Appendix 10 Systematic review of herbal immunomodulators
From a systematic review of the literature, Spelman et al.1 have identified a number of herbs as having their action through modulation of one or more cytokines. While some herbs were shown to stimulate pro-inflammatory cytokine secretion, other herbs had suppressive actions on these cytokines. Some herbs were shown to do both, depending on dosage, cell type and type of stimulus. It is important to know the context of the cells or animals used in order to know how results of in vitro, ex vivo (stimulation of cells to secrete cytokines after blood has been taken) and in vivo cytokine studies should be interpreted.
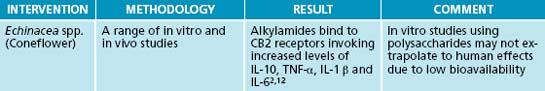
A case in point is that Echinacea purpurea was shown to stimulate pro-inflammatory cytokine production, in a manner comparable to lipopolysaccharides (Echinacea increased levels of IL-10, TNF-α, IL-1β and IL-6 (p < 0.05) more than culture medium alone).238 While this may be desirable in the early stages of a respiratory tract infection in order to hasten the cell-mediated response to an infection, it may not be desirable in an individual with an overactive cell mediated response.
It would appear from this study that Echinacea may be contraindicated in chronic inflammation. However, based on this one study, this conclusion would be quite premature. The human macrophages used for this in vitro study came from one 50-year-old female. Details of possible confounds for cytokine production, such as preexisting health concerns, atopic status, stress or inflammatory status or medication intake, were not given. Further, oestrogen levels are usually fluctuating widely at this time of life, and the presence of oestrogen receptors on macrophages may influence cytokine production. For this reason, most studies of cytokines exclude perimenopausal women, and many exclude women altogether. This finding can hardly be considered representative.
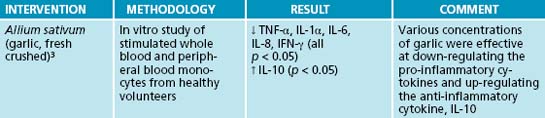
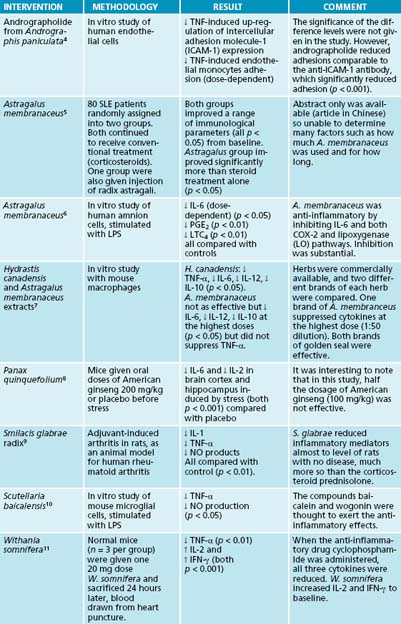
While in vitro studies are interesting, they must not be taken as a ‘gold standard’ on how a herb may affect cytokine profiles. There are so many factors that influence cytokine production and, by taking cells out of context, in vitro and ex vivo studies risk overlooking factors that regulate cytokine production in the plasma. It is also difficult to extrapolate the in vivo equivalent concentrations from herb concentrations that have been effective in vitro. Some herbs have been found to be suppressive at low concentrations and stimulatory at high concentrations in vitro.1 With these major methodological limitations in mind, those Western herbs included in the systematic review by Spelman et al.1 that were shown to suppress or inhibit pro-inflammatory cytokine production have been summarised in the table below. (see Table 6.4 in Chapter 6 for additional review).
1. Spelman K., et al. Modulation of cytokine expression by traditional medicines: a review of herbal immunomodulators. Altern Med Rev. 2006;11(2):128-150.
2. Burger RA, et al. Echinacea-induced cytokine production by human macrophages. Int J Immunopharmacol 1997; 19(7):371–379.
3. Hodge G., et al. Allium sativum (garlic) suppresses leukocyte inflammatory cytokine production in vitro: potential therapeutic use in the treatment of inflammatory bowel disease. Cytometry. 2002;48(4):209-215.
4. Habtemariam S. Andrographolide inhibits the tumour necrosis factor-α-induced upregulation of ICAM-1 expression and endothelial-monocyte adhesion. Phytother Res. 1998;12(1):37-40.
5. Cai X.Y., et al. Effects of radix Astragali injection on apoptosis of lymphocytes and immune function in patients with systemic lupus erythematosus. Zhongguo Zhong Xi Yi Jie He Za Zhi. 2006;26(5):443-445.
6. Shon Y.H., et al. Effect of Astragali radix extract on lipopolysaccharide-induced inflammation in human amnion. Biol Pharm Bull. 2002;25(1):77-80.
7. Clement-Kruzel S., et al. Immune modulation of macrophage pro-inflammatory response by goldenseal and Astragalus extracts. J Med Food. 2008;11(3):493-498.
8. Rasheed N., et al. Involvement of monoamines and proinflammatory cytokines in mediating the anti-stress effects of Panax quinquefolium. J Ethnopharmacol. 2008;117(2):257-262.
9. Jiang J., Xu Q. Immunomodulatory activity of the aqueous extract from rhizome of Smilax glabra in the later phase of adjuvant-induced arthritis in rats. J Ethnopharmacol. 2003;85(1):53-59.
10. Kim Y.O., et al. Cytoprotective effect of Scutellaria baicalensis in CA1 hippocampal neurons of rats after global cerebral ischemia. J Ethnopharmacol. 2001;77(2–3):183-188.
11. Davis L., Kuttan G. Effect of Withania somnifera on cytokine production in normal and cyclophosphamide treated mice. Immunopharmacol Immunotoxicol. 1999;21(4):695-703.
12. Gertsch J, et al. Echinacea alkylamides modulate TNFalpha gene expression via cannabinoid receptor CB2 and multiple signal transduction pathways. FEBS Lett 2004; 577(3): 563–569.