205 Retinal vein thrombosis
Salient features
History
• Age: central retinal vein occlusions arise in 0·1–0·4% and branch retinal vein occlusions in 0·6–1·1% of adults aged ≥40 years
• Branched retinal vein occlusion: decreased vision, floaters suggest vitreal haemorrhage
• Central retinal vein occlusion: loss or decreased vision, headache (associated increase in intraocular pressure), floaters
• History of hypertension, diabetes, glaucoma, multiple myeloma or macroglobulinaemia.
Examination
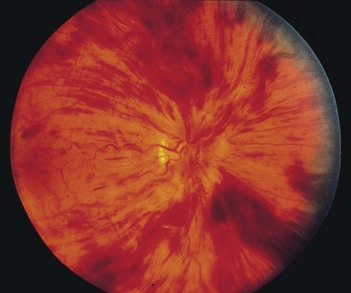
Patient 1
Central retinal vein occlusion (Fig. 205.1), the occlusion is behind the cribriform plate:
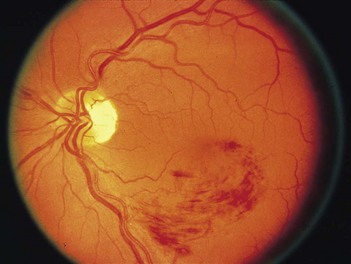
Patient 2
• Branch vein occlusion (Fig. 205.2), the occlusion is in front of the cribriform plate:
Advanced-level questions
What is the clinical course in central retinal vein occlusion?
• In mild cases, there is minimal dilatation of veins and haemorrhages with little or no oedema of the macula and no visual deficit.
• In severe instances, the vision may deteriorate to hand motions, with extensively deep and superficial haemorrhages with stagnation of blood in the markedly dilated veins and several cottonwool spots.
How would you manage such eyes?
• Treat the underlying condition
• Fluorescein angiography to determine areas of retinal ischaemia
• Regular follow-up by the ophthalmologist as secondary neovascularization is a common sequel and may need laser therapy. Panretinal photocoagulation prevents the dreaded complications of neovascular glaucoma.