27 (HLA-B27).7,19 The human leukocyte antigen system is the name of the major histocompatibility complex in humans. The major HLA antigens are essential elements in immune function. Sacroiliitis is observed in about 60% of patients with chronic Reiter syndrome. Management of Reiter syndrome includes NSAIDs and physical therapy similar to that used to treat ankylosing spondylitis.
Psoriatic Arthritis
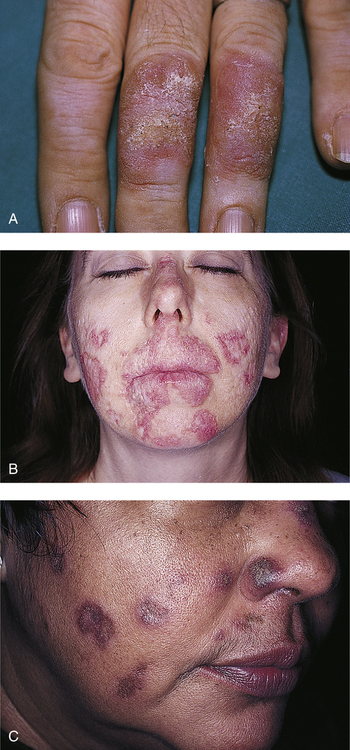
Psoriatic arthritis is a seronegative inflammatory joint disease affecting a small percentage of people with psoriasis.13,19 Psoriasis is an inherited chronic inflammatory skin disease that is characterized by silvery scales on a bright red plaque (Fig. 24-4).5,13 In most cases the skin disease precedes the arthritis symptoms by several months to years.9 Psoriatic arthritis closely resembles rheumatoid arthritis, but has differences such as DIP involvement, psoriasis or family history, nail pitting, and “sausage” appearance of digits.7,14,19 Gender does not appear to predispose one to psoriatic arthritis, but it generally begins at ages 30 to 50 years.9,13,18 Psoriatic arthritis is usually asymmetric and involves the small joints of hands and feet.7,13,32 However, larger axial joints such as the sacroiliac joint can be affected in later phases of disease. Sacroiliitis usually occurs unilaterally, whereas ankylosing spondylitis is bilateral.13,18 Imaging reveals a “pencil-in-cup” deformity caused by erosion and destruction of the phalanx bones that makes them look like a sharpened pencil at the end of the bone (Fig. 24-5).5,7,32 Furthermore, psoriatic arthritis can cause fingernail thickening, pitting, and separation from the nail bed.9 Finally, periosteal reactions (formation of new bone) can be seen on x-rays.
Management for psoriatic arthritis is similar to that of rheumatoid arthritis.7,18,32 Although there is no cure for psoriatic arthritis, NSAIDs can be used to treat inflammatory symptoms.5,13 Most of the time the disease is mild and not destructive; therefore treatment consists of symptom management.5,13
Juvenile Rheumatoid Arthritis
Many rheumatic diseases in children exist, consisting of both acute and chronic conditions, with juvenile rheumatoid arthritis (JRA) being one of the most common.44 JRA, a chronic inflammatory disease, actually covers three types of childhood arthritis: pauciarticular, polyarticular, and systemic.7,13,32,44 The etiology of JRA is unknown, but is thought to be triggered by environmental factors or infection in children with genetic predisposition.13,44 “JRA is similar to adult RA in the fact that the immune system mistakenly attacks the joints and organs, causing inflammation, destruction, fatigue, and other local and systemic effects.”13 JRA occurs before the age of 16 years and affects girls more commonly.7,13,44 To confirm diagnosis the child must have the arthritis for at least 6 consecutive weeks.44 Other symptoms of JRA are fever, rash, fatigue, anemia, loss of appetite, stiffness, irritability, altered mobility, and change in ADLs.44
Pauciarticular JRA is characterized by asymmetric synovitis of four or less joints.7,13,44 There are usually no systemic features and it most commonly affects the knee, elbow, and ankle (Fig. 24-6).13,44 Two subtypes of pauciarticular JRA exist: early onset and late onset.7,13,44 Early onset pauciarticular JRA occurs before the age of 5 years and usually affects girls. Early onset pauciarticular JRA left untreated can result in iridocyclitis that can lead to visual impairments.7,13,44 The second subtype, late onset pauciarticular JRA, occurs between the ages of 10 and 12 years and is more common in boys. This subtype affects large weight-bearing joints and entheses (insertion point of tendon into bone).44 These children often have spinal involvement that may develop into a spondyloarthropathy.13,44
Polyarticular JRA is synovitis in more than four joints and is more common in girls.7,13,44 It usually manifests with symmetrical involvement of the small joints of the hands or feet, wrists, elbows, shoulders, knees, hips, ankles, cervical spine, and temporomandibular joints.13,44 Bursitis and tendinitis can occur because they too are lined with synovial tissue. Unlike pauciarticular JRA, polyarticular JRA can have systemic features, including low grade fever, anemia, leukocytosis, mild hepatosplenomegaly, and lymphadenopathy.44
The last type of JRA is systemic JRA (Still disease) which can occur at any age and does not favor girls or boys.13,44 Systemic JRA is characterized by a rash, synovitis in one or more joints, and an intermittent high grade fever.7,13,44 The fever usually occurs in the afternoon and evenings and will return to normal with the child feeling better.13,44 Because the fever can precede all other symptoms these children are often initially evaluated for fever of unknown origin.44 The rash usually appears with the fever and is salmon pink, 2 to 5 mm in diameter, and has an erythematous perimeter.44 Other signs and symptoms of systemic JRA include malaise, irritability, anemia, hepatitis, peptic ulcer disease, leukocytosis, thrombocytosis, lymphadenopathy, hepatomegaly, splenomegaly, pericarditis, and pleuritis.13,44
Management of Juvenile Rheumatoid Arthritis
Management for children with JRA is a combination of medication, physical therapy, and occupational therapy. Main objectives of therapy should be to control pain and inflammation, promote mobility, and improve function.13,44 Control of pain and inflammation is usually done with NSAIDs, which have been shown to decrease stiffness, pain, and swelling in children with JRA. Other medications used with JRA are corticosteroids, DMARDs, infliximab, and immunosuppressants.13,44 ROM is the strongest indicator of functional disability in children with systemic JRA.13 Therefore, all joints should be stretched through the full ROM twice a day to maintain good mobility. 44 Heat can be used before stretching to help warm the muscles and decrease pain before stretching. Splinting and serial casting can also be used to help maintain or gain ROM.44 Resistive exercise is also important and has been shown to change the immune response, with lower levels of cytokines and higher levels of antiinflammatory compounds.13 Aquatic therapy is an appropriate management for JRA because the heat can help relax the muscles and decrease pain.44 Even though the patient with JRA is only a child, education in joint protection and energy conservation is still important. Furthermore, always try to make the exercise program fun, interesting, and interactive to keep the child involved.44
Septic Arthritis
Septic arthritis is the invasion of a joint by an infectious agent causing arthritis. Septic arthritis usually occurs from a bacterial infection, but can be viral, mycobacterial, or fungal. Bacteria are introduced into the joint by the bloodstream from an infection elsewhere or from direct penetration after a wound, surgery, or local infection.42 Two common types of septic arthritis are gonococcal and nongonococcal.19,42
Gonococcal Arthritis
Gonococcal arthritis usually occurs in healthy individuals and is two to three times more common in females.19,42 Initially the patient will experience 1 to 4 days of noninflammatory joint pain in the wrist, ankle, knee, and elbow. Chronic arthritis or tendonitis are common symptoms preceding gonococcal arthritis.42 Patients tend to have a characteristic asymptomatic skin lesions with 2 to 10 small necrotic pustules over the extremities, especially the palms and soles.19
Nongonococcal Arthritis
Nongonococcal bacterial infections are primarily monoarticular and in large weight-bearing joints and wrists.19,42 Previous joint damage from a disease like RA or intravenous drug users have increased risk of infection.19,42 Staphylococcus aureus is the most common cause of nongonococcal septic arthritis.19,42 Nongonococcal septic arthritis is marked by a sudden onset of acute arthritis with pain, swelling, and heat in one joint.19 The hip, wrist, shoulder, and ankle can all be affected, but the knee is the most common. Chills and fever often accompany the symptoms of nongonococcal septic arthritis.19
Management of nongonococcal arthritis
Management should be initiated quickly with systemic antibiotics addressing the causative organism. If the specific organism cannot be determined then bacterial antibiotics are recommended.19 Aspiration of the affected joint will keep the joint free of destructive exudates.19,42 Early intervention is important because ankylosis and articular damage can occur if management is delayed. Immobilization and heat can help decrease the joint pain.19 Rest, elevation, and immobilization are used during the acute phase of the disease.
As stated before, early diagnosis and management are important because of the potential for harm if septic arthritis goes untreated.42 Risk factors to keep in mind are infection elsewhere in the body, very old or young age, presence of other systemic diseases, recent joint aspiration or surgery, prosthetic joints, immunosuppression, and intravenous drug abuse.13,42 An infected joint will be painful, tender, and have limited motion, but may not have redness, heat, and swelling, especially if treatment includes immunosuppressants.42 Finally, remember that prevention is always a key component of physical therapy, so passive and then active ROM should be started as soon as possible to prevent contractures and loss of strength.42
Arthritic Conditions of the Spine
 Onset is before the age of 40 years.
Onset is before the age of 40 years.
 Patients generally have inflammatory arthritis of the spine or the large peripheral joints.
Patients generally have inflammatory arthritis of the spine or the large peripheral joints.
Ankylosing Spondylitis
Ankylosing spondylitis is a type of inflammation that affects the synovium of the spinal arthrodial joints as well as all the joint ligaments of the spine at their insertion points into the bone (enthesitis). It begins in the sacroiliac joints in nearly all patients and spreads superiorly up the spine.18 As the disease progresses the spine becomes more rigid (ankylosed) and develops flexion deformities.18 The disease also leads to formation of bony bridges called syndesmophytes between the vertebra. Structurally the patients will lose the lumbar curve, have reduced chest expansion, and have an increase in thoracic kyphosis.18,22 Other changes noted in radiographic imaging are squaring of vertebrae and destruction of the sacroiliac joints32 (Fig. 24-7).
Ankylosing spondylitis has a greater incidence in men and the age of onset is usually in the late teens to early 20s.18 Hypomobility is likely to be seen in men between ages 40 and 50 years and in women older than 50 years.27 Patients with ankylosing spondylitis usually will complain of alternating buttock pain that radiates down the thigh and that increases with rest but decreases with activity, a hot bath, or a shower.18 Patients may show signs of peripheral arthritis such as swelling, redness, and tenderness. Constitutional symptoms include fever, fatigue, weight loss, and elevated erythrocyte sedimentation rate (ESR).18 Ankylosing spondylitis can often be confused with sacroiliac arthritis, however there are several differences between these two diseases (Table 24-2).
Table 24-2
Differential Diagnosis between Ankylosing Spondylitis and Sacroiliac Arthritis
| Differential | Ankylosing Spondylitis | Sacroiliac Arthritis |
| History | Bilateral sacroiliac pain that may refer to posterior thigh Morning stiffness Male predominance |
Bilateral sacroiliac pain referring to gluteal area (S1-S2 dermatomes) Morning stiffness (prolonged) Coughing painful |
| Observation | Stiff, controlled movement of pelvis | Controlled movement of pelvis |
| Active movement | Decreased | Side flexion and extension full Slight limitation of flexion |
| Passive movement | Decreased | Normal |
| Resisted isometric movement | Pain and weakness, especially if sacroiliac joints are stressed | Pain, especially if sacroiliac joints are stressed |
| Special tests | Sacral stress tests probably positive | Sacral stress tests probably positive |
| Sensation and reflexes | Normal | Normal |
| Palpation | Tender over sacroiliac joints | Tender over sacroiliac joints |
| Diagnostic Imaging | X-rays diagnostic | X-rays diagnostic |
| Lab tests | Erythrocyte sedimentation rate increased HLA-B27 human leukocyte antigen present in 80% |
Normal |
From Magee DJ: Orthopedic physical assessment, ed 5, St Louis, 2008, Saunders.
Management of ankylosing spondylitis
Management for ankylosing spondylitis includes both physical therapy and drug therapy. Early rehabilitation of ankylosing spondylitis is crucial because it has been shown to significantly reduce the impact of disability.18 Therapeutic exercise along with antiinflammatory drug therapy is important in managing ankylosing spondylitis. Benefits of exercise include improved mobility, posture, and function. Education is key to starting management of patients with ankylosing spondylitis. Patients should try to exercise when pain level is low and they are least tired. Starting an exercise session with heat application and light motion exercises can help loosen the joints and decrease pain for exercise.18 Before starting the patient on a strengthening regimen, the therapist should always try to improve mobility of the spine, which can reduce pain and stiffness in the patient.18 Physical therapy should focus on stretching the anterior flexor muscles and strengthening the extensors. Specifically, therapy should focus on strengthening the postural muscles, back and neck extensors, shoulder retractors, and hip extensors and abductors.18 A prone program is a good management option to stretch the anterior muscles.18 Postural exercises are also beneficial, including standing against a wall with heels, buttocks, and shoulders touching the wall. Also, patients should try to sleep with as much extension as tolerable and lay prone at least 15 minutes a day.18 Aquatic therapy is another management option that can help reduce discomfort and provide an avenue for relaxation, stretching, and strengthening.18 Finally, breathing exercises are important because of the decreased chest expansion that occurs with ankylosing spondylitis.
Pharmacologic intervention is usually NSAIDs to help decrease pain and stiffness, allowing for normal ADLs and exercise. Indomethacin is the most effective NSAID used with ankylosing spondylitis for decreasing night pain and morning stiffness.18,19 Sulfasalazine, which reduces the levels of acute phase reactants, may act as a “disease-modifying” agent. Sulfasalazine can decrease the peripheral symptoms associated with ankylosing spondylitis. Immunosuppressant drugs are reasonable for the severe cases when a patient cannot participate in physical therapy.18,19
NONARTHRITIC RHEUMATIC DISEASES
Gout
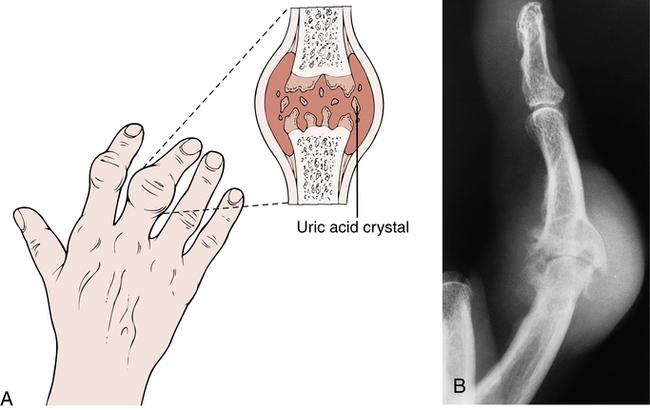
Gout is a metabolic disorder characterized by deposition of monosodium urate crystals in the joints, soft tissue, kidneys, and other connective tissue (Fig. 24-8).7,13,19,42 Once urate crystals are present they can cause acute or chronic inflammation by stimulating inflammatory mediators.7,13,19,32,42 The deposition of monosodium urate crystals is the outcome of hyperuricemia, which is the presence of high levels of uric acid in the blood. Hyperuricemia is due to the overproduction and/or underexcretion of uric acid.7,13,19,32,42 Overproduction of uric acid is more common in individuals with a history of lymphoma, leukemia, or psoriasis.13,19 Overproduction can also be due to enzyme abnormalities, hematologic malignancies, or other causes of rapid cell turnover.42 Underexcretion of uric acid is more common with obesity, fasting, medication (such as diuretics or cyclosporin), renal insufficiency, hypertension, hypothyroidism, hyperparathyroidism, and acidosis.13,19,42 Alcoholism increases risk of gout by both increasing production and decreasing the renal excretion of uric acid.13,19,42
Gout most commonly affects men older than the age of 30 years with occasional cases in postmenopausal women.7,13,19,42 Acute monoarticular onset of inflammatory arthritis that is worst at night characterizes gout. Although the metatarsophalangeal joint of the great toe is the most common site of pain, the ankle, knee, wrist, elbow, and fingers can all be affected.13,19,42 The involved joints usually become tender, swollen, warm, and red.13,19,42 A fever often occurs along with the joint complaints.13,19 The early initial episodes only last 3 to 10 days and then a patient can go months to years with no symptoms.13,19,42 Severe gouty attacks suddenly return with more frequency affecting more joints and lasting longer.13,19,42 The gout can become chronic with multiple joint damage leading to loss of function and disability.13,19 Tophi, visible deposits of crystallized monosodium urate, usually occur several years after the first episode of gout.
Management of Gout
Management of acute gout focuses on the arthritis and then addresses the hyperuricemia.13,19 NSAIDs are the most common management for acute gout decreasing both inflammation and pain.13,19,42 Corticosteroids are also used, but mainly when a patient has a contraindication for NSAIDs.19 Another management option is to use drugs to inhibit tubular reabsorption of uric acid to promote urinary excretion.39 Furthermore, rest, elevation, and joint protection are important during acute gout to further promote decreased inflammation.13,42 Between or after the acute attacks hyperuricemia is addressed to help prevent future episodes.13,19,42 Management when symptom free includes changes in diet, avoidance of hyperuricemic medications, colchicine, and reduction of serum uric acid. Dietary changes that can decrease the risk of gout are weight loss, moderation of alcohol, and avoidance of high purine foods.13,19 Controlling the hyperuricemia is important to prevent gout from becoming chronic.13
Fibromyalgia
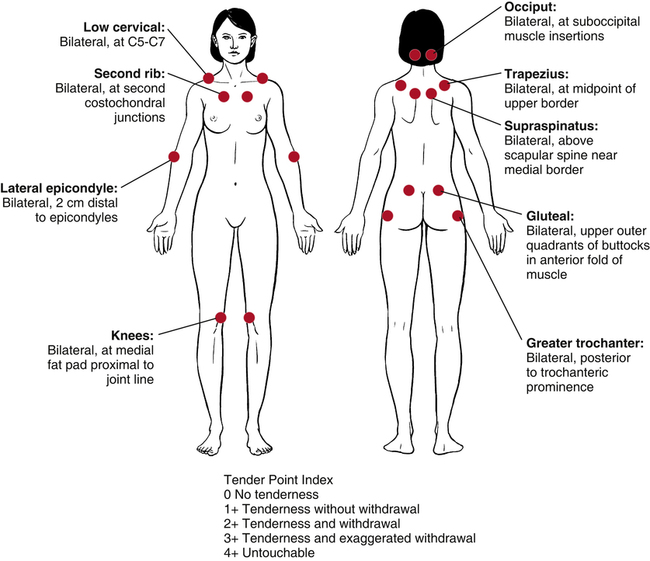
Fibromyalgia is a chronic widespread muscle pain syndrome.8,13,19,21 By definition fibromyalgia is widespread pain lasting at least 3 months with physical findings of 11 to 18 tender points (Fig. 24-9).8,13,21 Common characteristics of fibromyalgia are chronic widespread pain, aching, fatigue, and stiffness. Patients may also complain of headaches, sleep disorders, mood disorders, irritable bowel syndrome, and paresthesias.28 Fibromyalgia is most common in women aged 20 to 50 years.8,13,19 The exact etiology and pathogenesis of fibromyalgia is not fully understood, but is thought to be disturbances in different systems of the body. One common thought is that pain results from abnormalities of central sensory processing.8 New research characterizes fibromyalgia as a biological disorder associated with neurohormonal dysfunction of the autonomic nervous system (ANS) because of the objective biochemical, endocrine, and physiologic abnormalities.13 Furthermore, abnormalities in the hypothalamic–pituitary–adrenal axis, reproductive hormone axis, ANS, and immune system have been found in patients with fibromyalgia.13 The onset of fibromyalgia may be due to prolonged stress or anxiety, trauma, rapid steroid withdrawal, hypothyroidism, and viral and nonviral infections.8,13 Fibromyalgia may start as localized pain and after months or years become widespread.8 The pain associated with fibromyalgia is often described as burning or aching, and sometimes tender, stiff, throbbing, and sore.8,13 Even though fibromyalgia pain is widespread, patients will have one or two locations that are the worst, which are usually the neck, shoulders, and back.8,19,21 Sleep disturbance is one of the other more common symptoms in fibromyalgia.8,13,19 Patients will complain of exhaustion even after a night of sleep, which is because of the disordered non-rapid eye movement sleep.35 Also, patients with fibromyalgia have increased motor activity and restlessness during sleep, which accounts for increased fatigue.35 Other common symptoms are fatigue, subjective numbness, chronic headaches, dizziness, Raynaud phenomenon, and irritable bowel and bladder.8,13,19,21 Symptoms tend to be exacerbated with noise, stress, tiredness, weather changes, trauma, noxious smells, and too much or too little exercise.8,13,28
Management of Fibromyalgia
The first step in treating a patient with fibromyalgia is to make sure the patient understands they have a diagnosed syndrome that is a legitimate disorder with real symptoms and there is an effective management.8,19 The management for fibromyalgia needs to be multidisciplinary and address education, stress management, nutrition and lifestyle training, medication, muscle pain, and exercise.13 Pharmacologic management focuses on managing the pain and sleep disturbances.8 Antidepressants are commonly used with fibromyalgia because of their positive effects on pain, sleep, and fatigue.8,21 The antidepressants work well with some patients because the chemicals in the body that control pain and sleep also control mood.21 Other drugs used to treat fibromyalgia are muscle relaxants, antianxiety medications, and sleep aids.9
Exercise is an important aspect of fibromyalgia management and is shown to have numerous benefits.8,13,19,21 The exercise program should not be progressed too fast and it is suggested to have the patient to start below a level they believe they can accomplish.8 Modalities are useful in decreasing a patient’s acute pain, therefore allowing them to start an exercise program.13,21 Stretching can help improve flexibility and decrease pain. Stretching should be done in a pain-free range and can start with 10- to 15-second holds and then progress up to 1 minute. It is important to perform stretches at least once a day. Heat alone can help with muscle pain, but it is also beneficial to use heat before stretching.8,21 Aerobic exercise has been shown to decrease pain and improve function in patients with fibromyalgia.8,21 The exercise routine can be broken into several shorter bouts throughout the day or one longer 30-minute session. Depending on the patient’s fitness level, some may need to start with 5 minutes daily and work up to 30 minutes slowly. It is very important that the patient avoid overexertion because this can lead to increased symptoms.8 Strengthening can help reduce the risk of muscle damage, but the patient should attempt to reduce eccentric muscle work.8 Patients should pause for about 4 seconds between repetitions to allow for complete muscle relaxation. Lifting above the head and shoulders should be avoided to reduce risk of shoulder girdle injury or overuse. Furthermore water therapy or aerobics is a good alternative because the warmth and decreased pressures can lead to better relaxation.8
Systemic Lupus Erythematosus
Systemic lupus erythematosus (SLE) is a chronic inflammatory autoimmune disorder that may affect multiple organ systems.7,13,19,37 SLE is most common in women during their childbearing years and is rarely found in older individuals.7,13,19,37 In SLE the body produces antibodies against itself.13 The antigen–antibody complexes in tissues suppress the body’s immunity and damage tissues. The etiology of SLE is unknown, but environmental and genetic factors are believed to be the most related with evidence also supporting interrelated immunologic and hormonal factors.13 Many risk factors exist for SLE with hereditary factors at the forefront, along with physical and mental stress, streptococcal or viral infections, exposure to sunlight or ultraviolet light, and abnormal estrogen metabolism.13 Diagnosis for SLE is not difficult if the patient presents with common symptoms associated with SLE. The American Rheumatism Association has diagnosis criteria for SLE in which the patient needs to show 4 or more of the 11 symptoms. If the patient shows a few symptoms then diagnosis is made using clinical judgment along with supportive laboratory testing.19,37
The clinical symptoms of patients with SLE are variable and most will not present with exactly the same symptoms. The severity of SLE can vary drastically from a treatable rash or fatigue to a life-threatening illness.19,37 The skin, joints, lungs, kidneys, blood, and other organs and tissues can be affected.13,19,32,37 General signs of SLE include fever, fatigue, anorexia, weight loss, and myalgias.19,37 Joint involvement is one of the earlier symptoms and occurs in more than 90% of patients.19 Symmetrical polyarthritis is common in any joint, but is usually found in small joints of hands, wrists, and knees.13,37 SLE presents like RA, but is not usually destructive or deforming.13,19,32,37 When deformities are present, ulnar deviation, swan neck deformity, fixed subluxations of fingers, tenosynovitis, and tendon ruptures can occur.13,37 Recurrent inflammation of tendons and other supportive structures of the joints can lead to ulnar deviation of the second to fifth fingers and subluxation of the metacarpophalangeal joints, which is referred to as Jaccoud arthropathy.37,45 Jaccoud arthropathy is correctable with no radiographic signs of erosion.37 Also, observe patients for signs of osteonecrosis or septic arthritis, which will present as persistent monoarthritis primarily in the shoulders, hips, or knees.37
Another common symptom in SLE is skin rashes over areas exposed to sunlight. Butterfly rash is an acute inflammatory rash over the nose and checks.13,19,32,37 Discoid lupus is characterized by raised, red, scaly, and scarring rashes that can develop around the face, scalp, ears, and upper extremities (Fig. 24-10).13,19,37 Other cutaneous manifestations include alopecia, oral ulcers, fingertip lesions, periungual erythema, nail fold infarcts, splinter hemorrhages, livedo reticularis, urticaria, panniculitis, and Raynaud phenomenon.13,19,37 Other clinical findings in SLE are associated with the renal, hematologic, cardiopulmonary, immune, and central nervous systems.13,19,37
Management of Systemic Lupus Erythematosus
Systemic lupus erythematosus is marked by remissions and relapses and therefore management is focused on addressing symptoms quickly during an exacerbation.19,37 Patient education is important for successful management of SLE. Relapses are less likely if activities are controlled and sometimes limited.13 Also, after an exacerbation, return to activity should be slow and pain free.13 Joint pain is managed similar to RA, with NSAIDs as the primary medication for minor symptoms.19,37 Patients should be cautioned against prolonged sun exposure and should use sunscreen regularly. Topical corticosteroids are often used for rashes or skin lesions.19,37 Because of the use of corticosteroids, patients will have a higher risk of osteoporosis, so weight-bearing exercises should be incorporated into the management plan.
OSTEOPOROSIS
It is not uncommon for patients with arthritic conditions to concomitantly have osteoporosis, a disease characterized by low bone mass and microarchitectural deterioration of bone tissue, which leads to enhanced bone fragility and a consequent increase in fracture risk (Fig. 24-11).29 The decrease in bone mass is due to decreased osteoblast activity, which builds bone, and/or increased osteoclast activity, which reabsorbs bone.43 Remodeling of bone, which maintains bone mass, is performed by osteoblasts and osteoclasts and occurs about every 120 days. However, between the ages of 30 and 40 years, bone resorption starts to exceed bone formation and density decreases.25 The bone then becomes weaker because of the decreased quantity of bone, however, the quality of bone remaining has not been altered.7,32
There are many risk factors associated with osteoporosis, such as a sedentary lifestyle, white or Asian race, thin body frame, smoking, excessive alcohol intake, immobilization, early menopause, low calcium and vitamin D intake, and corticosteroid treatment.25,32 Osteoporosis prevalence is more common in women and is directly associated with age. Peak bone mass is usually reached by age 20 to 25 years and then slowly declines, especially after menopause. The peak bone mass is generally higher and the decline in bone mass is less rapid in men.29 For more on osteoporosis and bone healing.
The clinical features associated with osteoporosis are kyphosis, vertebral compression fractures, hip fracture, and distal radius fractures.29 However, a true diagnosis is made by measuring bone mineral density. The most popular method to measure bone mineral density is dual energy x-ray absorptiometry (DEXA).
Preventive measures for osteoporosis include a proper diet with adequate calcium and vitamin D, weight-bearing exercises, and an estrogen therapy evaluation at menopause.32 Prevention or management of osteoporosis needs to include weight-bearing activities and strength along with endurance exercise.39 Management for osteoporosis should include a combination of medication (bisphosphonates, teriparatide, strontium ranelate), nutrition (calcium and vitamin D), and exercise (aerobic, weight-bearing, and resistance exercise). Getting the correct amount of both vitamin D and calcium are important for healthy bones. Calcium alone will not lead to strong bones, because vitamin D is needed to transport the calcium into the bone.9 Strength training exercises are important for postmenopausal women with osteoporosis, because they can increase or stabilize bone density of the hip and spine while also improving muscle mass, strength, and balance.26 Furthermore, increasing the strength of the back extensors can help decrease symptoms of osteoporosis.26
TREATMENT IN RHEUMATIC DISEASE
 Decreasing biomechanical stress on joints
Decreasing biomechanical stress on joints
 Increasing cardiovascular tolerance to activity (especially in RA)
Increasing cardiovascular tolerance to activity (especially in RA)
 Improving efficiency and safety of gait
Improving efficiency and safety of gait
 Promoting independence with ADLs
Promoting independence with ADLs
 Educating about joint protection, energy conservation techniques, functional abilities, and limitations
Educating about joint protection, energy conservation techniques, functional abilities, and limitations
These goals can be achieved with an eclectic management program including modalities, stretching, strength and aerobic training, and education. Numerous studies have shown different modes of exercise to be beneficial in decreasing a patient’s signs and symptoms of arthritis, so it is important for the patient to have a balanced exercise routine.25
Rehabilitative Management of Rheumatic Disorders
Modalities
Cold
During an acute exacerbation of symptoms, patients should use cold to decrease inflammation, pain, and swelling.9,17 Cold has been shown to have beneficial effects on pain, function, and stiffness.17 Cold should be avoided in patients with inadequate thermoregulatory response.17 Cold decreases pain by slowing or blocking nerve conduction, decreasing activity of the muscle spindle, and releasing endorphins. Veins in the tissues contract because of the coldness and decrease blood flow and capillary pressure, therefore decreasing swelling.17 Histamine release is blocked by cold, which also decreases inflammation.
Heat
During subacute or chronic phases of rheumatic diseases, heat is more appropriate to decrease pain and increase ROM.17 Heat should be avoided during an acute phase of inflammatory arthritis and in people who have decreased thermoregulatory response. Other contraindications include swelling, fever, infection, hemorrhage, or malignancy.17 Heat can increase the pain threshold, increase blood flow, wash out pain-producing metabolites, and decrease muscle guarding.9,17 Heat increases the extensibility of connective tissue and therefore should be combined with a low-stress prolonged stretch to increase flexibility.17
Electrical stimulation
Transcutaneous electrical nerve stimulation (TENS) is an effective management to decrease pain (Fig. 24-12).17 A TENS units should never be placed close to the heart in a patient with a pacemaker.11 TENS uses the gate theory to block pain by stimulating larger sensory fibers, which then block the smaller pain C fibers. C fibers innervate the synovium and joint capsule, so blocking pain perception in these fibers is beneficial to decreasing pain in patients suffering from arthritis.17 One study has shown decreased inflammation, joint volume, and joint pressure from use of TENS.17
Stretching
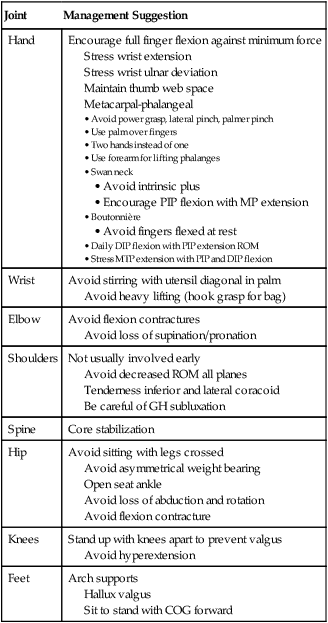
Stretching is an important component of exercise in arthritis because it can relieve stiffness, increase joint mobility, and increase muscle length.34 Intensity, duration, and frequency of stretching should take into consideration the phase of arthritis (Table 24-3).
Table 24-3
Joint-Specific Management Suggestions
| Joint | Management Suggestion |
| Hand | Encourage full finger flexion against minimum force Stress wrist extension Stress wrist ulnar deviation Maintain thumb web space Metacarpal-phalangeal |
Avoid heavy lifting (hook grasp for bag)
Avoid loss of supination/pronation
Avoid decreased ROM all planes
Tenderness inferior and lateral coracoid
Be careful of GH subluxation
Avoid asymmetrical weight bearing
Open seat ankle
Avoid loss of abduction and rotation
Avoid flexion contracture
Avoid hyperextension
Hallux valgus
Sit to stand with COG forward
In the acute phase patients should decrease activity and rest the inflamed joint.34 Splinting also helps to reduce pain and inflammation by immobilizing or supporting the joint.16 Reduced stress on the joint capsule and synovial lining through splinting reduces pain and inflammation.16 Rest is needed during the acute phase, but gentle ROM to maintain joint motion is still important. The goal of stretching in the acute phase is not to gain flexibility, but to maintain it, so do not overstretch the tissues. Tensile strength is decreased in inflamed tissues, therefore tears are more likely to occur. ROM exercise should be performed at least once a day to maintain proper flexibility.34
During the subacute or chronic phase of arthritis the goal is to increase flexibility, so a stretch at the end range of joint motion should be maintained. Intensity of the stretch should be gentle during subacute arthritis and aggressive during the chronic phase. Stretching should be performed two to three times a day with two to five repetitions performed on each joint.34 If symptoms are subacute, five warm-ups with two to five more aggressive stretches can help improve motion. When joint symptoms are chronic, three to five warm ups with one to two maximum tolerated stretches are recommended. Each stretch should be held 10 to 30 seconds depending on the pain involved.34 Pain should never last longer than 1 to 2 hours after exercise, but if pain persists longer than 2 hours, the intensity of exercise needs to be decreased.
Strengthening
There is an abundance of research supporting the benefits of exercise in rheumatic diseases. Muscle balance and conditioning are important aspects of physical activity because they provide joint stabilization and help the patient remain functional and independent with ADLs.25 In OA, regular exercise has been shown to decrease joint pain and disability.39 Exercise in patients with RA increases muscle strength and functional capacity without increased pain or medication.39 Furthermore, resistive training can improve muscle disability, physical performance, and pain with no increase in arthritic symptoms10; strong muscles can help absorb shock through a joint whereas weak muscles cannot provide stability or control.34 Strengthening is important, but is more effective when using the correct resistance for the phase of disease.
During an acute phase, resistive exercises need to be gentle with little pressure on the joints so that symptoms are not increased. Isometric exercises, those during which muscles are contacted without joint movement, are therefore recommended because of the minimal increase in joint pressure. Increased strength can also occur with isometric contractions held 6 seconds at 70% maximum effort and repeated 5 to 10 times a day.34 Placing the joint at midrange during contractions allows for safer exercise. If symptoms increase, decrease intensity to avoid joint irritation, but if pain does not subside 1 to 2 hours after exercise, the exercises should be terminated until the patient is past the acute phase of an arthritis flare-up.
When a patient reaches the subacute phase, isotonic exercises, those during which the muscle contracts against a constant load resulting in joint movement, should be implemented.34 The exercises should be performed through a pain-free ROM, but the American College of Sports Medicine states that 3 sets of 8 to 10 repetitions should be performed for each exercise.1 If the patient is older than 50 years of age, however, 10 to 15 repetitions are recommended.34 The appropriate amount of resistance is determined when the patient is able to perform all repetitions with no increase in symptoms but a minor feeling of fatigue at the end of each set. Once a patient can perform all repetitions easily, resistance should be increased slightly (1 to 2 pounds).25 When working with larger muscle groups, such as the chest, back, or leg, an increase of 5 pounds should not aggravate symptoms. Even though the joint is not in an acute flare-up, precautions should be taken to avoid exacerbation of symptoms. Open-chain exercises are less stressful on the joint because the weight of the body is not sustained by the joint. All major muscle groups should be addressed during exercise, but focus should be placed on muscles crossing the joint or joints affected by arthritis.
Aerobic Exercise
Aerobic activities are beneficial to all individuals for overall health and to decrease the risk of disease. Patients with arthritis often believe that rest is the only answer to decrease joint pain, but inactivity may actually exacerbate arthritic symptoms.25 RA has many extraarticular manifestations, so aerobic exercise is an especially important part of management. Aerobic activity should be performed three to five times a week for 20 to 30 minutes continuously.1 If the patient cannot tolerate 30 minutes of continuous exercise, the patient should be encouraged to perform several shorter activities throughout the day that add up to 30 minutes. As the patient’s cardiovascular endurance improves, the amount of time spent in continuous exercise may increase. The intensity of exercise should be 70% to 85% of the patient’s maximum heart rate (calculated as 220 minus age). The therapist should also explain that any hobby or activity that increases their heart rate can be considered exercise.
Aquatic Therapy
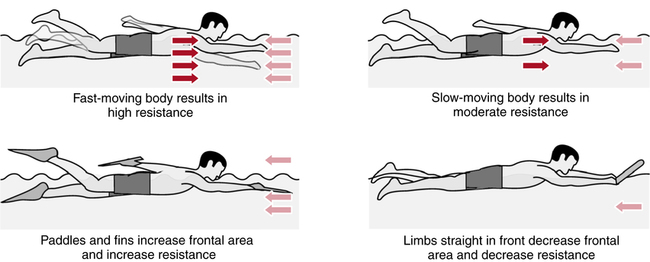
Water is an excellent medium to allow for an increase in pain-free movement while decreasing the stress on the joints. Aquatic exercise is unique because it can support, resist, or assist with exercises depending on the motion. Decreased joint compression, muscle relaxation, and sensory input from the pressure and temperature in the water help to decrease pain,34 so aquatic therapy programs can increase strength, flexibility, and aerobic fitness in patients with knee or hip OA.46 The resistance of water provides a means to strengthen muscles: the faster a patient moves through the water, the more resistance the patient experiences. Fins or water weights can be used to provide more resistance and progress strengthening (Fig. 24-13). The buoyancy of the water helps unload the body’s weight-bearing joints, which can decrease stress and pain. As the patient’s pain decreases and strength and endurance improve, the water level can be decreased to allow for more weight bearing. Recommendations from Minor33 are as follows:
 Select a pool with a water temperature of 84° F to 92° F (29° C to 33° C).
Select a pool with a water temperature of 84° F to 92° F (29° C to 33° C).
 Exercise in sufficiently deep water to minimize joint compression (midchest to shoulder level).
Exercise in sufficiently deep water to minimize joint compression (midchest to shoulder level).
 Use nonslip, padded footwear to reduce foot discomfort.
Use nonslip, padded footwear to reduce foot discomfort.
 Choose aquatic exercise programs specifically designed for people with arthritis.
Choose aquatic exercise programs specifically designed for people with arthritis.
 Receive instruction in proper technique before starting a swimming or deep water running program.
Receive instruction in proper technique before starting a swimming or deep water running program.
Medical Management of Rheumatic Disorders
Analgesics
The main role of an analgesic is to decrease pain, which is prevalent in patients with rheumatic disorders. Analgesics are primarily used with OA or in the early phases of RA, where inflammation is not as prevalent.31 There are several analgesics available to patients with rheumatic disorders, most notably acetaminophen, oxycodone, propoxyphene, and tramadol. Acetaminophen is one of the safest and most cost-effective drugs available. Other pain reducers, such as propoxyphene, oxycodone, and tramadol, are often used but have more side effects and higher risk of dependence. Tramadol is the least likely to cause dependence and is therefore often used first; however, tramadol does contain opioids, which decrease the sensation of pain through the central nervous system. Opioids can cause sleepiness, dizziness, and constipation.31 Education on the side effects is important so patients can report any side effects.
Nonsteroidal Antiinflammatory Drugs
NSAIDs have both analgesic and antiinflammatory effects but have no effect on arthritis progression.13 There are many NSAIDs, including ibuprofen (Motrin), aspirin, naproxen, indomethacin, meloxicam (Mobic), choline, and magnesium salicylates.9,31 NSAIDs inhibit cyclooxygenase (COX), which is an enzyme that converts arachidonic acid to prostaglandin, a molecule that has many roles including the promotion of inflammation and pain. COX has two different isomers: COX-1 and COX-2. COX-1 may be the main contributor in the adverse side effect of gastric bleeding and ulcers. COX-2 is mainly involved in inflammation of tissues; therefore, COX-2 inhibition may be the key factor in the use of NSAIDs.19,31
NSAIDs given at a lower dosage act more as an analgesic, but NSAIDS given at a higher dosage have more of an antiinflammatory effect. Low doses of NSAIDs may therefore be more appropriate with OA and early phase RA.6 Late phase or severe RA may require a higher dosage. Educating the patient on the importance of regularly taking their NSAID to get proper dosage is important. Symptoms should decrease in the first 2 to 3 weeks of NSAID use, however some patients will respond better to different medications, so a different NSAID should be tried if the patient does not feel any improvement after 3 weeks.19 Side effects to watch for include gastrointestinal bleeding and ulcers, dizziness, headaches, and drowsiness. Nausea and abdominal irritation are common and can be reduced by taking medication with food.31
Corticosteroids
Patients with inflammation as a primary symptom or who do not respond to NSAIDs are good candidates for corticosteroids.6 Several corticosteroids are available including prednisone, dexamethasone, hydrocortisone, and betamethasone.19,31 Corticosteroids are primarily used on a short-term basis to decrease symptoms and allow for other management methods to be used, such as physical therapy. Though corticosteroids usually provide the fastest and most effective antiinflammatory response long term usage has been shown to increase the risk of osteoporosis. Patients using corticosteroids should take precautions to make sure they get adequate calcium and vitamin D. Corticosteroids given by intraarticular injection should not be repeated more than three to four times in a year because of increased loss of blood supply to the bones. Oral and intravenous options are also available for giving corticosteroids. Most patients will feel a decrease in symptoms within 24 hours of dosage. Corticosteroids are often given along with NSAIDS or DMARDs.13
Disease-Modifying Antirheumatic Drugs
DMARDs are generally started as soon as a definite diagnosis of rheumatoid disease is made because they work in the early phases of the inflammatory process, can decrease arthritic symptoms, and possibly decrease the rate of damage to bone and cartilage.13,19,31 DMARDs decrease this damage by suppressing the immune system, but generally take several weeks to months to produce effects.9 DMARDs are primarily used with patients diagnosed with RA and systemic lupus erythematosus, but DMARDs may also used for psoriatic arthritis and ankylosing spondylitis.9,31
There are several types of DMARDs, including methotrexate, oral gold, penicillamine, sulfasalazine, and antimalarial drugs. Methotrexate is generally the first option for severe RA because of its long-term efficiency and its antiinflammatory and immunosuppressant effects.9,19,31 Methotrexate tends to produce results within 2 to 6 weeks, as opposed to other DMARDs that can take up to 6 months.19,31 As stated earlier, it is important for the PTA to be cognitive of side effects for each drug. Methotrexate side effects include nausea, vomiting, diarrhea, mouth ulcers, decreased white blood cell count, megaloblastic anemia, and liver fibrosis or cirrhosis.31
Oral gold was one of the first DMARDs that showed improved symptoms in the majority of patients, but it has several side effects that start to negatively impact the risk-to-benefit ratio. Penicillamine was another DMARD used; it has many adverse side effects with about the same amount of beneficial results as oral gold. Sulfasalazine has been shown to be effective in treating spondyloarthropathies and juvenile RA.9,31 Sulfasalazine has antibacterial, antiinflammatory, and immunomodulatory properties and has been shown to inhibit tumor necrosis factor-alpha which coordinates the autoimmune process.31,41
Biological Response Modifiers
The main purpose of biological agents is to inhibit the chemicals that are key factors in the inflammation and autoimmune processes. Unlike DMARDs, biological response modifiers target specific components of the immune system, thereby avoiding its widespread suppression.9 Two chemicals that current RA drugs are addressing are tumor necrosis factor (TNF) and interleukin-1 (IL-1). TNF is a cytokine that activates lymphocytes and leukocytes, two inflammatory cell types that destroy the synovium of joints.19,31 TNF inhibitors can be more effective than methotrexate in early phases of RA, but the two have been used in combination with favorable results.19 Side effects are minimal with TNF inhibitors, but can include fever, chills, dyspnea, hypotension, and possibly higher chances of infection.32 IL-1 receptor antagonist is designed to slow the rate of joint damage. This is done by blocking interleukin-1 alpha and beta, which play a role in immune and inflammatory responses in the body.
Supplements
Glucosamine and chondroitin sulfate are two safe supplements widely used for pain with arthritis.31 Glucosamine is a natural substance that is a precursor in the synthesis of glycosaminoglycans, which are present in cartilage. Glucosamine therefore helps the body build and repair cartilage.20 Chondroitin sulfate is a glycosaminoglycan and is thought to draw fluid into the cartilage, allowing for better joint function and protection from destructive enzymes.20,31 There are no serious side effects documented with either of these supplements and they are readily available.20,31,40 According to Richy and colleagues,40 patients taking glucosamine and chondroitin reported improved scores on a visual analog scale for both pain and mobility. These two supplements have an excellent safety record and have been shown to be effective in managing the symptoms of arthritis in the knee and hip.30
Surgical Management of Rheumatic Disorders
Synovectomy
A synovectomy is the removal of synovium infected with inflammation. Removing the inflamed synovium can decrease symptoms and prevent or slow destruction of a joint.9 Patients who continue to have inflammation after pharmacologic intervention are good candidates for this procedure; however, if the joint is degenerative without synovial inflammation then a synovectomy will not be beneficial. Synovium does grow back so the long-term benefits of a synovectomy are unknown.19
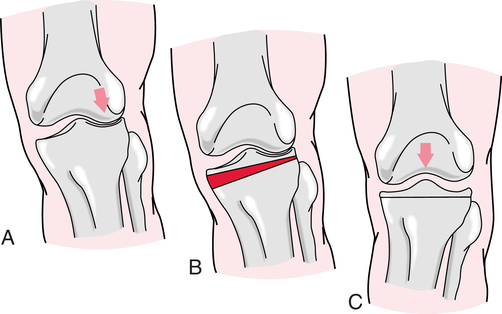
Osteotomy
An osteotomy is a procedure during which bone is cut to change the alignment of the joint to a better position (Fig. 24-14). Osteotomy can improve weight-bearing position of the lower extremities to aid in ambulation and is commonly used to correct coax vera, genu valgum, and genu varum.9 Osteotomy is one option that can be used to delay the need for a total joint replacement. During the rehabilitation of a patient after an osteotomy the therapist needs to be careful to not cause trauma or torque on the extremity. Stretching and exercise should be done in a gentle manner, and pain in these activities should last no longer than 1 hour. Osteotomy may be used for a patient with a spondyloarthropathy disease who has severe deformities of the lumbar spine.18
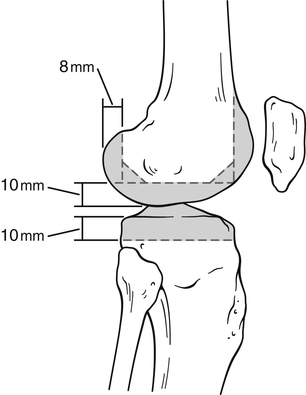
Resection
Resection is a procedure during which part or all of a bone is removed from a stiff or immobile joint, creating a space between the bones (Fig. 24-15). The empty space fills with scar tissue, which can be more flexible.9 Patients with severe arthritis of the foot can have bone resection in the foot to improve walking and pain. Other common sites for resections are the wrist, thumb, and elbow. The main goal of the surgery is to improve function and decrease pain.
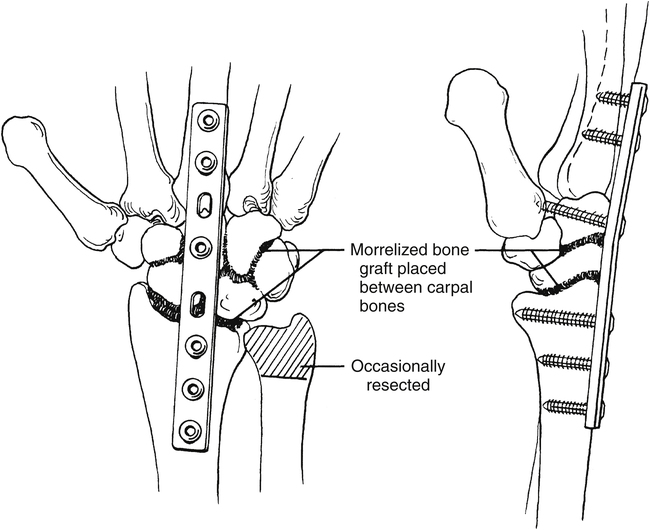
Arthrodesis
Arthrodesis is the artificial ossification between two bones or a bone fusion (Fig. 24-16). By fusing, the joint pain is decreased and the joint can better sustain weight. The two bones lose flexibility but are pain-free and sturdy.9 Common sites for arthrodesis are the ankles, wrists, fingers, and thumbs. Arthrodesis is used less commonly, but can be beneficial for a chronically infected and painful joint.19
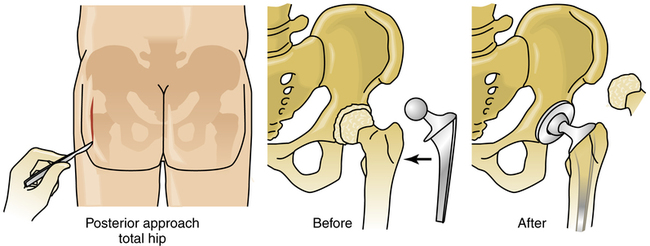
Arthroplasty
Arthroplasty is a procedure for rebuilding joints that have been damaged, become painful, and are less functional (Fig. 24-17). Total joint replacement is a very successful method for decreasing pain and improving the functional ability of individuals, but generally the surgery is used in people older than the age of 65 years because the new joint only lasts about 10 to 15 years. The arthritic joint is replaced with metal, ceramic, and plastic parts. The two most common joint replacements are knee and hip, but shoulder, elbow, ankle, and knuckles also can be replaced.19 In general, patients are expected to return to normal function, strength, mobility, and ROM after 6 months.3 Hip and knee arthroplasties are common surgical interventions in patients with OA24; total hip arthroplasty is the most common procedure in patients with ankylosing spondylitis.18
Arthroscopy
GLOSSARY
Atrophy A wasting; a decrease in size of an organ or tissue.
Infection The presence and growth of a microorganism that produces tissue damage.
Malaise Discomfort, uneasiness, or indisposition, often indicative of infection.
Proteoglycan A glycoprotein that retains water therefore providing more absorptive properties to the cartilage.2