CHAPTER 15 Revision Instability Surgery
Arthroscopic techniques to repair the unstable shoulder continue to evolve. Shoulder surgeons have embraced modern techniques to evaluate and anatomically repair the glenohumeral joint with minimally invasive procedures, reducing complications and stiffness. Historically, the absence of recurring dislocation has been equated with a successful outcome, but currently athletes and physically active individuals consider the return to their activity as the true measure of success.1–5 Return to sport and work following arthroscopic stabilization has been achieved based on a successful preservation of external rotation, improved outcomes in overhead athletes, and the avoidance of division of the subscapularis.6–9 Despite an emphasis on anatomic repairs, recurrence of instability is the most common complication of arthroscopic stabilization. To minimize the risk of recurrence, surgeons need to choose the best surgical approach when treating patients with failed shoulder instability surgery. The options for active individuals include arthroscopic stabilization, open stabilization, and possible augmentation with bone or soft tissue in complex revision situations.
Revision surgery is not as unusual as was once thought. Athletes and workers are likely to return to the activity that precipitated the initial injury.10,11 Surgeons continue to make surgical approach decisions based on anatomic lesions and anticipated activity demands.12 Surgical complications that have been reported include recurrence of instability, stiffness, joint pain, and hardware complications; the treatment goal is to return to physical activities and delay or prevent the onset of degenerative joint disease. The arthroscopic approach has met with success in secondary repairs and is an option for properly selected patients undergoing revision surgery.
Revision surgery adds challenges that are not always present when performing initial repairs. Additional trauma and soft tissue and bone changes following surgery can promote degenerative findings.13 Retained hardware, osteolytic changes secondary to implant choice, loss of tissue compliance, and incremental associated pathology can also further complicate treatment choices. As a result, revision surgical outcomes are not as promising as the results of the index surgery.14,15 The more anatomic the original repair, the easier to identify the causes of failure that need to be addressed.
ANATOMY AND PATHOANATOMY
The shoulder is comprised of static and dynamic stabilizers that allow maximal rotation with stability. Although surgery is directed at the static stabilizers, returning an athlete back to his or her sport requires a combined muscular rehabilitation program with repair of the essential lesions. Critical structures include the articular surface of the glenohumeral articulation, labrum, and capsular ligaments. Most experts have agreed that detachment of the labrum along with the capsular ligaments is the most common presentation following a glenohumeral dislocation.16,17 The inferior glenohumeral ligament combined with the superior labrum play a significant role in limiting anterior translation.18–20
Early surgical repair of recurrent instability has become popular as a result of improved outcomes. A progression of soft tissue and bone failure can follow multiple instability events.21 These changes may be permanent and affect the options that treating physicians need to consider. Although it remains controversial whether athletes should be repaired after a single dislocation, most would agree that surgery should be performed after recurrent subluxation or disability caused by apprehension is confirmed.
Following surgical repair, athletes often return to activities that place the shoulder at risk. After additional trauma and disruption of the failed surgical repair, there is often an acceleration of damage to the static stabilizers.22 Minor bone losses can become larger, further reducing the amount of contact and containment of the humeral head. Soft tissue changes in quality and mobility may become a challenge to the reconstructive surgeon.
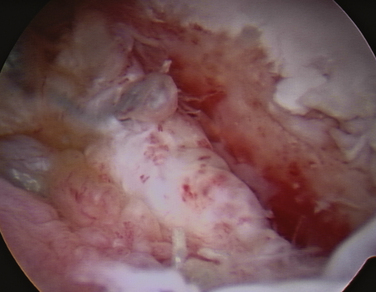
The most common findings following failure of previous stabilization is the re-creation of a capsule and labrum detachment, capsular pouch, glenoid rim erosion or fracture, and articular changes to the humeral head (Fig. 15-1).16,22,23 Other findings may include extension of injury into the rotator interval or superior labrum, loose bodies, and articular tears of the rotator cuff. These findings often occur in combination, and each of these features needs to be considered when deciding on the best approach to the damaged shoulder.
A concern for arthroscopic treatment of the unstable shoulder is the decision of whether a soft tissue procedure can compensate for bone loss. There have been reports of increased failure rates when anterior and inferior glenoid bone loss exceeds 25% to 30%.24,25 Internationally, the treatment has been to consider bone grafting through open or arthroscopic techniques.26–28 Most surgeons agree that bone loss needs to be considered during primary and revision surgery, and that anatomic repair of the detached labrum may be insufficient to return an athlete back to sport. Experts have not agreed on the amount of bone loss that becomes critical to consider a grafting procedure, but laboratory experiments can demonstrate measurable loss of stability when a glenoid rim deficiency exceeds 20%.29–31 It can be a challenge to quantitate bone loss, although a number of radiologic techniques have been proposed.25,30–33 Operative evaluation may be necessary to appreciate the combined impact of glenoid rim and humeral head deficiency.34
Displaced glenoid rim fractures can be problematic when considering revision surgery. These fractures are often medialized with the displaced labrum in a position that does not contribute to limiting anteroinferior translation.35,36 Some fractures may present as nonunions or fibrous unions; others may actually heal to the glenoid neck in a medial position (Fig. 15-2).37
The anterior dislocated shoulder will also demonstrate a humeral head impression defect that is created in the dislocated position as a result of impaction against the anterior glenoid rim. Duration and frequency of dislocations, combined with muscular force resisting reduction, play a role in the size and shape of the defect. This value needs to be considered in combination with glenoid deficiency when considering the sum effect of this pathologic condition (Fig. 15-3). The position of the shoulder when dislocation occurs will dictate the orientation of the Hill-Sachs lesion. As the lesion becomes more vertical, engagement can occur with less shoulder elevation. This may increase the likelihood of recurrence and potentially complicate activities of daily living.
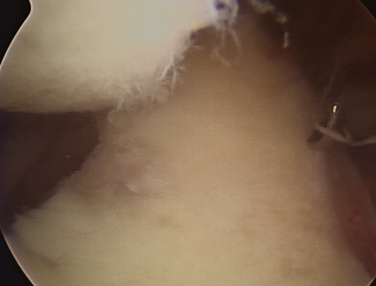
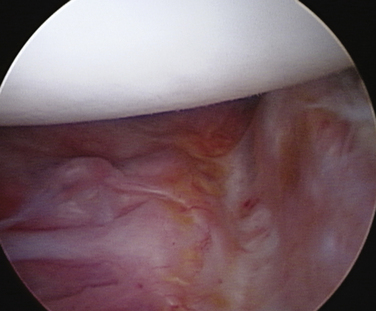
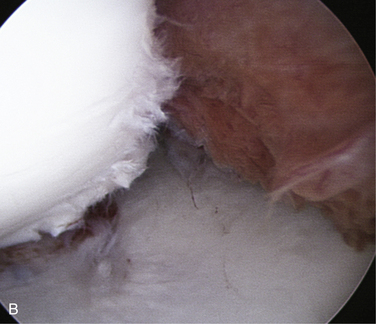
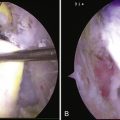
Soft tissue changes following failed stabilization include synovitis, labral detachment and involution, soft tissue stiffness, and adhesions to neighboring structures (i.e., the subscapularis). Tissue mobility is a critical step in repositioning the labrum and inferior ligaments onto the glenoid. To re-create the compression concavity of the normal articulation, the soft tissue bumper needs to be able to be repositioned on top of the glenoid rim. Following surgical failure, there is often additional scarring to the medial glenoid neck and subscapularis. This has been called an ALPSA (anterior labral periosteal sleeve avulsion) lesion.38 Careful mobilization and repositioning of this tissue is required if an anatomic repair is being considered (Fig. 15-4).
A recurrent labral detachment may resemble the original Bankart lesion or can extend beyond the previous limits. The detachment may extend posteriorly along the inferior aspect of the glenoid and superiorly to the base of the biceps. Additional trauma combined with tissue stiffness can be partially responsible for the enlarged defect. It is essential for the surgeon to visualize the boundaries of the lesion and to assess the degree of damage to the capsule, labrum, and bony structures so that specific treatment can be applied. The rotator interval is the region between the superior border of the middle glenohumeral ligament and superior glenohumeral ligament. Although normal intervals have not been defined, most surgeons agree that closure or reduction of the interval should be considered in revision surgery. This is accomplished in an inferior to superior fashion to augment the anterior repair and reduce translation.39 Tightening this interval may be a concern in overhead throwing athletes, and absorbable versus permanent sutures may be considered. The superior labral attachments and rotator interval play a role in limiting anterior translation and assist the function of the inferior glenohumeral ligament.20,40
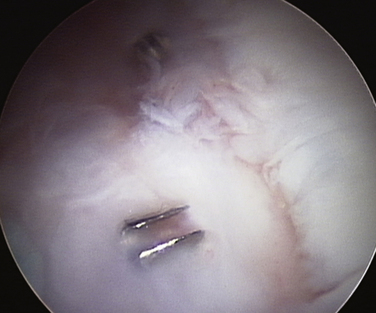
Foreign bodies may play a role in developing a painful shoulder following prior surgical stabilization. Metallic and nonmetallic anchors may have become displaced during the traumatic event. Exposed hardware is harmful to the articulation and needs to be removed as soon as the diagnosis is confirmed to limit articular cartilage injury.41,42 Permanent suture material can be embedded in the articular cartilage, creating painful impingement and a sense of subluxation. Removal of foreign matter is an important part of joint débridement prior to considering further repair.
The rotator cuff and biceps may exhibit pathologic changes. Although this was thought to occur in patients older than 40 years, these injuries can be found in younger patients. Rotator cuff tears vary from partial-thickness tears in young athletes to full-thickness tears in adults.43 In addition, subscapularis avulsions may be an important discovery in patients who have undergone prior open surgery.44 Review of previous operative reports is important when considering tissue failure and possible revision surgery.
HISTORY AND PHYSICAL EXAMINATION
The event that created recurrent instability should be reviewed when obtaining a history:
Special tests for shoulder instability include translation tests, apprehension tests, relocation tests, and the superior labral and biceps test, most commonly performed in the seated and supine patient. Translation tests include a load and shift test, which begins with the examiner centering the humerus and stabilizing the scapula. Translation is tested anteriorly, inferiorly, and posteriorly and compared with the other extremity. The arm is initially examined in the neutral position with 20 degrees abduction and retested in a position that would normally tension the involved ligaments (i.e., 45-degree abduction and 45-degree external rotation; Fig. 15-5). Evaluate patients in these positions for pain or apprehension. Apprehension may be demonstrated by verbal concern, visual awareness, or reflexive muscle contracture to try to avoid this position. A supine relocation maneuver can be performed with direct pressure added in the opposite direction, relieving apprehension and pain. Additional shoulder rotation is often demonstrated with this additional step. The superior labrum is evaluated by a combination of translation test and biceps traction tests in the seated patient. This can be accomplished by resisting forward flexion with the palm up, the O’Brien test with the thumb down, and resistance to elbow flexion. Localized tenderness along the biceps groove can lead to suspicion of additional pathology to the biceps, superior labrum, and rotator interval.
DIAGNOSTIC IMAGING
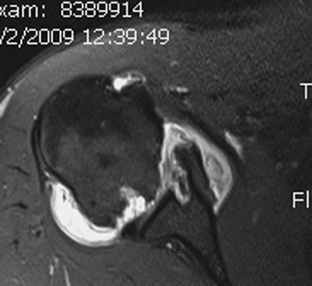
Careful preoperative imaging is critical to proper patient selection. Radiographs of the shoulder when dislocated are helpful, if available, to confirm the direction and degree of instability. Postreduction radiographs of the humerus and glenoid can identify fracture, glenoid loss, and the possibility of a Hill-Sachs lesion on the posterolateral humeral head.. Typical views include an anteroposterior view of the scapula, trans-scapular or Y view, and axillary view. Additional views of the glenoid (e.g., West Point view) can further demonstrate anterior glenoid pathology while rotation views of the humerus can delineate impression fractures. Metallic hardware from previous surgery is best seen with plain radiographs. In surgical revision cases, additional imaging may be desirable. Because anterior glenoid erosion can be a concern for arthroscopic repair, more detailed imaging can be obtained with computerized scans and three-dimensional reconstruction images. Magnetic resonance imaging (MRI) can assess soft tissue and labral deficiency, as well as absorbable hardware location (Fig. 15-6). When concerned about significant bone loss, the computed tomography (CT) scan provides more reliable information when compared with the MR study. Contrast agents can be added to these scans and are helpful in subtle cases of labral tearing, as well as assisting with clarifying artifactual images from prior surgery. Most soft tissue injuries can be assessed arthroscopically whereas bone loss may be the most important factor to be estimated preoperatively. A treatment strategy should be in place following the history, physical examination, and imaging studies.
INDICATIONS AND CONTRAINDICATIONS
Patients with failed stabilization surgery can be challenging. Arthroscopic intervention has gained popularity because of its ability to visualize articular lesions, preserve the subscapularis attachments, provide combined anterior and posterior treatment directly to damaged structures, and reduce the risk of stiffness and infection.6
The ideal arthroscopic candidate is a patient with a traumatic event that caused recurrent instability who has minimal bone loss on imaging studies, is an overhead athlete, and has failed nonoperative management. The effectiveness of arthroscopy diminishes as bone loss becomes a factor. Contact or collision athletes with demonstrable glenoid deficiency encounter higher failure rates.24,45 Large Hill-Sachs lesions with minor glenoid loss may be managed with arthroscopic tenodesis of the infraspinatus to the defect. Purchase and colleagues46 have referred to the Connolly procedure as a “remplissage” when performed arthroscopically. Arthroscopic bone grafting techniques to the glenoid and humerus are being developed.47 These procedures are new and few experts have had long-term experience. These techniques may, in time, expand the effectiveness of arthroscopic revision surgery.
Current relative contraindications to arthroscopic revision repair are excessive bone loss, capsular insufficiencies, atraumatic recurrence of instability, and certain capsular dependent collision sports (e.g., wrestling). In patients with a minor Bankart lesion following a traumatic dislocation, surgeons need to be suspicious of additional factors that may place the shoulder at risk for recurrent instability. Sports that create capsular deformation and lateral capsular injury (i.e., HAGL [humeral avulsion of glenohumeral ligaments]) are best treated by an open approach, particularly because of the proximity of neurologic structures.48 Capsular damage can be addressed with overlapping flaps commonly performed with open repair.49 In the future, these techniques will be performed arthroscopically as instrumentation and techniques improve.
Other contraindications include atraumatic onset after a previously well-performed arthroscopic suture anchor repair. The reasons for failure are often unclear, and an open approach allows for additional capsular reinforcement medially and laterally.50 Treating deficient glenoid rims, Hill-Sachs lesions, or capsular necrosis following thermal treatment is currently being performed as an open surgical procedure.
TREATMENT OPTIONS
There are very few reports on arthroscopic techniques to revise failed surgical stabilization.51–55 This may be because most stabilization procedures are successful and there is a paucity of revision material. Furthermore, the literature suggests that open revision procedures are more secure and therefore should be used as the primary choice for failed surgery.14,15 Because higher success rates have been reported with modern suture anchor techniques, arthroscopic techniques have been applied to the failed stabilization procedures.. The risk factors that influence the success of primary repairs are the same factors that dictate the success rate when performing revision surgery.28
Kim and associates51 have reported on 23 patients who underwent arthroscopic revision surgery. Of these patients, 3 had a recurrence, and 2 others demonstrated positive apprehension tests (78% stable), They emphasized creating an anatomic repair using up to four to seven anchors, with inferior placement critical to success.
Neri and coworkers52 have reviewed 12 patients with early failure following surgical stabilization. A 73% success rate after arthroscopic revision surgery was reported. Although the numbers were small, the authors favored this approach in athletes participating in noncontact sports. They restated the concern that previous surgery failed to recreate the anterior bumper and deepen the glenoid because of poor anchor placement. Although their study concluded that failure is often the result of medially placed anchors, the additional bone loss that occurs following a failed Bankart, can be misleading and can make the previous fixation points appear to be medially placed.
Creighton and colleagues53 have reviewed 18 patients. They emphasized that more than 25% glenoid bone loss is excessive and recommended an open procedure. Of the shoulders that were repaired arthroscopically, 83% remained stable. Additional anchors, posterior plication sutures, and interval closure were thought to add stability to the final repair. Athletes were likely to return to their sport, but workmen’s compensation cases were less predictable with regard to returning to work.
Franceschi and associates54 have performed arthroscopic revision surgery on 10 patients who had prior arthroscopic stabilization; 9 of the 10 returned to sports participation. This study had a minimum of 4 years follow-up, and patients with significant bone loss were excluded.
Boileau and coworkers55 performed arthroscopic revision surgery on 22 patients with failed open repair. Procedures included a suture anchor repair, capsular plications, and hardware removal, resulting in 3 patients with continued instability. The greater concern was the continued pain in half of these patients, who developed osteoarthritis after their open surgical procedure.
Conservative Treatment
Conservative treatment is an option and is often the first step after instability recurrence following a shoulder repair. Patients who have been satisfied for a long period of time and have low physical demands may choose a nonoperative program. Patients with continued apprehension and instability recurrence are more likely to choose surgical revision. Contraindications to conservative treatment include displaced glenoid fractures, subscapularis avulsions, and displaced hardware within the joint. In these cases, there is an opportunity to reduce the risk of permanent joint injury with early intervention.
Arthroscopic Techniques
The surgical procedure begins with an examination of the shoulder under anesthesia. Using a load and shift test, the affected shoulder can be compared with the contralateral side. The humeral head is pressed into the glenoid on a supine patient. This is followed by translation anteriorly, posteriorly, and inferiorly. The test is repeated with varying degrees of abduction and external rotation to test the tensioned ligaments specifically (see Fig. 15-5).56 Abduction and external rotation will stress the anterior inferior glenohumeral ligament (IGHL) and flexion and internal rotation will test the posterior band of the IGHL. The degree and directions of increased translation are often guides to the degree of anticipated capsular plication.
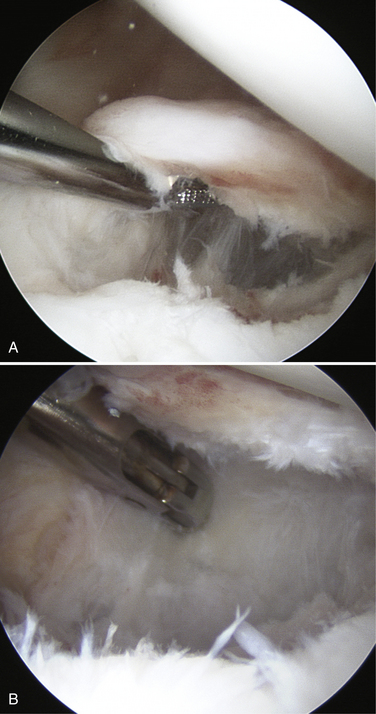
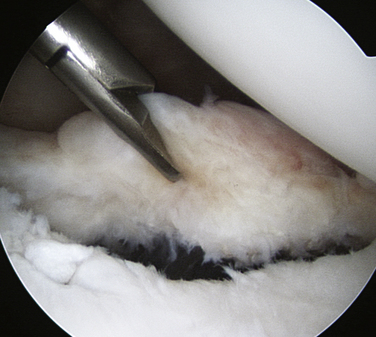
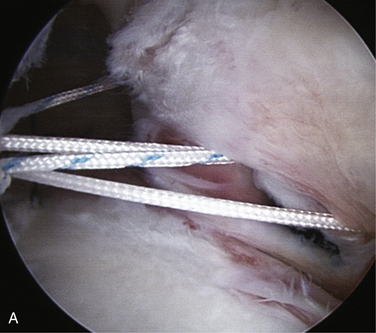
Anterior arthroscopic portals are created with an outside to inside approach. A needle is placed inferior to the acromioclavicular joint, entering below the long head of the biceps junction with the superior labrum. A cannula is placed here. A second more lateral portal is created lateral to the coracoid, entering the joint above the superior margin of the subscapularis. A second cannula is placed. A liberator or elevator is used to mobilize the labrum from the glenoid neck from superiorly to inferiorly. A shaver blade can be introduced to remove debris from the glenoid neck and undersurface of the capsule. Further separation of the capsule from the subscapularis allows mobility of the inferior capsule complex (Fig. 15-7). A suction punch may be necessary to create this plane of dissection. Note that the axillary nerve is visible at the inferior border of the subscapularis. The dissection continues inferiorly and potentially posteriorly if the labral detachment is shaped like a hockey stick. Move the arthroscope to the anterosuperior portal for the best view of the anteroinferior glenoid. Access to the inferior quadrant can be accomplished with the anteroinferior and posterior portals. Assessment of bone deficiency should be reevaluated with this view. The head will often rest on the anterior edge, possibly engaged anteriorly. Reassess tissue mobility with an atraumatic grasper (Fig. 15-8).
Begin in the posterior inferior quadrant. Use a fenestrated shaver to avoid tissue damage in the posterior portal and abrade the capsule and labrum posterior to the Bankart lesion. Use a suture hook and grasp full-thickness bites of the inferior capsule and pass under the posterior labrum. If the posterior labrum is deficient or detached, a suture anchor can be placed into the glenoid from a posterolateral skin puncture. Small anchors can be inserted at 6 and 7 o’clock from this approach (Fig. 15-9). The purpose of this suture is to reduce the pouch and secure the repair, allowing for increased tension applied to the anterior inferior capsule with additional anchors. Some surgeons tie the sutures at the end of the procedure to maximize visibility when performing the anterior repair.
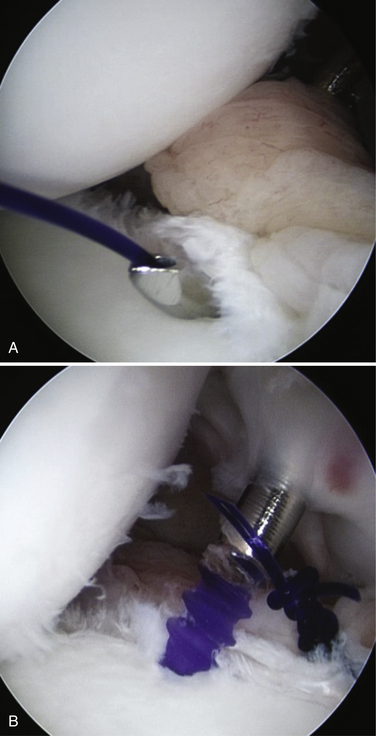
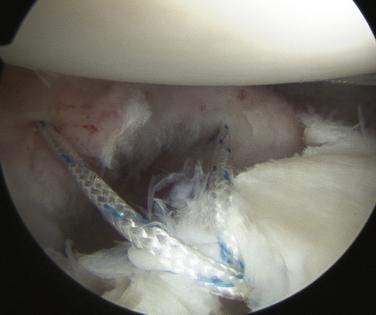
The drill and suture anchor are placed through the anterior inferior cannula to the 5:30 o’clock position of the (right) glenoid. A left suture hook is placed in the posterior portal, and the braided suture is retrieved posteriorly to the Bankart lesion. The simple suture is tied. An anchor is placed 8 to 10 mm above the previous anchor and a right suture hook is used to pass inferior and lateral to retrieve one arm of the suture. A second right hook pass is passed 1 cm superior to the prior suture and the second arm is retrieved to create a mattress suture (Fig. 15-10). An additional anchor is placed 1 cm above, and the process is repeated. The inferior glenohumeral IGHL can generally be reapproximated with mattress sutures. The superior anchor becomes the fixation point for the middle glenohumeral ligament, so simple sutures may be sufficient (Fig. 15-11). Periodically, take the arm out of traction, evaluate the resting position of the humerus, and visualize the Hill-Sachs lesion relative to the glenoid with elevation and rotation. Additional capsule plication sutures can be placed in the midcapsule to create additional tension and capsular thickness.
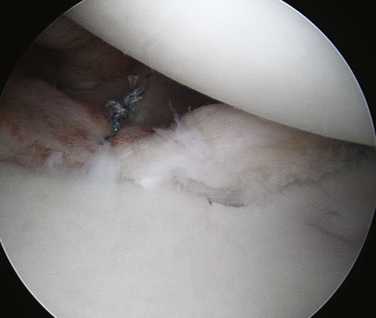
FIGURE 15-11 Combined simple sutures of anterior middle ligament with mattress sutures inferiorly in right shoulder.
Large Hill-Sachs lesions may be a consideration for an infraspinatus transfer. Place the arthroscope in the subacromial space and develop the interval between the infraspinatus and deltoid. Return the arthroscope to the anterior superior articular portal and use a needle to identify the percutaneous pass of a suture anchor into the abraded humeral head. A piercing instrument can be used to make several passes creating mattress sutures. Another option is to use a second anchor 1.5 cm away from the previous anchor. Replace the arthroscope in the subacromial bursae and the mattress sutures or sutures between anchors to compress the tendon into the defect (Fig. 15-12). A posteriorly directed force on the humerus will help at this point. The shoulder portals are closed, and the shoulder is placed in a protective brace.
PEARLS& PITFALLS
PEARLS
PITFALLS
CONCLUSIONS
The measure of success of shoulder revision surgery is the ability to return an athlete or worker back to her or his desired lifestyle. Early intervention of recurrent instability offers the best chance of successful repair of anatomic restraints. With a dislocation recurrence, arthroscopic and open options are available to patients with persisting complaints. Arthroscopy has become a popular technique to evaluate the articular structures and continue with an arthroscopic revision or convert to an open repair based on intraoperative findings. Superior labrum anteroposterior (SLAP) repairs, capsulolabral avulsions, or combined posteroinferior and anterior repairs that require additional visualization favor an arthroscopic revision approach. Concerns with extensive bone loss and soft tissue deficiency may be relieved by grafting. The development of degenerative joint changes increases following recurrent subluxation and failed surgical procedures.
1. Rowe CR, Patel D, Southmayd WW The Bankart procedure: A long-term end-result study. J Bone Joint Surg Am, 60; 1978:1-16.
2. Hovelius LK, Sandstrom BC, Rosmark DL, et al Long-term results with the Bankart and Bristow-Latarjet procedures: recurrent shoulder instability and arthroplasty. J Shoulder Elbow Surg, 10; 2001:445-452.
3. Kim SH, Kwon-Ick Ha, Cho YB, et al Arthroscopic anterior stabilization of the shoulder: two- to six-year follow-up. J Bone Joint Surg Am, 85; 2003:1511-1518.
4. Carreira DS, Mazzocca AD, Oryhon J, et al A prospective outcome evaluation of arthroscopic Bankart repairs: minimum 2-year follow-up. Am J Sports Med, 34; 2006:771-777.
5. Marquardt B, Witt KA, Liem D, et al. Arthroscopic Bankart repair in traumatic anterior shoulder instability using a suture anchor technique. Arthroscopy. 2006;22:931-936.
6. Abrams JS. Role of arthroscopy in treating anterior instability of the athlete’s shoulder. Sports Med Arthrosc. 2007;15:230-238.
7. Bottoni CR, Smith EL, Berkowitz MJ, et al Arthroscopic versus open shoulder stabilization for recurrent anterior instability: a prospective randomized clinical trial. Am J Sports Med, 34; 2006:1730-1737.
8. Sachs RA, Williams B, Stone ML, et al Open Bankart repair: correlation of results with postoperative subscapularis function. Am J Sports Med, 33; 2005:1458-1462.
9. Scheibel M, Tsynman A, Magosch P, et al. Postoperative subscapularis muscle insufficiency after primary and revision open shoulder stabilization. Am J Sports Med. 2006;34:1586-1593.
10. Ide J, Maeda S, Takagi K Arthroscopic Bankart repair using suture anchors in athletes: patient selection and postoperative sports activity. Am J Sports Med, 32; 2004:1899-1905.
11. Mazzocca AD, Brown FMJr, Carreira DS, et al. Arthroscopic anterior shoulder stabilization of collision and contact athletes. Am J Sports Med. 2005;33:52-60.
12. Cole BJ, L’Insalata J, Irrgang J, Warner JP Comparison of arthroscopic and open anterior stabilization: a two- to six-year follow-up study. J Bone Joint Surg Am, 82; 2000:1108-1114.
13. Pelet S, Jolles BM, Farron A Bankart repair for recurrent anterior glenohumeral instability: results of twenty-nine years’ follow-up. J Shoulder Elbow Surg, 15; 2006:203-207.
14. Zabinski SJ, Callaway GH, Cohen S, Warren RF Revision shoulder stabilization: 2- to 10-year results. J Shoulder Elbow Surg, 8; 1999:58-65.
15. Levine WN, Arroyo JS, Pollock RA, et al. Open revision stabilization surgery for recurrent anterior glenohumeral instability. Am J Sports Med. 2000;28:156-160.
16. Bankart ASB. The pathology and treatment of recurrent dislocation of the shoulder joint. Br J Surg. 1938;26:23-29.
17. Rowe CR, Zarins B, Ciullo JV Recurrent anterior dislocation of the shoulder after surgical repair: apparent causes of failure and treatment. J Bone Joint Surg Am, 66; 1984:159-168.
18. Turkel SJ, Panio MW, Marshall JL, Girgis FG. Stabilizing mechanisms preventing anterior dislocation of the glenohumeral joint. J Bone Joint Surg Am. 1981;63:1208-1217.
19. McMahon PJ, Burkart A, Musahl V, Debski RE Glenohumeral translations are increased after a type II superior labrum anterior-posterior lesion: a cadaveric study of severity of passive stabilizer injury. J Shoulder Elbow Surg, 13; 2004:39-44.
20. Rodosky MW, Harner CD, Fu FH. The role of the long head of the biceps muscle and superior glenoid labrum in anterior stability of the shoulder. Am J Sports Med. 1994;22:121-130.
21. Habermeyer P, Gleyze P, Rickert M Evolution of lesions of the labrum-ligament complex in posttraumatic anterior shoulder instability: a prospective study. J Shoulder Elbow Surg, 8; 1999:66-74.
22. Meehan RE, Petersen SA. Results and factors affecting outcome of revision surgery for shoulder instability. J Shoulder Elbow Surg. 2005;14:31-37.
23. Hayashida K, Yoneda M, Nakagawa S, et al Arthroscopic Bankart suture repair for traumatic anterior shoulder instability: analysis of the causes of a recurrence. Arthroscopy, 14; 1998:295-301.
24. Burkhart SS, DeBeer JF Traumatic glenohumeral bone defects and their relationship to failure of arthroscopic Bankart repairs: significance of the inverted-pear glenoid and the humeral head engaging Hill-Sachs lesion. Arthroscopy, 16; 2000:677-694.
25. Gerber C, Nyffeler RW. Classification of glenohumeral joint instability. Clin Orthop. 2002;400:65-76.
26. Edwards TB, Walch G The Latarjet procedure for recurrent anterior shoulder instability: Rationale and technique. Oper Tech Sports Med, 10; 2002:25-32.
27. Chen AL, Hunt SA, Hawkins RJ, Zuckerman D. Management of bone loss associated with recurrent anterior glenohumeral instability. Am J Sports Med. 2005;33:912-925.
28. Boileau P, Villalba M, Hery JY, et al. Risk factors for recurrence of shoulder instability after arthroscopic Bankart repair. J Bone Joint Surg Am. 2006;88:1755-1763.
29. Greis PE, Scuderi MG, Mohr A, et al. Glenohumeral articular contact areas and pressures following labral and osseous injury to the anteroinferior quadrant of the glenoid. J Shoulder Elbow Surg. 2002;11:442-451.
30. Itoi E, Lee SB, Berglund LJ, et al The effect of a glenoid defect on anteroinferior stability of the shoulder after Bankart repair: a cadaveric study. J Bone Joint Surg, 82; 2000:35-46.
31. Tauber M, Resch H, Forstner R, et al. Reasons for failure after surgical repair of anterior shoulder instability. J Shoulder Elbow Surg. 2004;13:279-285.
32. Itoi E, Lee SB, Amrami KK, et al. Quantitative assessment of classic anteroinferior bony Bankart lesions by radiography and computed tomography. Am J Sports Med. 2003;31:112-118.
33. Ito H, Takayama A, Shirai Y. Radiographic evaluation of Hill-Sachs lesion in patients with recurrent shoulder instability. J Shoulder Elbow Surg. 2000;9:495-497.
34. Burkhart SS, DeBeer JF, Tehrany AM, Parten PM. Quantifying glenoid bone loss arthroscopically in shoulder instability. Arthroscopy. 2002;18:488-491.
35. Sugaya H, Moriishi J, Kanisawa I, Tsuchiya A. Arthroscopic osseous Bankart repairs for chronic recurrent traumatic anterior glenohumeral instability. J Bone Joint Surg Am. 2005;87:1752-1760.
36. Porcellini G, Campi F, Paladini P. Arthroscopic approach to acute bony Bankart lesion. Arthroscopy. 2002;18:764-769.
37. Sugaya H, Moriishi J, Dohi M, et al. Glenoid rim morphology in recurrent anterior glenohumeral instability. J Bone Joint Surg Am. 2003;85:878-884.
38. Neviaser TJ The anterior labroligamentous periosteal sleeve avulsion: A cause of anterior instability of the shoulder. Arthroscopy, 9; 1993:17-21.
39. Mologne TS, Zhao K, Hongo M, et al The addition of rotator interval closure after arthroscopic repair of either anterior or posterior shoulder instability: effect on glenohumeral translation and range of motion. Am J Sports Med, 36; 2008:1123-1131.
40. Harryman DTII, Sidles JA, Harris SL, Matsen FA. The role of the rotator interval capsule in passive motion and stability of the shoulder. J Bone Joint Surg Am. 1992;74:53-66.
41. Kaar TK, Schenck RC, Wirth MA, Rockwood CA Complications of metallic suture anchors in shoulder surgery: a report of 8 cases. Arthroscopy, 17; 2001:31-37.
42. Rhee YG, Lee DH, Chun IH, Bae SC. Glenohumeral arthropathy after arthroscopic anterior shoulder stabilization. Arthroscopy. 2004;20:402-406.
43. Neviaser RJ, Neviaser TJ, Neviaser JS. Anterior dislocation of the shoulder and rotator cuff rupture. Clin Orthop. 1993;291:103-106.
44. Greis PE, Dean M, Hawkins RJ. Subscapularis tendon disruption after Bankart reconstruction for anterior instability. J Shoulder Elbow Surg. 1996;5:219-222.
45. Uhorchak JM, Arciero RA, Haggard D, Taylor DC. Recurrent shoulder instability after open reconstruction in athletes involved in collision and contact sports. Am J Sports Med. 2000;28:794-799.
46. Purchase RJ, Wolf EM, Hobgood ER, et al Hills-Sachs “Remplissage”: an arthroscopic solution for the engaging Hill-Sachs lesion. Arthroscopy, 24; 2008:723-726.
47. Lafosse L, Legeune E, Bouchard A, et al. The arthroscopic Latarjet procedure for the treatment of anterior shoulder instability. Arthroscopy. 2007;23:1242.
48. Arciero RA, Mazzocca AD. Mini-open repair technique of HAGL (humeral avulsion of the glenohumeral ligament) lesion. Arthroscopy. 2005;21:1152.
49. Deutsch A, Barber JE, Davy DT, Victoroff BN Anterior-inferior capsular shift of the shoulder: A biomechanical comparison of glenoid-based versus humeral-based shift strategies. J Shoulder Elbow Surg, 10; 2001:340-352.
50. Pagnani MJ, Dome DC. Surgical treatment of traumatic anterior shoulder instability in American football players. J Bone Joint Surg Am. 2002;84:711-715.
51. Kim SH, Kwon-Ick Ha, Kim YM Arthroscopic revision Bankart repair: A prospective outcome study. Arthroscopy, 18; 2002:469-482.
52. Neri BR, Tuckman DV, Bravman JT, et al. Arthroscopic revision of Bankart repair. J Shoulder Elbow Surg. 2007;16:419-424.
53. Creighton RA, Romeo AA, Brown FM, et al. Revision arthroscopic shoulder instability repair. Arthroscopy. 2007;23:703-709.
54. Franceschi F, Longo UG, Ruzzini L, et al Arthroscopic salvage of failed arthroscopic Bankart repair: a prospective study with a minimum follow-up of 4 years. Am J Sports Med, 36; 2008:1330-1336.
55. Boileau P, Richou J, Lisai A, et al. Arthroscopic revision of failed open anterior stabilization of the shoulder. In: Boileau P, editor. Shoulder Arthroscopy. and Arthroplasty, Current Concepts. Paris: Savramps Medical; 2006:117-130.
56. Abrams JS. Shoulder stabilization and evolving trends in arthroscopic repair. Sports Med Arthrosc. 1999;7:104-116.