CHAPTER 130 Return to Competition Following Prolonged Injury
INTRODUCTION
Athletes can experience a variety of spinal injuries depending upon the nature of the sporting activity. Most injuries are relatively benign in nature, typically involving muscle strains. These injuries can be treated in a brief period of time with limited resources, allowing the athlete to quickly and safely return to competition. More serious or chronic injuries, including fractures, radiculopathies, or spondylolysis, may require an extensive evaluation and treatment plan prolonging the athlete’s recovery period. With a prolonged recovery comes the potential for deconditioning, further delaying the athlete’s return to competition. The challenge to the physician involves balancing the prompt recognition and treatment of the spine injury against the pressure to return quickly to competition and potential for recurrent injury.
EPIDEMIOLOGY
It is important to understand which sports have an increased risk for more severe injuries. Overall, it has been estimated that cervical spine injuries account for 2–3% of all athletic injuries.1 Fortunately, severe or catastrophic cervical spine injuries are rare. Typically the mechanism of injury involves cervical hyperflexion with concurrent axial loading. In football players,2 cervical hyperflexion, as may occur with spear tackling, has been proposed as the primary mechanism of cervical spine injury leading to spinal cord neurapraxia3 and cervical fractures. Similar cervical flexion-type injuries have been noted in athletes involved in gymnastics, diving,4 ice hockey, wrestling, trampoline, somersaulting, rugby,5 cheerleading, and motor sports. Fortunately, the use of protective equipment and improvement in equipment design in some sports has helped decrease the incidence of cervical spine injuries.6
Similar to cervical spine injuries, the incidence of low back injuries varies depending on sports and mechanism of injury. Several studies have suggested that lumbar spine injuries represent 10–15% of competitive sports injuries.7 Compared to cervical spine injuries, the mechanism of injury is more variable, relating to hyperflexion, hyperextension, and rotatory motions. Hyperflexion injuries can typically occur in football, ice hockey, and rowing. Gymnasts have been shown to have a higher incidence of spondylolysis compared to nonathletes, most likely due to repeated hyperextension and axial loading of the lumbar spine.8 Twisting and rotatory motions can contribute to lumbar pain in racquet sports and golf. It has been estimated that 10–30% of tour golf players experience lumbar spine pain.9 As with cervical spine injuries, lumbar spine injuries with neurologic compromise are rare, representing less than 1% of all sports injuries.9
ASSESSMENT
Examination of an athlete with a spine injury requires a fundamental knowledge of the underlying functional anatomy in relation to the rehabilitative process. The initial priority should include the assessment of spinal stability. A more aggressive evaluation of the spine may occur only once the physician is 100% certain there is no underlying spinal instability. The reader is referred to the previous chapters in this textbook for a complete discussion relating to the clinical evaluation of the cervical and lumbar spine. In addition, resources such as the PASSOR Musculoskeletal core competency list will provide a more detailed outline of the various physical examination tests.10
Of note, injuries in children are of particular concern due to the inherent ligamentous laxity. Cervical radiographs should be interpreted with caution as spinal cord injury can be seen without radiographic abnormality. Beck et al. concluded that children and adolescents who have neurological deficits and spinal cord injuries without radiographic abnormalities (SCIWORA) require close following of their deficits and further evaluation to define structural pathology and often require prolonged therapy.11
GENERAL TREATMENT PRINCIPLES
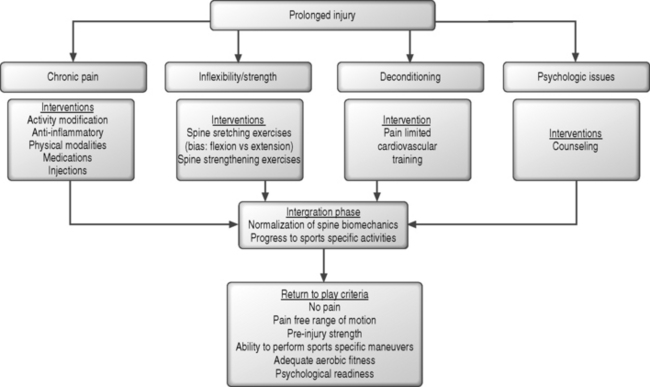
An appropriate treatment plan will depend upon the etiology and severity of, and secondary maladaptations associated with, the spinal injury. After an acute injury, the focus is on inflammation and pain control with the goal of promoting tissue healing. After prolonged injury, treatment interventions should be utilized in a systematic manner focusing on: (1) pain control, (2) correction of inflexibilities and strength deficits, (3) maintenance of cardiovascular stamina, (4) assessing any psychological barriers, and (5) reintegration into sports-specific activities. The general treatment outline is summarized in Table 130.1.
Table 130.1 General Principles for Recovery from Prolonged Spine Injuries
| I. INITIAL PHASE: PAIN CONTROL | |
| Activity modification | |
| Antiinflammatory medication | |
| Physical modalities | |
| Peripheral or axial injections | |
| II. RESTORATIVE PHASE: CORRECTING FLEXIBILITY AND STRENGTH DEFICITS | |
| Truncal and extremity stretching | |
| Soft tissue mobilization | |
| Cervical or lumbar stabilization strengthening exercise | |
| Maintenance of cardiovascular fitness | |
| III. INTEGRATIVE PHASE: FUNCTIONAL ADAPTATIONS | |
| Normalization of spine mechanics | |
| Progression towards sports-specific activities | |
| IV. RETURN TO COMPETITION | |
| Pain free | |
| Pain-free range of motion | |
| Pre-injury strength | |
| Ability to perform sports-specific maneuvers |
Pain control
Muscular strains and ligamentous sprains usually occur as a blow to the head or body creates rotary, sidebending and flexion–extension forces to the spine. Trying to maintain the head and neck in normal alignment by strong eccentric contraction creates muscle and ligamentous tearing by overcoming their tensile strength.12 It is during the acute pain period that the athlete may learn protective compensatory posturing, resulting in abnormal posture, thus leading to a chronic pain mechanism. The head protruded forward is commonly seen in those with poor posture secondary to habit or body habitus. A cycle of biomechanical derangements occurs, resulting in an alteration of the normal anatomy and alignments. Muscles meant to stabilize come to function as movers of the spine, leading to a further pattern of chronic myofacial pain syndrome.
In general, injury to a musculoskeletal structure such as a muscle or ligament will lead to a systematic process of degradation and repair. During the initial inflammatory phase, micro/macro tears and localized hematoma formation give way to phagocytosis and enzymatic degradation with subsequent tissue necrosis. Modalities to control the inflammatory process may play a role in limiting the extent of tissue damage during the initial stages. During the reparative phase, the body attempts to repair the injured area through collagen formation. However, the reparative process will lead to disorganized fibrous tissue without the appropriate applied stressors. Prolonged pain symptoms will inhibit the rehabilitative process by limited the amount of stress one can tolerate during the recovery process. Therefore, adequate pain control is imperative during the management of an athlete with prolonged injury. It is the basis for early mobilization and is the reason why soft tissue is not immobilized for a prolonged period, unless absolutely indicated by the injury.13
Unfortunately, evidence supporting the use of specific pain modalities in the athlete is lacking. In the general population, there is strong evidence that prolonged bed rest is detrimental to the functional recovery of individuals with acute low back pain without radiculo-pathy.14 It could be surmised that the principle of relative rest and the avoidance of bed rest in athletes will also facilitate earlier functional recovery. Fellander-Tsai et al.15 suggested some benefit from the use of modalities for pain relief in individuals with spondylolysis, including activity modification and electrical stimulation. However, the study had several design flaws including small sample size and selection bias. Various studies provided conflicting support as to the efficacy of interventional spinal injections.16,17 Finally, O’Sullivan et al.18 showed a signification reduction in pain intensity and utilization of pain medication at 30-month follow-up in a treatment group that underwent a 10-week exercise treatment program compared to controls. Future, randomized, controlled studies are need to better support or refute the utilization of these various modalities in managing a specific spinal injury in athletes.
Correction of inflexibilities and strength deficits
Spinal flexibility
However, evidence is limited as to the role of spine flexibility and injuries in athletes. In addition, a review of the literature pertaining to nonathletes yields conflicting reports as to the role of spine flexibility and range of motion in the treatment of spine injuries. Several recent studies outlined below have suggested that there is no correlation between spinal flexibility and disability or function. Kuukkanen et al. suggested that flexibility does not play an important role in the functional ability of individuals with back pain that is not severe in nature.19 Similarly, Sullivan et al. studied the relationship of active lumbar spine range of motion and disability. Using the Roland-Morris Back Pain Questionnaire and therapist assessments, they suggested that active lumbar spine flexion should not be used as a treatment goal.20 In contrast, Magnusson et al.21 studied a group of patients’ with chronic low back pain. The study suggested that increased trunk motion could be achieved by participation in a 2-week, full-time rehabilitation program. The authors suggested that motion was of ‘greater magnitude and was done at an increased velocity.’ In addition, patients who demonstrate a pain avoidance behavior can achieve the confidence to recover in spite of their pain. More comprehensive randomized, prospective studies are needed to better assess the role of spinal flexibility in the recovery process in athletes. Despite these limitations, the authors still advocate that athletes work on correcting any loss of spinal flexibility or range of motion. These flexibility exercises may be initiated at the beginning of the recovery period and in combination with the strength training once the pain is controlled. A flexion- or extension-based program will depend upon the specific limitations as per the physical examination.
Strength deficits
Addressing strength deficits is another primary focus of spine rehabilitation. Similar to the previous discussion of spinal flexibility, prolonged injury and pain can lead to muscle atrophy, altered spine biomechanics, and decreased athletic performance. There are a variety of spine exercise programs including spine stabilization exercises, McKenzie exercises, and Williams’ flexion exercises which are utilized to treat spine injuries based upon the etiology of the spine pain.22 However, there is limited study of the utility of these programs in the management of prolonged spine injuries in athletes. The following is a review of the various studies that have attempted to analyze the role of the spine muscles in supporting the spine, anatomical changes which occur from an exercise program, and efficacy in treating individuals with prolonged spine injuries.
In the lumbar spine, the superficial and deep truncal muscles are strengthened to assist with the control of the lumbar spine. Various studies have yielded conflicting results as to changes involving the superficial muscles of the lumbar spine. In contrast, the multifidus muscles are believed to be important in maintaining stiffness and strength of the lumbar spine.23,24 Zhao et al. suggested that functional inactivity may contribute to selective type 2 atrophy of the multi-fidus muscles in patients with lumbar disc herniations.25 Antigravity postural muscles have been shown to atrophy to a greater extent than lower extremity muscles in microgravity simulation models.26 Changes in muscle composition in healthy subjects who stopped normal repetitive low-level activity patterns is thought to result in transformation of the muscle towards a more fatigable type of muscle fiber.26,27 The implication is that muscles situated on the trunk and lower extremities are affected most by prolonged inactivity and deconditioning. Fortunately, it is believed that these changes are reversible with adequate therapy.
Various studies have looked at the anatomical changes in spinal muscles after a treatment exercise program. Hides et al. attempted to assess the recovery of lumbar multifidus muscles after treatment with an exercise program consisting of isometric contractions of these muscles with cocontraction of the abdominal muscles compared to medical treatment only for individuals following a nonradicular acute lumbar spine injury.28 These authors noted a more rapid and complete recovery of the multifidus muscles as measured by an improvement in the muscle symmetry. Sung studied the endurance of multifidus muscles and functional status of chronic low back pain patients after participation in a 4-week spinal stabilization program.29 Although the authors believed it was difficult to measure the isolated effect on the multifidus alone, they suggested the evidence did show a change in the multifidus strength in conjunction with other spinal extensor muscles. Finally, Danneels et al. analyzed effect of three different 10-week exercise training programs on the cross-sectional area of the paravertebral muscles in individuals with chronic lumbar spine pain.30 The authors suggested that a lumbar stabilization program combined with dynamic resistance training was necessary to restore the size of the paravertebral muscles. These studies would suggest that a structured lumbar exercise program can lead to anatomical improvement in the lumbar multifidus muscles.
Other studies have attempted to define the functional efficacy of a structured strengthening exercise program in the management of individuals with chronic lumbar spine pain. Unfortunately, there are few prospective, randomized studies. O’Sullivan et al.18 compared a treatment group utilizing strengthening of the deep abdominal muscles with coactivation of the lumbar multifidus to a control group in individuals with chronic low back pain and spondylolisthesis. The treatment group showed a significant improvement at 30 months in regards to pain, function, range of motion, and abdominal muscle recruitment. Mannion et al.27 performed a prospective study of three active exercise treatments (active physical therapy, muscle reconditioning on devices, and low-impact aerobics) over a 3-month period for individuals with chronic lower back pain. All three treatment exercises showed a similar increase in isometric strength in all lumbar planar movements, increase activation of the erector spinae during extension testing, and increased endurance testing as measured by the Blering-Sorensen test. The authors concluded that significant muscle performance was observed in all three exercise groups.
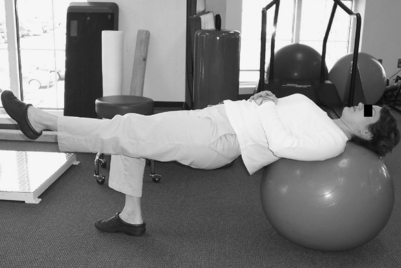
Though these studies were not specific to athletes, they would suggest that a structured strengthening program may be efficacious in the management of chronic spine injuries. In the lumbar spine, the program should focus on strength training of the deep intrinsic spinal muscles, such as the lumbar multifidus, with cocontraction of the abdominal muscles (Fig. 130.1). Indeed, many of today’s spinal rehabilitation programs incorporate control and strengthening of these ‘core’ muscles of the spine (Fig. 130.2). However, more comprehensive randomized, prospective studies are needed to better assess the efficacy of spinal strengthening exercises in treatment of athletes.
Maintenance of cardiovascular stamina
Despite the rationale for cardiovascular fitness during the recovery process, there are no definitive studies to suggest the effectiveness of a fitness program in athletes after a spinal injury. Wittink et al. noted in a prospective case series that patients with chronic low back pain had comparable level of aerobic fitness with those of healthy subjects.31 Though the authors suggested that aerobic fitness level was independent of diagnosis, duration of pain, pain intensity, or work status, they felt aerobic fitness training was a useful treatment modality. Sulco et al. studied low back pain patients who underwent a 10-week aerobic fitness training regimen. In the short term, improvements in mood profile were noticed, but not in pain levels. However, at 2.5-year follow-up, the exercise group received fewer pain medication prescriptions, was given fewer physical therapy referrals, and showed an improved work status in exercising patients.32 Future prospective studies are needed to better define the amount and efficacy of aerobic fitness training for athletes with specific diagnoses. Despite this need, maintenance of aerobic fitness should be part of a rehabilitation treatment program.
Psychosocial issues
All athletes, whether amateur or professional, may experience psychosocial issues, which may affect their recovery from a prolonged injury. For most athletes, this may pertain to the frustration of not being able to return to a specific sport in a certain period of time. For elite athletes, the issues may be more complex due to the many stakeholders including agents, trainers, and coaches. In addition, burnout can cause the athlete to regress during rehabilitation, which should put the training and medical staff on notice to look for the symptoms while following the athlete’s recovery.33 Therefore, the physician must be aware of these issues and the patient’s goals to develop a complete treatment program.
The impact on recovery of the manifestation of the psychological issues has been studies in both athletes and nonathletes with chronic low back pain. A few studies have found a relation to psychological distress and the development chronic back pain in workers.34,35 Sports psychology, while generally relating to a much different population, can, in some ways, draw parallels with regards to anxiety and fears of pain. If the athlete’s focus falters, a negative cycle can develop which can evolve into increased tension. It is important for the support team to help the athlete maintain high self-esteem and concentration. As noted above, burnout can occur from overtraining and erode the self-confidence and motivation of the athlete.
A stepwise approach with directed goals will help with maintaining a positive outlook for the athlete as he or she reaches for new levels of achievement during the course of rehabilitation. Fear of re-injury can be an inhibitory consequence of having low back pain. Patients often will not attempt certain activities due to a belief that it will worsen their condition. Obviously, this can be quite detrimental to progression in a therapeutic program. In patients with chronic low back pain, it has been shown that if they believe that their pain will worsen, significant disability and depression will be encountered.36 For these reasons, it is sometimes important to employ a sports psychologist to facilitate rehabilitation and ensure a smooth progression to eventual return to activity, as appropriate.
Reintegration in sports-specific activity
The final steps in the rehabilitation process involve integrating the athlete back into their sports-specific activity (Fig. 130.3). Progression from the basic flexibility and strengthening exercises of the spine will depend upon the athlete’s symptoms and performance needs. Athletes should begin these sports-specific motions under the guidance of the trainer or therapist. Such supervision will allow the trainer or therapist to review any biomechanical abnormalities which might impede the recovery process. In addition, the athlete should be pain free and without surgical restriction. Any asymmetry in muscle strength would limit the athlete’s progress toward the sports-specific activity.
The progression from basic to more complex motions will depend upon the subsequent forces placed on the spine. As an example, athletes participating in tennis should simulate a basic forehand or backhand swinging motion in a plane parallel to the ground. The motion should initially begin without any contact with the tennis ball or resistance measures, such as Therabands. Contact or resistance is then added in a linear plane with progression toward reaching in multiple planes as would occur in competition. Overhead volleys and serves should be avoided until the athlete is able to perform the above motions with fluidity and without pain. The athlete is then progressed to overhead serves and volleys which will place a greater amount of stress on the spine. Again, the motions should initially occur without any ball contact. The athlete can then progress from low-speed to high-speed motions with increased power as tolerated. A final decision allowing return to full activity should occur in the context of a complete medical recovery from the injury with the hopeful prevention of any future injury.
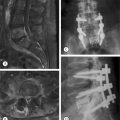
RETURN TO COMPETITION
The eventual return of the athlete to competition requires a balance of various factors. The physician must be sure the athlete has had adequate time to recover from the medical injury with a relative assurance that the athlete will not sustain a recurrent injury. The athlete must demonstrate a return to the pre-injury proficiency in athletic performance. The level of proficiency will vary depending upon the level of competition, external pressure from coaches, peers and agents, and timing of competition. In general, the athlete should be pain free, exhibit pre-injury range of motion and pre-injury strength. In addition, the athlete should be able to perform sport-specific maneuvers involving such movements as running, cutting, or jumping motions without any significant abnormal motions (Fig. 130.4).
Cervical spine
Several authors have suggested an algorithmic approach for treating injuries to the cervical spine. Wang el al.37 attempted to study the effectiveness of an algorithmic approach for treating different etiologies of cervical pain. Patients were grouped according to symptoms, including radicular arm pain or neck pain, referred neck or arm pain, cervicogenic headaches, and neck pain only. Treatment approaches included range of motion, traction, postural exercise, and joint mobilization. Based on the results, the authors determined that there was a place for individualized treatment approaches using such an algorithm. Beazell et al. suggested specific exercises for the cervical region to correct dysfunctional motion and restore posture.38 Exercises to facilitate proper posture include stretching of the pectoralis minor and the posterior shoulder depressors in addition to the trapezial and cervical paraspinal muscles. Other muscles that can be targeted to prevent muscle inhibition include the longus colli and lower trapezius. Maintenance of proper posture during reconditioning is emphasized to facilitate normal neuromuscular patterns that can carry over to sport-specific exercises. Scapular strengthening will help with stabilizing the shoulder in order to aid in maintaining cervical alignment. Prior to returning to sport, the athlete should be able to demonstrate appropriate cervical posture. As previously noted, criteria for return are pain-free range of motion, no abnormal neurologic signs, spinal stability, normal strength, and no provocative signs.
Torg and Ramsey-Emrhein39 proposed criteria for clinicians to use to help patients understand the risks of collision activities and to help make sound recommendations regarding participation in competition. The following are brief summarizations, and the reader is directed to the references for a full discussion of the recommendations. Congenital conditions such as odontoid anomalies and atlanto-occipital fusion are complete contraindications, while Klippel-Feil anomaly depend on the type and confounding pathology. Developmental cervical stenosis without evidence of instability does ‘not predispose athletes to permanent catastrophic neurologic injury’ and should not disallow the athlete from playing. However, athletes with a loss of ‘functional reserve’ as defined by obliteration of the protective cerebrospinal fluid around the spinal cord on MRI imaging should not participate in contact or collision sports.40 Those athletes with uncomplicated cervical cord neurapraxia or ‘stingers’ can be allowed to play without risking more serious neurologic injury.39 Spear-tackler’s spine as seen in athletes with developmental stenosis, straightening of the cervical column and post-traumatic radiographic abnormalities, is an absolute contraindication. There are no contraindications for athletes with single-level stable cervical fusions. However, athletes with 2–3-level fusions present a relative contraindication and those with more levels are absolutely contraindicated.
Lumbar spine
As an example, the treatment of lumbar spondylolysis and time to return to competition will vary depending upon the physician’s beliefs and preference. Standaert et al.41 recommended that athletes may return to competition if they are asymptomatic after 4–6 weeks with a mature corticated fracture on CT scan. If the CT scan shows an earlier-stage lesion with either a stress reaction or minimal separation with noncorticated or cystic margins, the athlete should rest for 12 weeks and no extensive physical activity beyond that associated with normal daily activities. After a gradual rehabilitation program and no symptoms, the athlete can progressively return to the sport. Cogeni recommended that athletes can return to competition if they are pain free during therapy, at rest, with lumbar hyperextension motions and specific athletic activity after 8 weeks from the diagnosis.42 Omey and Micheli recommend the application of a rigid brace for 6–9 months for athletes with early spondylolytic lesions before returning to sport.43
Despite the variation in treatment times, the overall goal is to allow adequate healing of the pars defect, relieving pain, and optimizing function. In each case, the athlete should not be allowed to return to play until demonstration of painless range of motion and relief of hamstring spasm, if present. The goal of physical therapy is to increase spinal stability, whether implemented in a brace or without a brace. However, prolonged brace use will require reconditioning. Physical therapy exercises have varied, but focus on targeting the deep abdominal muscles and lumbar multifidi.18,44 With time, most athletes will eventually return to competition. For a more complete discussion, the reader is referred to the earlier chapter on spondylolysis.
SPECIFIC CONCERNS FOR VARIOUS SPORTS
Running sports
Running athletes are less likely to experience back pain injuries compared to injuries involving the lower extremity. However, back pain injuries may represent approximately 2–11% of all running injuries.45 The majority of these injuries involve lumbar strains. Less common injuries that may lead to prolonged injury include lumbar radiculopathy, lumbar spondylolysis, lumbar spondylolisthesis, and lumbar stress fractures. Fortunately, the majority of lumbar spine injuries can be managed with medical rehabilitation and rarely require surgical intervention
In general, the compressive forces and flexion–extension moments generated in the spine during running are not believed to place the spine at an increased risk for injury. However, any biomechanical abnormalities that may increase the forces on the spine may contribute to lumbar spine injuries.45 During the running gait cycle, there appears to be coordinated movements for: (1) flexion–extension of the lumbar spine and anterior–posterior pelvic tilt, and (2) lateral bending of the lumbar spine and obliquity of the pelvis.46 The lumbar extensor muscles appear to exhibit significant muscular activation at the time of heel strike, assisting with truncal deceleration and stabilization of the pelvis. At the same time the peak compressive forces range from 2.5–5.7 times body weight at heel strike.47 Any lower extremity abnormality, such as excessive pronation, may increase internal tibial rotation placing increased stress on the lumbar spine.
Golf
Golfers experience one of the highest incidences of back pain for all sports. The incidence varies for amateur and professional athletes depending upon the study. The incidence in amateur athletes incidence ranges 25–46%, and in professional athletes range 30–40%.48 In the amateur golfer, the majority of golf injuries are due to technical error or biomechanical deficiencies.49 In professional golfers, the majority of injuries are due to overuse.50 In both types of athletes, the most common injury involves the lumbar spine including lumbar strains, lumbar radiculopathy, and lumbar spondylolysis.
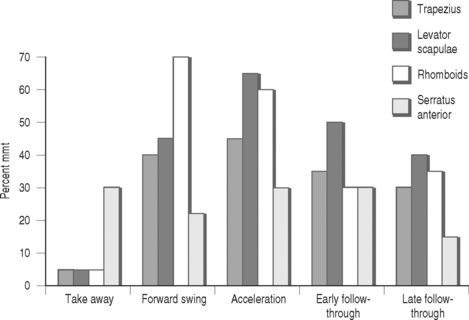
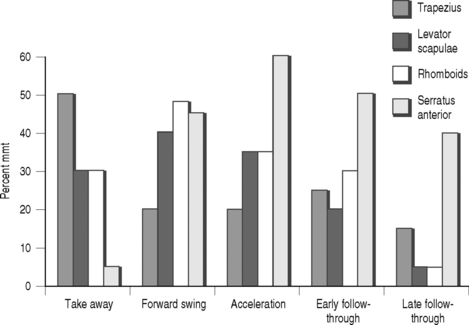
It has been suggested that poor swing mechanics may lead to an increased injury of the lumbar spine. Hosea and Gatt noted that compressive, rotatory, lateral flexion and anterior–posterior traction forces are applied to the lumbar spine during the golf swing.51 The spine may be particularly at risk during the take-away or back swing and late follow-through phases of the golf swing due to the compressive forces placed on the spine. The erector spinae and abdominal oblique muscles exhibit increased muscle activity throughout the golf swing. The erector spinae assist with stabilization, while the abdominal muscles contract for truncal flexion and rotation.52,53 For the scapular stabilizers: (1) the trapezius is active in the trailing arm during take-way and during the leading arm during acceleration, (2) the levator scapulae and rhomboid muscles are active in the leading arm during the forward swing and acceleration phases and the trailing arm during take-away, and (3) the serratus anterior is constantly active in the leading arm and mainly during the acceleration and early follow-through phase in the trailing arm (Kao, 1995) (Fig. 130.5, 130.6).54 In any technical error in the golf swing, spinal inflexibility or truncal strength deficits could contribute to subsequent injury.
A comprehensive rehabilitative program will focus on all components of flexibility, strength, and endurance conditioning, as well as poor swing biomechanics. Potential areas of inflexibility include limited lumbar spine mobility in any plane, limited hip motion, tight hamstrings, and tight pectoralis muscles. Strengthening exercises should focus on the lumbar paraspinal muscles (erector spinae), abdominal muscles (rectus and oblique), latissimus dorsi, and scapular stabilizers (rhomboid, serratus anterior and trapezius). Finally, a thorough review of all phases of the golf swing is essential to improve any potential technical flaws. Specific areas of focus may include: straightening of the back posture during the swing, proper positioning of the feet to allow equal distribution of weight and appropriate weight transfer during the swing, and speed control during trunk rotation.48
Cycling
Cervical and lumbar spine injuries are quite common in the sport of cycling. The injury will vary for amateur verses professional riders and road verses off-road cycling. In addition, traumatic injuries are more likely to lead to head injuries or spinal fractures, which are beyond the scope of this discussion. For atraumatic injuries, cervical spine injuries include cervical and trapezial muscle strains, while lumbar spine injuries are typically lumbar strains secondary to the various positions of the cyclist. The incidence of low back pain has ranged from 10% to 17% of competitive cyclists.55 Other common injuries include radiculopathies and spondylosis in the older athlete.
The position of the road cyclist for prolonged period of times may predispose the athlete to injury. The cyclist rides with the cervical spine hyperextended and the lumbar spine hyperflexed for aero-dynamic stability. The position may be exaggerated when the cyclist utilizes the drop handlebars or aerobars. Cervical and upper back injuries are probably secondary to the increased load on the arms and shoulders while riding.56 An electromyographic study suggested increased activity in the thoracic muscles depending upon head position and aerodynamic positioning.57 Lumbar spine injuries are probably secondary to an increased stretch to the lumbar paraspinal muscles and increased pressure to the lumbar disc in the hyperflexed position. In addition, lumbar extensor muscle activity appears to be proportional to pedal cadence.57
Rowing
Injury rates among rowers are relatively low when compared to other traumatic sports. However, a fair number of injuries involve the lumbar spine, with an incidence of 15–20% among elite and club level rowers.58,59 Fortunately, the majority of injuries relate to muscle strains from overuse and subsequent fatigue.
Rowers must repetitively cycle though four distinct phases: the finish, recovery, catch, and drive. It has been hypothesized that alterations in flexibility or strength may lead to subsequent injury due to fatigue. A study of 20 elite rowers reveals greater mobility in the lower lumbar spine region and less in the pelvic region in rowers with no history of lower back pain. In contrast, rowers with chronic lower back pain were noted to have hypomobility in the lower spine and compensatory increased motion in the upper lumbar or pelvic regions.60 Over the rowing time period, there was an increase in the lumbar flexion and the electromyographic activity of the lumbar muscle including the multifidus, iliocostalis lumborum. and longissimus muscles.61 In theory, this may lead to subsequent injury.
The rehabilitation of spinal injuries involves a restoration of the spinal mobility and endurance training of the core lumbar muscles. Rowers will benefit from stretching exercises focusing on the hamstring and iliopsoas muscles to increase lumbar flexion and synchronize the lumbopelvic motion.60,61 Strengthening exercises should focus on endurance concentric and eccentric exercises of both the abdominal and lumbar extensor muscles. In addition, exercises should strengthen the gluteal muscles, which assist with developing the explosive forces during the drive phase of rowing. Maintenance of the lumbar flexibility and strength should assist with the prevention of subsequent injuries.
1 Maroon JC, Bailes JE. Athletes with cervical spine injury. Spine. 1996;21(19):2294-2299.
2 Torg JS, Guille JT, Jaffe S. Injuries to the cervical spine in American football players. J Bone Joint Surg [Am]. 2002;84A(1):112-122.
3 Torg JS, Pavlov H, Genuario SE, et al. Neurapraxia of the cervical spinal cord with transient quadriplegia. J Bone Joint Surg [Am]. 1986;68(9):1354-1370.
4 Bailes JE, Herman JM, Quigley MR, et al. Diving injuries of the cervical spine. Surg Neurol. 1990;34(3):155-158.
5 Webb JK, Broughton RB, McSweeney T, et al. Hidden flexion injury of the cervical spine. J Bone Joint Surg [Br]. 1976;58(3):322-327.
6 Marshall SW, Waller AE, Dick RW, et al. An ecologic study of protective equipment and injury in two contact sports. Int J Epidemiol. 2002;31(3):587-592.
7 Maxwell C, Spiegel A. The rehabilitation of athletes after spinal injuries. In: Watkins R, editor. The spine in sports. Philadelphia: Hanley and Belfus; 1990:281-292.
8 Garrick JG, Requa RK. Epidemiology of woman gymnast injuries. Am J Sports Med. 1980;8:260.
9 Tall RL, DeVault W. Spinal injury in sports: Epidemiologic considerations. Clin Sports Med. 1993;12:441-448.
10 Smith J, et al. PASSOR musculoskeletal physical examination core competencies. http://www.aapmr.org/passor/attachmt/msk.pdf, 2003.
11 Beck A, Gebhard F, Kinzl L, et al. Spinal cord injury without radiographic abnormalities in children and adolescents: case report of a severe cervical spine lesion and review of literature. Knee Surg Sports Traumatol Arthrosc. 2000;8(3):186-189.
12 Press JM, Herring S, Kibler WB. Rehabilitation of musculoskeletal disorders. In: Press JM, Herring SA, Kibler WB, editors. The textbook of military medicine. Borden Institute, Office of the Surgeon General, 1998.
13 Laskowski ER. Concepts in sports medicine. In: Braddom RL, Buschbacker RM, Dimitru D, et al, editors. Physical medicine and rehabilitation. Philadelphia: WB Saunders; 2000:957-983.
14 Deyo RA, Diehl AK, Rosenthal M. How many days bed rest for acute low-back pain: a randomized clinical trial. N Engl J Med. 1986;315:1064-1070.
15 Fellander-Tsai L, Micheli LJ. Treatment of spondylolysis with external electrical stimulation and bracing in adolescent athletes: a report of two cases. Clin J Sport Med. 1998;8(3):232-234.
16 Karppinen J, Ohinmaa A, Malmivaara A, et al. Cost effectiveness of periradicular infiltration for sciatica: subgroup analysis of a randomized controlled trial. Spine. 2001;26:2587-2595.
17 Carette S, Leclaire R, Marcoux S, et al. Epidural corticosteroid injections for sciatica due to herniated nucleus pulposus. N Eng J Med. 1997;336:1634-1640.
18 O’Sullivan PB, Phyty GD, Twomey LT, et al. Evaluation of specific stabilizing exercise in the treatment of chronic low back pain with radiologic diagnosis of spondylolysis or spondylolisthesis. Spine. 1997;22(24):2959-2967.
19 Kuukkanen T, Malkia E. Effects of a three-month therapeutic exercise program on flexibility in subjects with low back pain. Physiother Res Int. 2000;5(1):46-61.
20 Sullivan MS, Shoaf LD, Riddle DL. The relationship of lumbar flexion to disability in patients with low back pain. Phys Ther. 2000;80(3):240-250.
21 Magnusson ML, Bishop JB, Hasselquist L, et al. Range of motion and motion patterns in patients with low back pain before and after rehabilitation. Spine. 1998;23(23):2631-2639.
22 Young JL, Press JM, Herring SA. The disc at risk in athletes: perspectives on operative and nonoperative care. Med Sci Sports Med. 1997;29(7):S222-S232.
23 Hodges PW. Core stability exercise in chronic low back pain. Ortho Clin North Amer. 2003;34(2):245-254.
24 Wilke HJ, Wolf S, Claes LE, et al. Stability increase of the lumbar spine with different muscle groups: A biomechanical in vitro study. Spine. 1995;20:192-198.
25 Zhao WP, Kawaguchi Y, Matsui H, et al. Histochemistry and morphology of the multifidus muscle in lumbar disc herniation: comparative study between diseased and normal sides. Spine. 2000;25(17):2191-2199.
26 St. Pierre D, Gardiner PF. The effect of immobilization and exercise on muscle function: a review. Physiother Canada. 1987;39:24-36.
27 Mannion AF. Fiber type characteristics and function of the human paraspinal muscles: normal values and changes in association with low back pain. J Electromyogr Kinesiol. 1999;9(6):363-377.
28 Hides J, Richardson C, Jull G. Multifidus muscle recovery is not automatic after resolution of acute, first-episode low back pain. Spine. 1996;21:2763-2769.
29 Sung P. Multifidi muscles median frequency before and after spinal stabilization exercises. Arch Phys Med Rehabil. 2003;84:1313-1318.
30 Danneels L, Vanderstraten G, Cambier, et al. Effects of three different training modalities on the cross-sectional area of lumbar multifidus in patients with chronic low back pain. Scand J Sports Med. 2001;35:186-191.
31 Wittnick H, Michel TH, Wagner A, et al. Deconditioning in patients with chronic low back pain: fact or fiction? Spine. 2000;25(17):2221-2228.
32 Sulco AD, Paup DC, Fernhall B, et al. Effects of aerobic exercise on low back pain patients in treatment. Spine J. 2001;1(2):95-101.
33 Ahern DK, Lohr BA. Psychosocial factors in sports injury rehabilitation. Clin Sports Med. 1997;16(4):755-768.
34 Gatchel RJ, Polatin PB, Mayer TG. The dominant role of psychosocial risk factors in the development of chronic low back pain disability. Spine. 1995;20(24):2702-2709.
35 Croft PR, Papageorgiou AC, Ferry S, et al. Psychologic distress and low back pain. Evidence from a prospective study in the general population. Spine. 1995;20(24):2731-2737.
36 Verbunt JA, Seelen HA, Vlaeyen JW, et al. Disuse and deconditioning in chronic low back pain: concepts and hypotheses on contributing mechanisms. Eur J Pain. 2003;7(1):9-21.
37 Wang WT, Olson SL, Campbell AH, et al. Effectiveness of physical therapy for patients with neck pain: an individualized approach using a clinical decision-making algorithm. Am J Phys Med Rehabil. 2003;82(3):203-218.
38 Beazell JR, Magrum EM. Rehabilitation of head and neck injuries in the athlete. Clin Sports Med. 2003;22(3):523-557.
39 Torg JS, Ramsey-Emrhein JA. Management guidelines for participation in collision activities with congenital, developmental, or postinjury lesions involving the cervical spine. Clin J Sport Med. 1997;7(4):273-291.
40 Cantu RC. Functional cervical spinal stenosis: a contraindication to participation in contact sports. Med Sci Sports Exerc. 1993;25(3):316-317.
41 Standaert CJ, Herring SA, Halperin B, et al. Spondylolysis. Phys Med Rehab Clinic North Amer. 2000;11(4):785-803.
42 Congeni J, McCulloch J, Swanson K. Lumbar spondylolysis. A study of natural progression in athletes. Am J Sports Med. 1997;25(2):248-253.
43 Micheli LJ, Hall JE, Miller ME. Use of modified Boston brace for back injuries in athletes. Am J Sports Med. 1980;8(5):351-356.
44 Blanda J, Bethem D, Moats W, et al. Defects of pars interarticularis in athletes: a protocol for nonoperative treatment. J Spinal Disord. 1993;6(5):406-411.
45 Gatt CJ. Back pain in running. In: Guten G, editor. Running injuries. Philadelphia: WB Saunders; 1997:47-60.
46 Schache AG, Blanch P, Rath D, et al. Three-dimensional angular kinematics of the lumbar spine and pelvis during running. Human Movement Sci. 2002;21:273-293.
47 Capozzo A. Force actions in the human trunk during running. J Sports Med. 1983;23:14-22.
48 Theriault G, Lachance P. Golf injuries: An overview. Sports Med. 1998;26(1):43-57.
49 Theriault G, Lacoste E, Gaboury M, et al. Golf injury characteristics: a survey from 528 golfers. Med Sci Sports Exerc. 1996;28(5):565-571.
50 McCarroll JR. The frequency of golf injuries. Clin Sports Med. 1996;15:1-7.
51 Hosea TM, Gatt CLJr. Back pain in golf. Clin Sports Med. 1996;15:37-53.
52 Pink M, Perry J, Jobe FW. Electromyographic analysis of the trunk in golfers. Am J Sports Med. 1993;21(3):385-388.
53 Watkins RG, Uppal GS, Perry J, et al. Dynamic electromyographic analysis of trunk musculature in professional golfers. Am J Sports Med. 1996;24(4):535-538.
54 Kao JY, Pink M, Jobe FW, et al. Electromyographic analysis of the scapular muscles during a golf swing. Am J Sports Med. 1995;23(1):19-23.
55 Burke ER. Cycling. In: Watkins RG, editor. The spine and sports. St Louis: Mosby; 1996:592-596.
56 Mellion MB. Common cycling injuries: Manag Prevent Sports Med. 1991;11(1):52-70.
57 Usabiaga J, Crespo R, Iza I, et al. Adaptation of the lumbar spine to different positions in bicycling racing. Spine. 1997;22(17):1965-1969.
58 Hickey GJ, Fricker PA, McDonald WA. Injuries to elite rowers over a ten year period. Med Sci Sports Exer. 1997;29:1567-1572.
59 Bahr R, Anderson SO, Loken S, et al. Low back pain among endurance athletes with and without specific back loading: a cross-sectional survey of cross-country skiers, rowers and orienteerers and nonathletic controls. Spine. 2004;29(4):449-454.
60 MacGregor A, Anderson L, Gedroyc W. The assessment of interspinal motion and pelvic tilt in elite oarsmen. Med Sci Sports Exerc. 2002;34(7):1143-1149.
61 Caldwell J, McNair PJ, Williams M. The effects of repetitive motion on lumbar flexion and erector spinae muscle activity in rowers. Clincal Biomechanics. 2003;18:704-711.