Retropubic Urethropexy for Stress Incontinence
Modified Burch Colposuspension
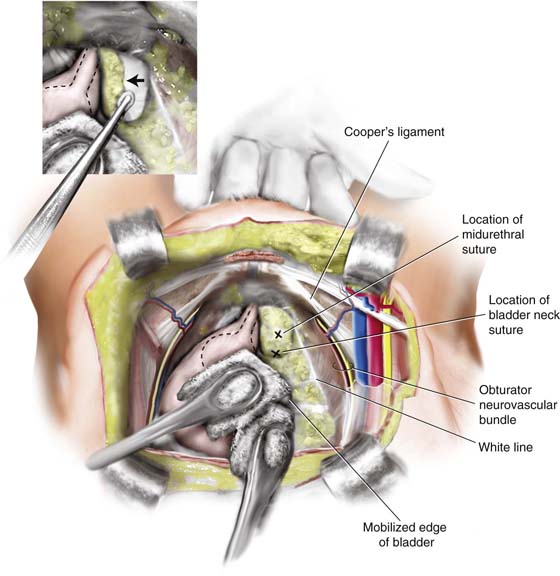
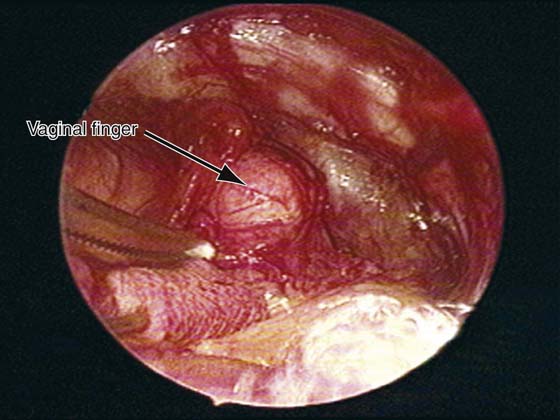
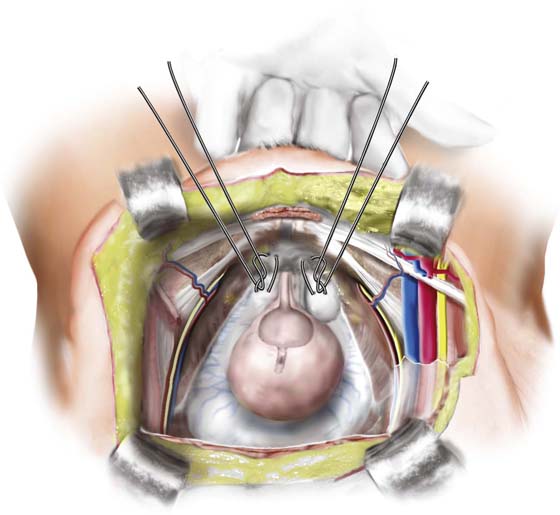
After the retropubic space is entered, the urethra and anterior vaginal wall are depressed. Dissection at the midline is avoided, thus protecting the delicate musculature of the urethra and urethrovesical junction from surgical trauma. Attention is directed to the tissue on either side of the urethra. The surgeon’s nondominant hand is placed in the vagina with the index and middle fingers on one side of the proximal urethra. Two sponge sticks are utilized to gently mobilize the bladder to the opposite side (Figs. 33–1 through 33–3). Most of the overlying fat can be cleared away with the use of a swab mounted on a curved forceps. This dissection is accomplished with forceful elevation of the surgeon’s vaginal finger until glistening, white periurethral fascia and vaginal wall are seen (see Figs. 33–1, 33–4, and 33–5). This area is extremely vascular, with a rich, thin-walled venous plexus, and should be avoided if possible. The positions of the urethra and the lower edge of the bladder are determined by palpating the Foley balloon, or by partially distending the bladder if necessary to find the rounded lower margins of the bladder as it meets the anterior vaginal wall.
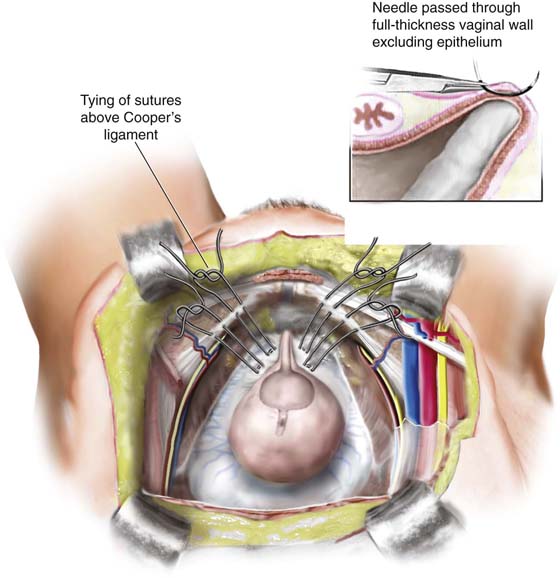
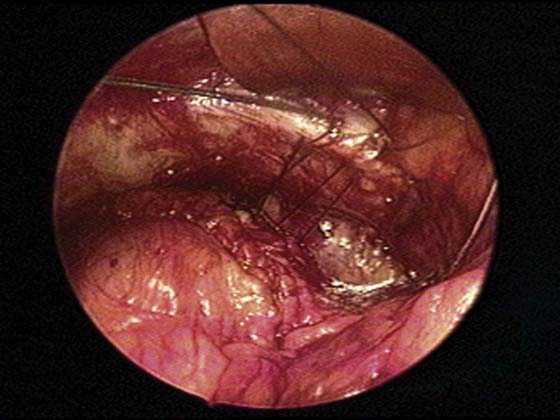
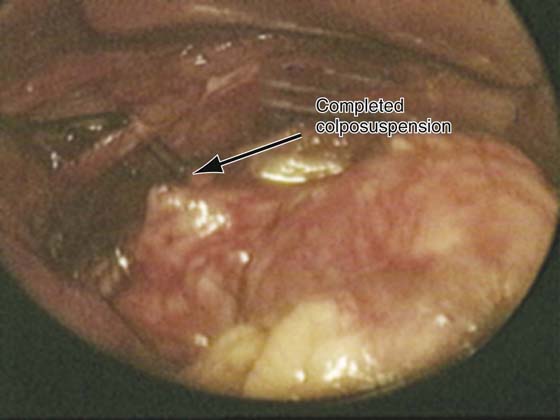
Dissection lateral to the urethra is completed bilaterally, and vaginal mobility is judged to be adequate by using the vaginal finger to lift the anterior vaginal wall upward and forward (see Figs. 33–1 and 33–5). Either 0 or 1 delayed-absorbable or nonabsorbable sutures are then placed lateral in the anterior vaginal wall. We apply two sutures of graded polyester on an SH needle (Ethibond by Ethicon, Inc., Somerville, NJ) bilaterally, using double bites for each suture. These sutures are double-armed so that each end of the suture can subsequently be brought up through Cooper’s ligament (see Figs. 33–4, 33–6, and 33–7). Proper placement of these sutures is important to provide adequate support and to avoid undue urethral kinking or elevation leading to postoperative voiding dysfunction or retention. We prefer to place the sutures in the lateral portion of the vagina just lateral to the tip of the vaginal finger, which should be elevating the most mobile and pliable portion of the vagina lateral to the bladder neck (see Figs. 33–1 through 33–8). The distal suture is placed 2 cm lateral to the proximal third of the urethra, and the proximal suture is placed approximately 2 cm lateral to the bladder wall or slightly proximal to the level of the urethrovesical junction (see Figs. 33–4 and 33–7). In placing the sutures, one should take a full-thickness bite of the vaginal wall, excluding the epithelium. This maneuver is accomplished by suturing over the surgeon’s vaginal finger at appropriate selected sites (see Figs. 33–4 and 33–5). On each side after the two sutures are placed, they are passed through the pectineal or Cooper’s ligament, so that all four suture ends exit above the ligament (see Figs. 33–4 and 33–7). The retropubic space can be extremely vascular, and visible vessels should be avoided if possible. When excessive bleeding occurs, it can be controlled by direct pressure, sutures, or vascular clips. Severe bleeding usually stops with direct pressure, or after the fixation sutures are tied. After all four sutures are placed in the vagina and through Cooper’s ligament, the assistant ties first the distal sutures and then the proximal ones while the surgeon elevates the vagina with the vaginal hand (see Fig. 33–8). If desired, a suprapubic catheter is placed through the extraperitoneal portion of the dome of the bladder. In tying the sutures, one does not have to be concerned about whether the vaginal wall meets Cooper’s ligament.
Marshall-Marchetti-Krantz Procedure
The retropubic space is exposed as previously described. Again, the surgeon’s nondominant hand is placed in the vagina, and dissection of the periurethral fat is performed as previously described for the Burch colposuspension. Some surgeons routinely perform a cystotomy to aid in periurethral dissection and suture placement.
Delayed-absorbable or permanent sutures are used and are placed at right angles to the urethra and parallel to the vesical neck. A single suture is placed bilaterally at the urethrovesical junction. A double bite is taken over the surgeon’s finger, incorporating the full thickness of the vaginal wall and excluding the epithelium. After placement of the sutures, the point of fixation of the urethra to the symphysis pubis can be determined by elevating the two vaginal fingers to the point where the vesical neck comes in contact with the pubic symphysis and noting the position at which the sutures will be placed into the pubic periosteum. The needle is placed medially to laterally against the periosteum and is turned with a simple wrist action. This may involve the cartilage in the midline, depending on the width, thickness, and availability of the periosteum. The sutures on each side are placed accordingly and are tied with the vaginal finger elevating the urethrovesical junction (Fig. 33–9).
FIGURE 33–1 Burch colposuspension. The bladder is gently mobilized to the opposite side with sponge sticks. The anterior vaginal wall is elevated by the middle finger of the surgeon’s nondominant hand, and fat is mobilized medially (see inset) with a swab mounted on a curved forceps or suction tip. The position of the sutures (indicated with an X) ideally should be at least 2 cm lateral to the proximal urethra and bladder neck, usually on the lateral downslope of the tissue elevated by the vaginal finger.
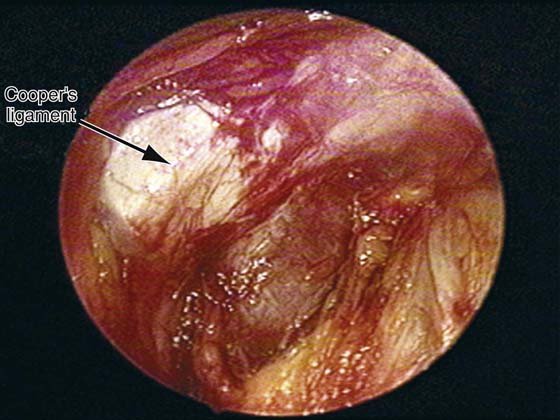
FIGURE 33–2 Lateral view of the retropubic space in a live patient. Note: The tissue has been cleaned off over Cooper’s ligament on the left side. This is the area through which the suspension sutures will be passed during performance of a Burch colposuspension.
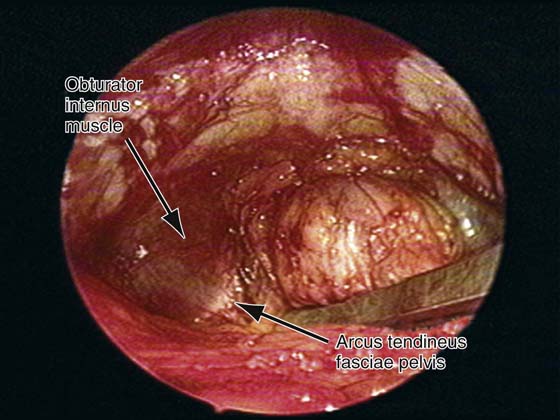
FIGURE 33–3 The lateral retropubic space on the left side is shown. Note the obturator internus muscle, which inserts into the arcus tendineus fasciae pelvis.
FIGURE 33–4 Sutures have been appropriately placed on each side of the proximal urethral and bladder neck. Note that figure-of-8 bites are taken through the vagina. Double-armed sutures are used so that the end of each suture can be brought up through the ipsilateral Cooper’s ligament, thus allowing the sutures to be tied above the ligament.
FIGURE 33–5 The first step of the Burch colposuspension is to elevate the vagina and mobilize the fat in a medial direction. Note: A sponge stick is used to initially mobilize the bladder medially, and then the fat is cleaned off with a small Kitner-type instrument. Elevating the vagina reveals the muscular lining of the vaginal wall through which sutures will be passed lateral to the midurethra and lateral to the bladder neck.
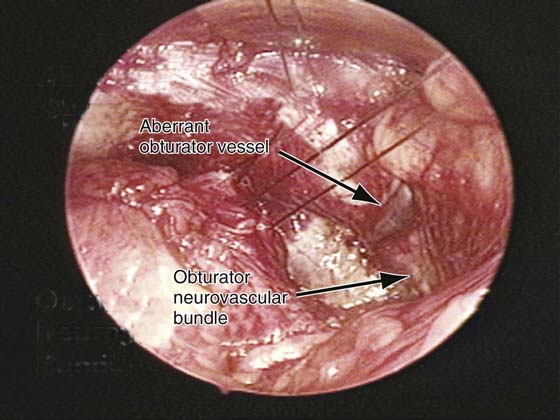
FIGURE 33–6 Two Burch colposuspension sutures have been passed through the full thickness of the vaginal wall on the patient’s right side. The suture lateral to the midurethra has also been passed through Cooper’s ligament on that side. Noted in this picture is an aberrant obturator vessel draping down over the most lateral aspect of Cooper’s ligament. Also noted is the obturator neurovascular bundle as it exits the pelvis through the obturator canal.
FIGURE 33–7 Both Burch colposuspension sutures have been passed on the right side. Again note that each end of the suture has been brought up through Cooper’s ligament and the knots tied above the ligament, completing the colposuspension on the right side.
FIGURE 33–8 The completed colposuspension is shown on the patient’s left side. Again note that the knot is tied above Cooper’s ligament, and sutures are elevated just until the slack or tension is taken out of the suture. It is very common to see, as in this photograph, a suture bridge that exists between the elevated vagina and Cooper’s ligament.
FIGURE 33–9 Marshall-Marchetti-Krantz procedure. One suture is placed bilaterally at the level of the bladder neck and then into the periosteum of the pubic symphysis.