Retroperitoneal Sarcoma
Preoperative Imaging and Incision
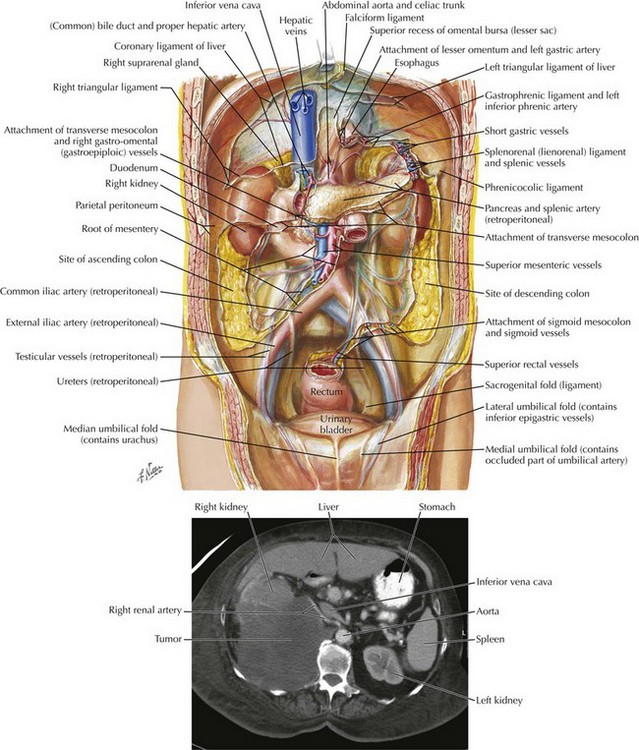
The retroperitoneum has many vital structures, including the kidneys, pancreas, inferior vena cava (IVC), and the aorta (Fig. 50-1). These structures are close to each other and can become greatly distorted by a large retroperitoneal tumor. Preoperative imaging is particularly useful; the CT scan in Figure 50-1 shows a large, right retroperitoneal tumor. This tumor encroaches on the IVC and clearly involves the right kidney. Availability of this information before surgery can allow for preoperative assessment of kidney function in the event of nephrectomy and planning for possible vascular resection (consulting with vascular surgeon).
Abdominal Exposure for Tumor Removal
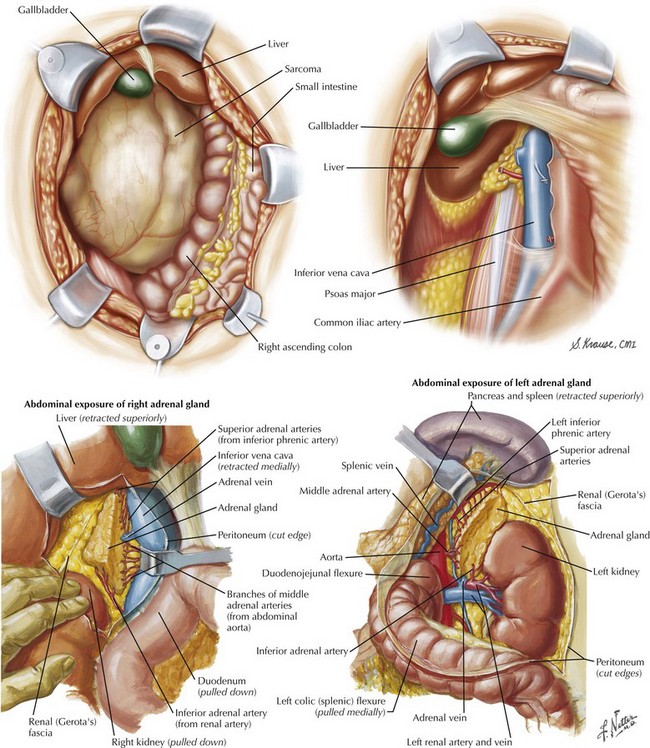
After the surgeon enters the abdomen, the retroperitoneal tumor is often the first structure to be seen and distorts the normal anatomy; a common site is shown in Figure 50-2. It is in these situations that correctly recognizing structures and being in the correct plane are vital.
Figure 50-2 shows the right retroperitoneum after removal of a large retroperitoneal tumor. Notice that the right kidney was resected as well. In this case the right colon and the duodenum have been mobilized and retracted medially.
Anaya, DA, Lev, DC, Pollock, RE. The role of surgical margin status in retroperitoneal sarcoma. J Surg Oncol. 2008;98(8):607–610.
Hueman, MT, Herman, JM, Ahuja, N. Management of retroperitoneal sarcomas. Surg Clin North Am. 2008;88(3):583–597.
Raut, CP, Pisters, PW. Retroperitoneal sarcomas: combined-modality treatment approaches. J Surg Oncol. 2006;94(1):81–87.
Thomas, DM, O’Sullivan, B, Gronchi, A. Current concepts and future perspectives in retroperitoneal soft-tissue sarcoma management. Expert Rev Anticancer Ther. 2009;9(8):1145–1157.