Retropubic Paravaginal Repair
Anterior vaginal wall prolapse may be the result of detachment of the vagina from its normal lateral attachment. The object of the paravaginal defect repair is to reattach bilaterally the anterior lateral vaginal sulcus with its overlying fascia to the lateral sidewall at the level of the arcus tendineus fasciae pelvis, which is its normal attachment.
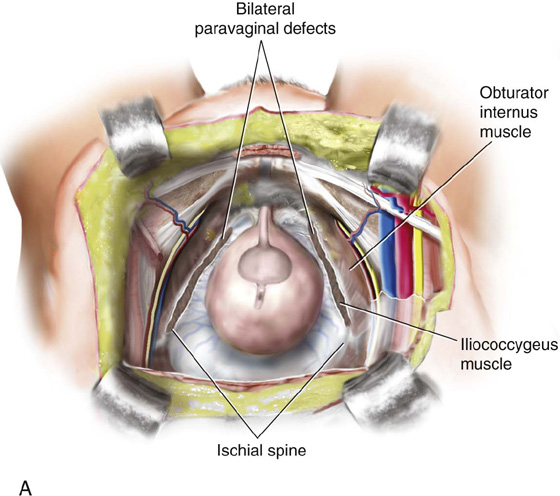
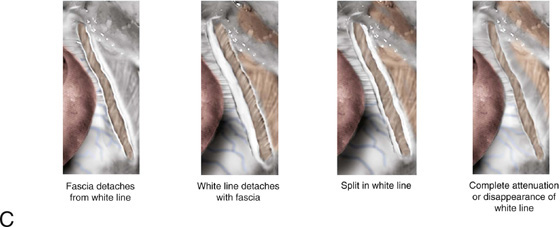
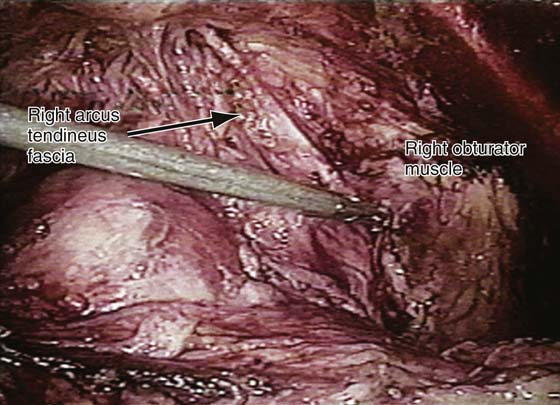
The retropubic space is entered, and the bladder and vagina are depressed and retracted medially to allow visualization of the lateral retropubic space and the lateral pelvic sidewall, including the obturator internus muscle and the fossa containing the obturator neurovascular bundle (Figs. 34–1 through 34–3; also see Chapter 31 on Retropubic Anatomy). Blunt dissection can be carried dorsally from this point until the ischial spine is palpated. The arcus tendineus fasciae pelvis, or white line, is often visualized as a white band of tissue running from the back of the symphysis pubis to the ischial spine (see Figs. 34–2 and 34–3). It is the anatomic separation between the lower edge of the obturator internus muscle and the beginning of the iliococcygeal portion of the levator ani muscle. A paravaginal defect represents avulsion of the vagina with its muscular layer or pubocervical fascia off the arcus tendineus fasciae pelvis or possibly an avulsion of the arcus as well as the fascia off the obturator internus muscle (see Figs. 34–1 through 34–3). Figure 34–1C depicts various anatomic defects that can be encountered when a paravaginal defect is present. It should be noted that at times the white line can be so attenuated that it may not be anatomically identifiable.
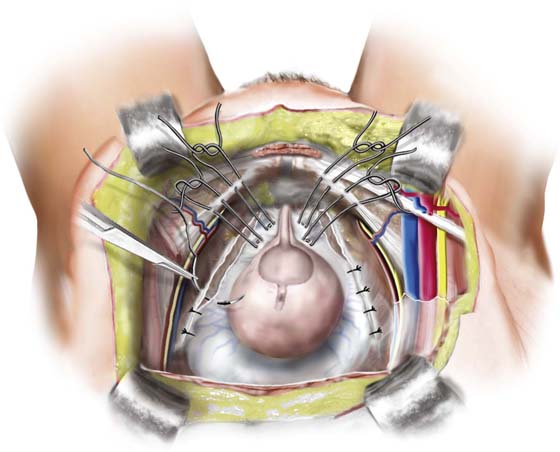
A retropubic paravaginal defect repair is performed as follows: The surgeon’s nondominant hand is inserted into the vagina. While gently retracting the bladder medially with sponge sticks (as shown in Fig. 33–1 in Chapter 33), the surgeon elevates the anterior lateral vaginal sulcus. Starting near the vaginal apex, a suture is placed first through the full thickness of the vagina excluding the epithelium. This suture should be in the lateral edge of the underlying muscular tissue of the vagina, or the pubocervical fascia. The needle then is passed into the obturator internus fascia or, if visualized, the arcus tendineus fasciae pelvis, 1 to 2 cm anterior to its origin at the ischial spine. After this first stitch is tied, four or five additional sutures are placed through the vaginal wall and then into the arcus tendineus fasciae pelvis or obturator internus fascia (see Fig. 34–1B). These stitches are placed at 1-cm intervals toward the pubic ramus. Tying of the sutures reapproximates the vagina with its fascia to the lateral pelvic sidewall (Figs. 34–1, 34–4, and 34–5). The most distal suture should be placed as close as possible to the pubic ramus into the pubourethral ligament. Usually 2-0 or 3-0 nonabsorbable sutures on a medium-sized tapered needle are utilized for this repair.
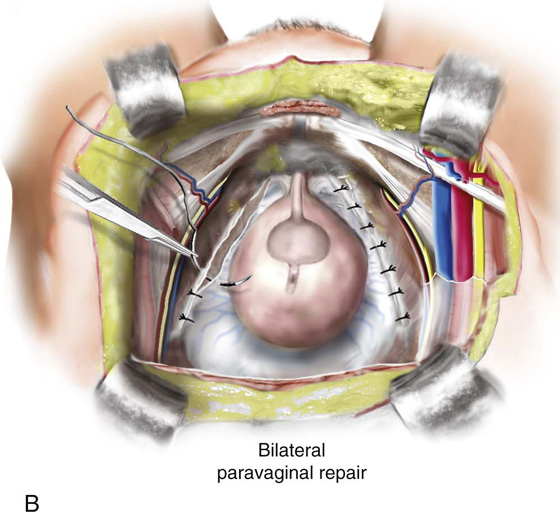
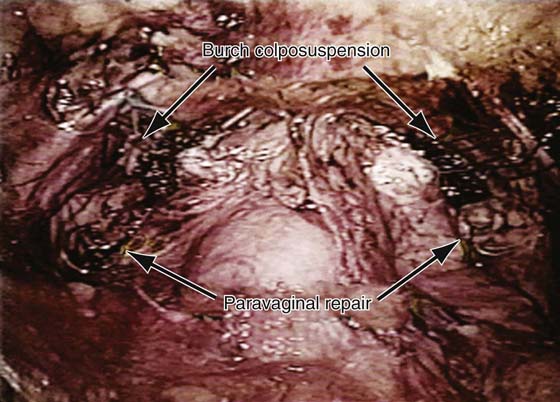
In patients who have genuine stress incontinence plus a paravaginal defect, a combined Burch colposuspension and retropubic paravaginal repair should be performed. This has been termed a paravaginal plus procedure (see Figs. 34–4 and 34–5).
FIGURE 34–1 Retropubic paravaginal defect repair. A. Bilateral paravaginal defects are illustrated. B. The defect on the right has been completely repaired, and the defect on the left is being repaired from just distal to the ischial spine and working toward the pubic symphysis. C. Four potential anatomic findings in patients with paravaginal defects are illustrated. Note that all result in falling away of the vagina with its underlying fasciae from the lateral pelvic sidewall.
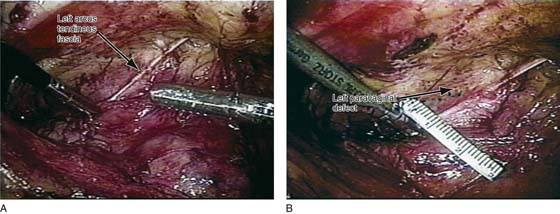
FIGURE 34–2 Demonstrates a patient with a left paravaginal defect repair. A. Note that the arcus tendineus fasciae pelvis has been detached. B. A 2-cm paravaginal defect is noted.
FIGURE 34–3 Demonstrates a right paravaginal defect on the same patient as in Figure 34–2. Again note the detached arcus tendineus fasciae pelvis.
FIGURE 34–4 Paravaginal defect plus repair. Combined Burch colposuspension and retropubic paravaginal defect repair.
FIGURE 34–5 Completed paravaginal prep plus procedure. Note that the Burch colposuspension stitches have been placed to pass to Cooper’s ligament, and the paravaginal stitches have reattached the detached arcus to the obturator internus fascia.