Retinal Detachment
Introduction:
Some eyes may present with a combination of these three. Tractional and exudative detachments are dealt in greater detail in the chapters associated with their underlying pathologies. Rhegmatogenous RD are more common in men, particularly those between 40 and 70 years of age. Risk factors for rhegmatogenous RD include prior cataract surgery, myopia, trauma, peripheral lattice degeneration, a family history of rhegmatogenous RDs, retinal tears and other intraocular surgery. Tractional RDs occur most commonly in the setting of fibrous membranes in the vitreous, secondary to diseases like proliferative diabetic retinopathy, retinopathy of prematurity, sickle cell retinopathy, trauma or proliferative vitreoretinopathy. Exudative RDs occur secondary to neoplastic or inflammatory processes, central serous chorioretinopathy, or uveal effusion syndrome
Clinical features:
Patients with rhegmatogenous RD present with painless unilateral decrease in vision or visual field with flashes and floaters. Most eyes have a posterior vitreous detachment. Examination reveals elevation of the retina, with a corrugated appearance and generally clear subretinal fluid that does not shift with position. The pathognomonic sign of a rhegmatogenous RD is the presence of one or more retinal tears or full thickness holes (Fig. 24.1.1).
OCT Features:
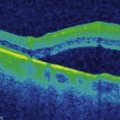
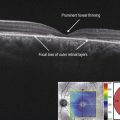
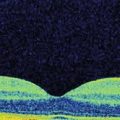
OCT of RD shows elevation of the neurosensory retina from the underlying RPE (Figs 24.1.2 and 24.1.3). No splitting of retinal layers is seen except in the setting of combined retinoschisis-rhegmatogenous RD. Occasionally, RDs especially chronic RDs may be associated with cystic changes within the retina. The subretinal fluid in rhegmatogenous RDs is usually clear and hyporeflective.

Figure 24.1.2 OCT scan through a retinal detachment shows separation of the neurosensory retina from the hyper-reflective underlying RPE. There is SRF seen. Note the site of vitreous attachment on the retina.
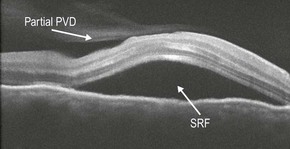
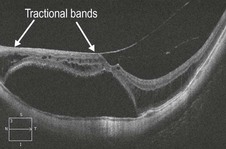
Figure 24.1.3 OCT scan through a serous retinal detachment on the left and a tractional detachment on the right. Note the smooth surface of the serous detachment and the preretinal fibrous tractional bands and hyaloidal thickening in the tractional retinal detachment.
Serous RDs may occasionally be associated with turbid subretinal fluid that is hyper-reflective.