1 Resuscitation
Clinical Presentation
The signs and symptoms of children requiring immediate resuscitation are typically the result of failure of the delivery of two vital substrates—oxygen and glucose—to end organs (Table 1-1). Recognition of these manifestations through a physical examination that focuses on airway, gas exchange, and cardiovascular stability allows for rapid resuscitation of those who have failure of substrate delivery and identification of those at risk for failure.
| Airway | Complete or severe airway obstruction |
| Breathing | Apnea, significant work of breathing, bradypnea |
| Circulation | Absence of detectable pulses, poor perfusion, hypotension, bradycardia |
| Disability | Unresponsiveness, depressed consciousness |
| Exposure | Significant hypothermia, significant bleeding, petechiae or purpura consistent with septic shock, abdominal distension consistent with acute abdomen |
Adapted from American Academy of Pediatrics and American Heart Association: Pediatric Advanced Life Support. Dallas, TX, American Heart Association Publication, 2006.
Initial Assessment
Primary Assessement
Airway
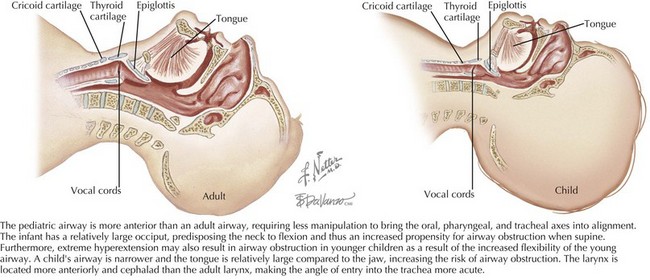
The patient’s airway is the first priority. There are fundamental differences between the airway of a child and that of an adult. The pediatric airway (Figure 1-1) is more anterior than the adult airway, requiring less manipulation to bring the oral, pharyngeal, and tracheal axes into alignment. In addition, the head-to-body proportion is larger in infants than in adults, and thus extreme hyperextension of the neck may exacerbate airway obstruction in younger children. The pediatric airway is narrower, and the tongue is relatively large compared with the jaw, increasing the risk of airway obstruction. The pediatric larynx is located more anteriorly and cephalad than the adult larynx.
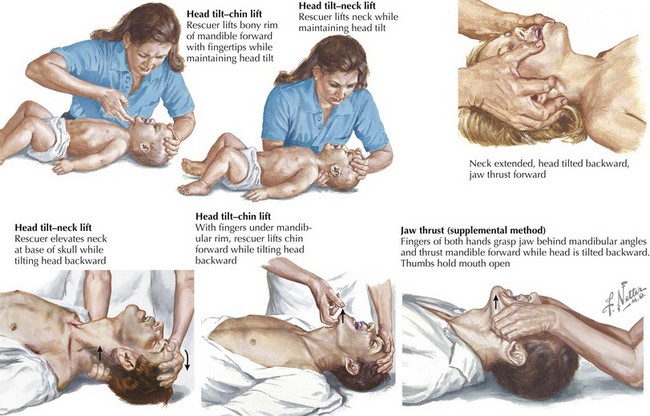
The most effective maneuvers for opening an obstructed pediatric airway are the head tilt–chin lift or jaw thrust techniques (Figure 1-2). In the head tilt–chin lift maneuver, the head is tilted back slightly (without overextending), and the chin is lifted gently with one finger on the bony prominence to avoid placing pressure on the soft tissues of the neck. A roll or towel may be placed under the shoulders to maintain the position.
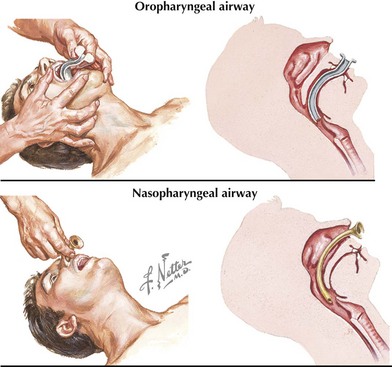
In an unconscious patient, an oropharyngeal airway can be used to help stent the mandibular block of tissue away from the posterior hypopharynx (Figure 1-3). A nasopharyngeal (NP) airway is another option. NP airways are well tolerated in unconscious and semiconscious patients and may even be used in conscious individuals with upper airway obstruction. NP airways should be used with caution when midface trauma is suspected because of the risk of inserting the airway through fractured bone into intracranial structures. Laryngeal mask airways (LMAs) are supraglottic airway devices that are being increasingly used in resuscitation settings to help bypass the soft tissues of the anterior oropharynx and to deliver oxygen directly to the proximal trachea.
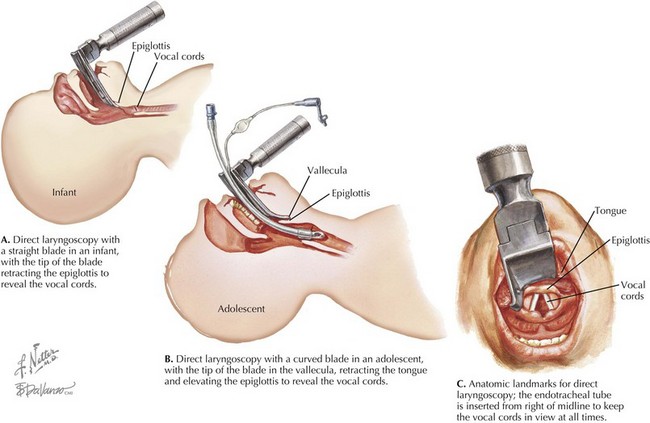
Direct laryngoscopy can be accomplished by positioning the patient’s head and then using the right thumb and index finger to “scissor” open the mouth. The laryngoscope blade is inserted under direct vision toward the right corner of the mouth over the tongue and over the epiglottis (if using a straight blade) or into the vallecula (if using a curved blade). The tongue should be “swept” toward the left side the mouth while the laryngoscope handle is pulled upward at a 45-degree angle, taking care not to damage the teeth or gums (Figure 1-4). Suctioning may be needed to clear secretions to visualize the vocal cords, which should fall into the direct line of sight. The provider should maintain his or her view of the larynx and insert the ETT while watching it pass through the vocal cords. The tube should be placed so that the second of the distal vocal cord markers is at the level of the vocal cords. A projection for how deep to place the tube (centimeter mark at the teeth) can be calculated using the following formulas: [(Age in years/2) + 12] or [3 × (External diameter of the ETT)].
Breathing
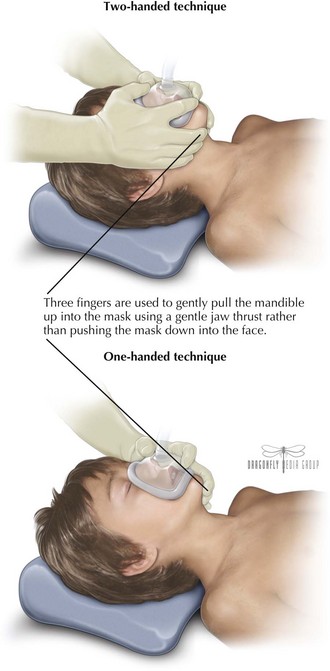
If the patient’s efforts at ventilation or oxygenation are compromised, assisted ventilation should be initiated. BVM ventilation (Figure 1-5) is a skill at which all physicians working in acute-care settings should become adept. Masks of various sizes should be available, and the smallest mask that completely covers the mouth and nose should be selected. Airway patency is maximized when the patient’s head is placed in the “sniffing position,” with the neck slightly flexed while the head is rotated into extension.
Circulation
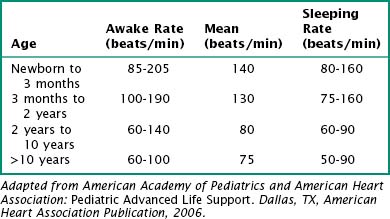
Heart rate should be appropriate for the child’s age (Table 1-2) but may be affected by clinical conditions other than poor circulation (e.g., fever, dehydration, pain). Normal blood pressure is also age dependent (Table 1-3) and can also be affected by associated clinical conditions. In children, compensatory mechanisms (tachycardia, increased stroke volume, and vasoconstriction) may cause blood pressure to be preserved even though there is inadequate tissue perfusion. This is termed compensated shock (see Chapter 2). However, hypotension should be treated as shock until proven otherwise in critically ill or injured children because it represents a state in which compensatory mechanisms have failed (uncompensated shock). It is important to measure blood pressure using a properly sized cuff.
Table 1-3 Definition of Hypotension by Systolic Blood Pressure and Age
| Age | Systolic Blood Pressure (mm Hg) |
|---|---|
| Term neonates (0-28 days) | <60 |
| Infants (1-12 months) | <70 |
| Children (1-10 years) | <70 + (Age in years × 2) |
| Children (>10 years) | <90 |
BP, blood pressure
Adapted from American Academy of Pediatrics and American Heart Association: Pediatric Advanced Life Support. Dallas, TX, American Heart Association Publication, 2006.
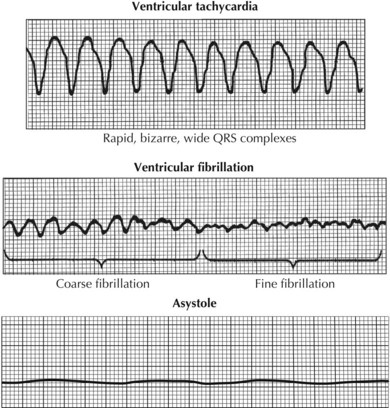
Cardiac arrest is associated with the following arrest rhythms (Figure 1-6): asystole, PEA, VF, and pulseless VT. Asystole is characterized by the absence of discernible electrical activity (“flatline”). PEA is a condition in which the patient has no palpable pulse despite showing electrical activity on cardiac monitoring (but excludes VF, VT, and asystole). VT is characterized by organized, wide QRS (>0.08 sec) complexes. Pulseless VT must be distinguished from VT with a pulse because they are treated differently. VF is a form of pulseless arrest that is characterized by chaotic, disorganized electrical activity on cardiac monitoring with an absence of coordinated contractions. For all of these rhythms, it is important to provide supplemental oxygen (100%) and to initiate CPR immediately.
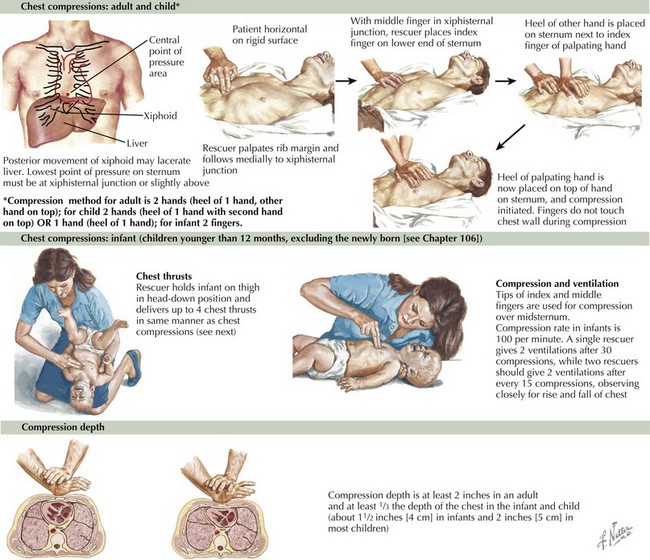
CPR (Figure 1-7) is indicated for the management of cardiopulmonary arrest. Studies have consistently shown that CPR, when performed correctly, saves lives. The mantra “push hard, push fast, minimize interruptions, allow full chest recoil, and do not overventilate” should guide the provider’s efforts.
Recommendations for compression to breath ratios are summarized. In newborns, a ratio of 3 : 1 is recommended. In infants and children, the compression to ventilation ratio is different depending on whether there is a single rescuer or two rescuers performing CPR. A single rescuer should give 30 compressions for every 2 breaths, whereas 2 rescuers should perform CPR using the ratio of 15 compressions for every 2 breaths. In both scenarios, the goal is to provide at least 100 compressions per minute. After an artificial airway has been placed, continuous compressions at a rate of at least 100 compressions/min with ventilations at a rate of about 8 to 10 breaths/min (1 breath every 6-8 sec) should be performed. Resuscitation of the newly born infant is discussed in Chapter 106.
Disability
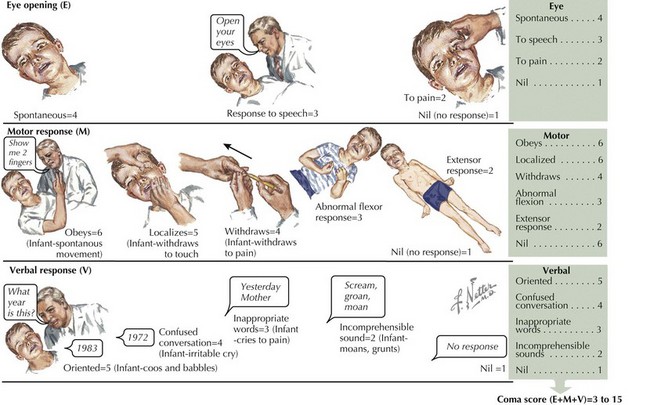
A more detailed assessment for older children and adolescents, the Glasgow Coma Scale, is the most widely used method (Figure 1-8). The patient’s best responses in each of the categories (eye opening, verbal response, motor response) are added to produce a score out of 15. A change of 2 points reflects a clinically significant change in neurologic status. This scale is modified when used in infants and younger children.
American Academy of Pediatrics and American Heart Association. Pediatric Advanced Life Support. Dallas, TX: American Heart Association Publication; 2006.
Atkins DL, Everson-Stewart S, Sears GK, et al. Resuscitation Outcomes Consortium Investigators. Epidemiology and outcomes from out-of-hospital cardiac arrest in children: The Resuscitation Outcomes Consortium Epistry-Cardiac Arrest. Circulation. 2009;119(11):1484-1491.
Berg MD, Schexnayder SM, Chameides L, et al. Pediatric Basic Life Support: 2010 American Heart Association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care: part 13. Circulation. 2010;122:S862-S875.
King C. Cardiopulmonary life support procedures. editor. Henretig FM, King C, editors. Textbook of Pediatric Emergency Procedures. Philadelphia: Lippincott Williams & Wilkins, 1997.
Kleinman ME, Chameides L, Schexnayder SM, et al. Pediatric Advanced Life Support: 2010 American Heart Association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care: part 14. Circulation. 2010;122:S876-S908.
Ludwig SL, Lavelle JM. Resuscitation—pediatric basic and advanced life support. In Fleisher G, Ludwig S, Henretig FM, editors: Pediatric Emergency Medicine, ed 5, Philadelphia: Lippincott Williams & Wilkins, 2006.
Schexnayder SM, Zaritsky AL. Pediatric Resuscitation. editors. Pediatr Clin North Am. 2008;55(4).
Topjian AA, Berg RA, Nadkarni VM. Pediatric cardiopulmonary resuscitation: advances in science, techniques, and outcomes. Pediatrics. 2008;122(5):1086-1098.