CHAPTER 32 Results and Complications
Reports on the results of reverse shoulder arthroplasty are becoming more common as implantation of this type of shoulder arthroplasty increases. The results vary predominantly by the underlying indication for which the arthroplasty was performed. We have participated in a large European-based study of the reverse prosthesis and continually enroll patients in our own database.1 The results and complications presented in this chapter are drawn from these sources.
RESULTS
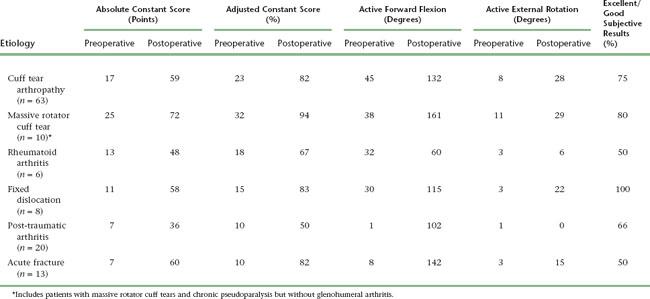
The results of reverse shoulder arthroplasty vary mainly with the etiology for which the arthroplasty was performed. The best results are obtained in the treatment of osteoarthritis with a massive rotator cuff tear (rotator cuff tear arthropathy), whereas results are least satisfactory in patients with post-traumatic arthritis. Tables 32-1 and 32-2 detail the results of reverse shoulder arthroplasty for the most common indications for which it is performed. These tables express the results in terms of active mobility; patient satisfaction; the Constant score, a shoulder-specific outcomes device incorporating pain, mobility, activity, and strength; and the age- and gender-adjusted Constant score.2,3
Table 32-1 RESULTS OF REVERSE SHOULDER ARTHROPLASTY ACCORDING TO UNDERLYING ETIOLOGY IN A LARGE EUROPEAN-BASED STUDY
| Rights were not granted to include this data in electronic media. Please refer to the printed book. |
INTRAOPERATIVE COMPLICATIONS
Humerus
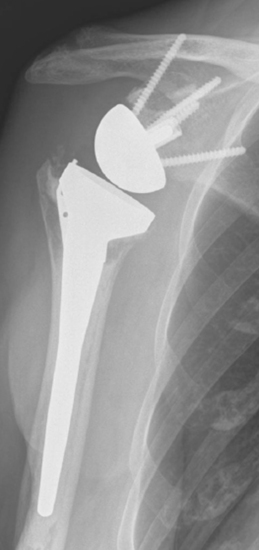
The most common humeral complication is iatrogenic fracture, which usually results from performing an overly aggressive dislocation maneuver without previous adequate soft tissue release. Many patients undergoing reverse shoulder arthroplasty have moderate to severe osteopenia, thus placing them at increased risk for this complication. Intraoperative tuberosity fractures during glenohumeral dislocation are less common during reverse shoulder arthroplasty than during unconstrained shoulder arthroplasty because of the lack of a rotator cuff attaching to the tuberosities, which could otherwise contribute to fracture during a dislocation maneuver. Fractures involving the humeral diaphysis should be reduced and a long-stem humeral implant placed. Allograft struts and cerclage cables may be added in patients with severe osteopenia (Fig. 32-1).
Intraoperative fractures involving the greater or lesser tuberosities (or both) are usually nondisplaced. Many of these fractures are stable or become stable once the humeral implant is inserted (Fig. 32-2). If a greater tuberosity fracture fragment that has maintained attachment of a substantial portion of the posterior rotator cuff is not satisfactorily stable, suture fixation of the tuberosity is performed and the postoperative rehabilitation adjusted accordingly to allow healing of the tuberosity. A greater tuberosity fracture fragment that is devoid of rotator cuff attachment and is unstable may simply be excised.
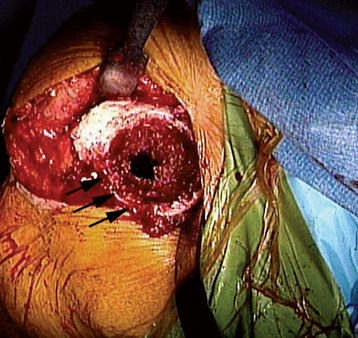
Intraoperative lesser tuberosity fractures commonly occur during retraction of the proximal humerus in the course of glenoid preparation and insertion. The thin anterior cortex of the humeral metaphysis, including the lesser tuberosity, may be crushed by the humeral retractor (Fig. 32-3). Creation of this fracture is often necessary to obtain adequate glenoid exposure during insertion of the reverse prosthesis through a deltopectoral approach. This fracture is without clinical consequence and can largely be ignored.
Glenoid
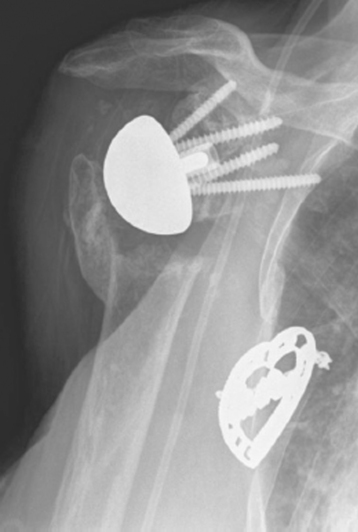
Fractures that involve only a small portion of the peripheral rim generally require no treatment, and the glenoid component can be inserted as planned. Glenoid fractures that extend into the central portion of the glenoid should be bone-grafted with the humeral head. The reverse glenoid component can be inserted to help secure the bone graft and internally fix the fracture. If the central post of the reverse component is firmly seated within native glenoid bone, consideration can be given to placing the humeral component in the same surgical setting. If the glenoid component does not seem secure or the central post of the glenoid base plate is not firmly seated in unfractured native glenoid bone, the humeral component should be initially omitted for 6 months to allow the fracture to heal. After 6 months a humeral component can be placed as the second part of a two-stage procedure (Fig. 32-4). Alternatively, if an intraoperative glenoid fracture occurs, the fracture can be bone-grafted and the humeral stem plus a hemiarthroplasty adapter placed (Fig. 32-5). After the fracture has healed and remodeled (around 6 months after the index attempt at reverse shoulder arthroplasty), the second stage of the procedure, consisting of implantation of the glenoid component, may be performed (Fig. 32-6).
Neurovascular Structures
Catastrophic injury to the neurovascular structures around the shoulder is exceedingly rare during reverse shoulder arthroplasty. The neural structures most at risk during reverse shoulder arthroplasty are the axillary and musculocutaneous nerves. These nerves should not be at risk for transection during primary arthroplasty using accepted operative technique. Neuropraxic injury caused by stretch most commonly involves the axillary nerve, but any nerves within the brachial plexus can be affected. Care should be taken when positioning the patient to maintain the cervical spine in neutral alignment to avoid a stretch injury to the brachial plexus. We have yet to establish risk factors for neuropraxic injury to the axillary nerve. Logic would suggest that patients with the most stiffness creating difficulty in glenoid exposure would be at the highest risk for this type of complication. Our clinical experience has not borne this out, however, and we are currently unable to predict which patients are most likely to suffer this complication. Patient education preoperatively is of paramount importance in dealing with neuropraxia inasmuch as patients are much more accepting if they have heard about the possibility of this complication before surgery. Axillary nerve (and other nerve) neuropraxia is treated by observation, with most patients recovering by 3 to 4 months postoperatively.
POSTOPERATIVE COMPLICATIONS
Postoperative complications are more common than intraoperative complications and occur in up to 50% of patients after reverse shoulder arthroplasty in some series.4 The most common postoperative complications include wound problems (dehiscence, hematoma), glenoid problems, humeral problems, acromial problems, scapular notching, instability (dislocation), stiffness, and infection.
Glenoid Problems
Glenoid problems after reverse shoulder arthroplasty are less common than after unconstrained total shoulder arthroplasty. In all cases of which we are aware, glenoid component failure after primary reverse shoulder arthroplasty has been associated with initial placement of the glenoid component in a superiorly oriented direction (Fig. 32-7) or implantation of the prosthesis in the presence of an intraoperative glenoid fracture (Fig. 32-8). These complications are best avoided. We implant the reverse prosthesis through a deltopectoral approach to avoid inadvertent placement of the glenoid component in a superiorly oriented position, which can occur with use of the superior lateral approach. If an intraoperative glenoid fracture occurs, we treat it as described previously in this chapter. When glenoid failure does occur, revision surgery consisting of glenoid reconstruction and conversion to a hemiarthroplasty is required (see Section Six).
Humeral Problems
Humeral problems after reverse shoulder arthroplasty are rare and can be divided into loosening of the humeral component, mechanical problems of the humeral component (polyethylene dissociation and polyethylene wear), and periprosthetic humeral fracture. Aseptic loosening of the humeral stem of a reverse prosthesis occurs in less than 1% of cases. The predominant risk factor for aseptic loosening of the humeral stem is proximal humeral bone loss (Fig. 32-9). Whenever loosening of a humeral stem occurs, infection must be ruled out (see later). In the rare instance of symptomatic aseptic humeral component loosening, treatment consists of revision of the humeral stem, usually combined with allograft reconstruction of the proximal humerus to provide osseous support of the proximal portion of the revision stem (see Section Six).
Mechanical problems of the humeral component are exceedingly rare and are related to the polyethylene liner. We are aware of one case of dissociation of the polyethylene liner from the humeral stem that was most likely related to incomplete seating of the polyethylene component at the index arthroplasty. In this scenario, revision surgery with replacement of the polyethylene liner is indicated. Polyethylene wear occurs medially on the rim of the polyethylene liner in many patients, as noted at the time of retrieval during revision surgery (Fig. 32-10). Such wear is related to scapular notching as discussed later.
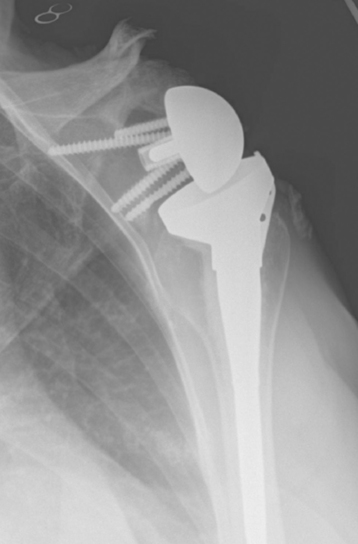
Periprosthetic humeral fractures are more common than loosening of the humeral component and are almost always the result of a fall or similar low-energy trauma (Fig. 32-11). The majority of these fractures occur just distal to the tip of the humeral stem, and most can be treated nonoperatively. Nonoperative treatment consists of fracture bracing, activity modification, pain medication, and frequent radiographic monitoring. If the fracture has not healed within 3 months, we will incorporate the use of an external bone stimulator (OL 1000 Bone Growth Stimulator, Donjoy Orthopedics, Vista, CA). Despite these measures, periprosthetic humeral fractures treated nonoperatively may take longer than 9 months to heal.5 Our criteria for recommending operative treatment of periprosthetic fractures (revision surgery; see Section Six) include complete displacement, angulation greater than 30 degrees, loosening or dislocation of the humeral component, or failure of nonoperative treatment (Fig. 32-12).
Acromial Problems
Occasionally, acromial stress fractures are seen after reverse shoulder arthroplasty (Fig. 32-13). These fractures result from deltoid tension applied to osteopenic bone. Frequently, these fractures are present preoperatively as a result of chronic superior migration of the humeral head with persistent acromiohumeral articulation. Postoperatively, deltoid tension may cause the fracture fragment to tilt inferiorly. Despite these radiographic findings, no specific treatment is necessary for this complication. Additionally, patients obtain satisfactory results even with this radiographic finding.
Scapular Notching
Though whether it should be considered a complication is debatable, notching of the scapula occurs within 2 years of surgery in half the patients who undergo reverse shoulder arthroplasty (Fig. 32-14). This radiographic finding most likely occurs as a result of mechanical impingement of the medial aspect of the humeral component and the lateral aspect of the scapula just inferior to the glenoid. The impingement is exacerbated when the patient internally rotates the shoulder. This mechanical impingement theory is further supported by the observation that patients’ internal rotation seems to improve as the scapular notch progresses, thus suggesting that the prosthesis must “carve out” a portion of the scapula to maximize postoperative internal rotation. Another theory of the cause of scapular notching is polyethylene wear causing osteolysis, although this theory currently has less support than the mechanical impingement theory.

Figure 32-14 Inferior scapular notch (arrows), which commonly occurs in patients after reverse shoulder arthroplasty.
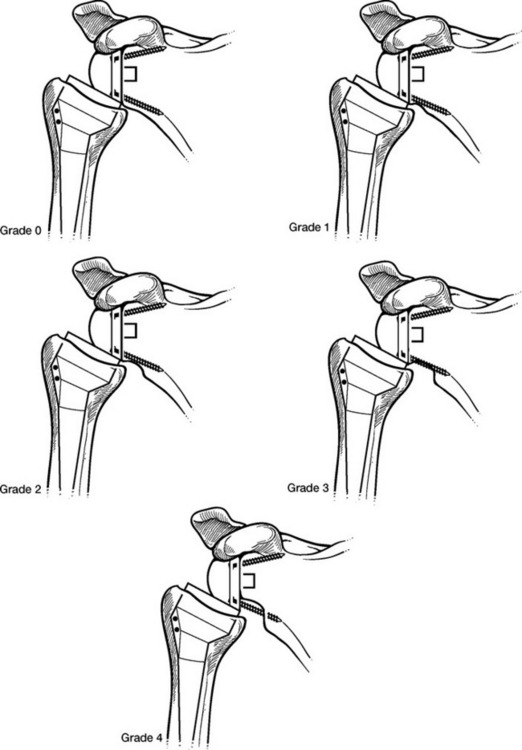
Scapular notching is commonly accompanied by a scapular osteophyte just medial to the notch (Fig. 32-15). The degree of scapular notching has also been graded by severity (Fig. 32-16).6 The best way to avoid scapular notching seems to be by initially placing the glenoid component inferiorly on the glenoid face and introducing slight inferior tilt during glenoid reaming (Fig. 32-17). Despite the concerning appearance of scapular notching, its clinical implications are unclear, with most of the evidence suggesting no adverse consequence. As long as the glenoid component remains stable, no treatment of an asymptomatic scapular notch is indicated.
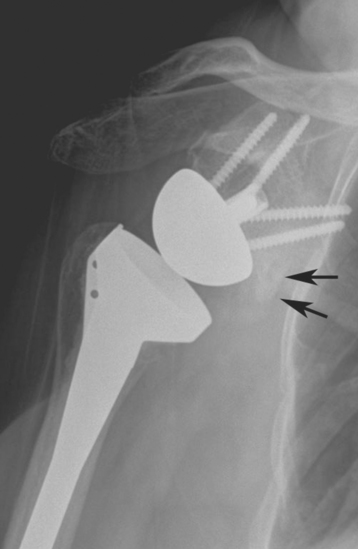
Figure 32-15 Scapular osteophyte (arrows) accompanying an inferior scapular notch after reverse shoulder arthroplasty.
Instability
Instability after reverse shoulder arthroplasty is the most common complication observed in our practice, and it occurs in approximately 5% of cases. Instability of a reverse prosthesis always occurs as a dislocation (Fig. 32-18). All dislocations that we have observed have occurred within 6 weeks of reverse shoulder arthroplasty. The majority of patients do not realize that their shoulder is dislocated, with the dislocation being detected on radiography during routine follow-up. We have observed a single case in which the patient would unintentionally dislocate his prosthesis anteriorly with arm extension but could perform a reduction maneuver himself to correct the dislocation (Fig. 32-19).
Instability of a reverse prosthesis can be related to various factors. In our experience, proximal humeral bone loss seems to be the greatest risk factor for dislocation of a reverse prosthesis. In this scenario, deltoid muscle tension is often solely responsible for stability of the implant because no rotator cuff or joint capsule exists to provide stability. Even if the deltoid is properly tensioned initially, it can gradually lose its tension and result in dislocation. A second major risk factor for dislocation of a reverse prosthesis is subscapularis insufficiency. All cases of dislocation that we have observed in our patients have occurred in those without a reparable subscapularis. A less common factor contributing to dislocation of a reverse prosthesis is mechanical impingement causing the prosthetic socket to be levered away from the glenoid component. This impingement usually occurs inferiorly as the arm is adducted and is often related to positioning of the glenoid component too superior on the glenoid face (Fig. 32-20). Finally, we have observed a single case in which a patient had sustained a neuropraxic injury to the axillary nerve that resulted in prosthetic instability secondary to an inability to contract the deltoid. In most cases of dislocation, one or more of these factors are present.
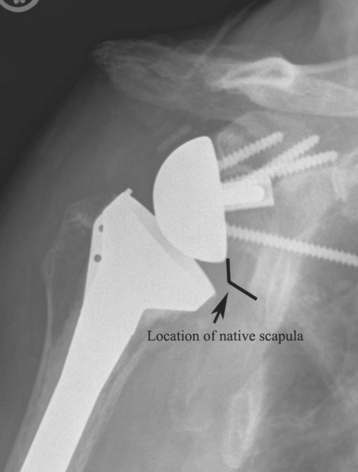
Figure 32-20 Positioning of the reverse glenoid component too superior on the glenoid face resulted in mechanical impingement.
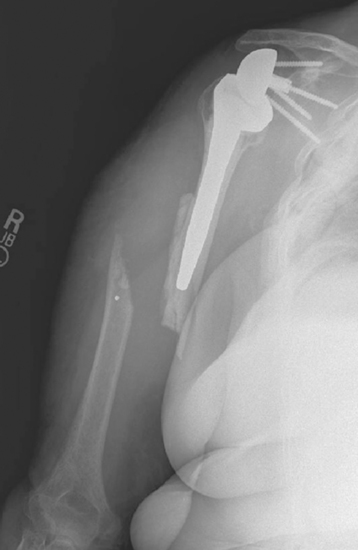
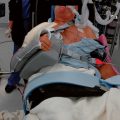
In the majority of cases, treatment of a dislocated reverse prosthesis consists of closed reduction and a period of bracing. Closed reduction is performed in the operating room with the patient either heavily sedated or under general anesthesia. Under fluoroscopic guidance an attempt is made to reduce the dislocation. If the prosthesis is successfully reduced, fluoroscopic examination is performed to ensure that mechanical impingement is not responsible for the instability. If the problem is not related to mechanical impingement and the prosthesis is reduced successfully, a brace is applied to maintain the arm with the humeral component centered on the glenoid component, generally in about 90 degrees of abduction with 30 degrees of forward flexion (Fig. 32-21). The patient maintains this brace at all times for 6 weeks, with radiographs performed in the brace every 7 to 10 days to confirm that the prosthesis has not dislocated (Fig. 32-22). After 6 weeks, the brace is discontinued and a normal rehabilitation regimen ensues.

Figure 32-21 A and B, Placement of a brace used for the treatment of a dislocated reverse prosthesis after closed reduction.

Figure 32-22 A and B, Radiograph obtained in the brace confirming maintenance of prosthetic reduction.
If the prosthesis is not reducible by closed means, mechanical impingement is causing the dislocation, or closed reduction with bracing has failed, open reduction with insertion of a thicker polyethylene spacer or metallic augment (or both) ensues (Fig. 32-23). Any mechanical impingement can simultaneously be addressed by careful removal of bone at the lateral aspect of the scapula just inferior to the glenoid component if necessary. Postoperatively, the patient is treated with the same bracing protocol used after closed reduction of a dislocated reverse prosthesis.
Infection
Infection after reverse shoulder arthroplasty occurs at the same frequency as after unconstrained shoulder arthroplasty (<1% of cases). Patients most at risk for infection are those with systemic illness (diabetes mellitus), those with compromised soft tissues (radiation-induced osteonecrosis, post-traumatic arthritis), and those with inflammatory arthropathy (rheumatoid arthritis). These infections are most commonly caused by Staphylococcus aureus or Propionibacterium acnes. Infections after shoulder arthroplasty can be divided into perioperative (within 6 weeks of surgery) and late (hematogenous) infections.
Late-appearing infections are treated by removal of the prosthesis and intravenous administration of antibiotics as detailed in Section Six. The decision whether to place a revision shoulder arthroplasty or continue with a resection arthroplasty is patient specific.
1 Wall B, Nové-Josserand L, O’Connor D, et al. Reverse total shoulder arthroplasty: A review of results by etiology. J Bone Joint Surg Am. 2007;89:1476-1485.
2 Constant CR, Murley AH. A clinical method of functional assessment of the shoulder. Clin Orthop Relat Res. 1987;214:160-164.
3 Constant CR. Assessment of shoulder function. In: Gazielly D, Gleyze P, Thomas T, editors. The Cuff. New York: Elsevier; 1997:39-44.
4 Werner CML, Steinmann PA, Gilbart M, Gerber C. Treatment of painful pseudoparesis due to irreparable rotator cuff dysfunction with the Delta III reverse-ball-and-socket total shoulder prosthesis. J Bone Joint Surg Am. 2005;87:1476-1486.
5 Kumar S, Sperling JW, Haidukewych GH, Cofield RH. Periprosthetic humeral fractures after shoulder arthroplasty. J Bone Joint Surg Am. 2004;86:680-689.
6 Valenti P, Boutens D, Nerot C. Delta 3 reversed prosthesis for osteoarthritis with massive rotator cuff tear: Long term results (>5 years). In: Walch G, Boileau P, Molé D, editors. 2000 Prosthèses d’Epaule … Recul de 2 à 10 Ans. Paris: Sauramps Medical; 2001:253-259.