Restrictive Lung Diseases: General and Ventilatory Management
A A restrictive lung disease is any disease in which the ability to inhale is affected.
B Restrictive diseases of pulmonary origin are frequently associated with an increase in pulmonary fibrous tissue. The result is an overall increase in pulmonary elastance and a decrease in pulmonary compliance.
C Characteristic pulmonary function findings (Table 22-1)
TABLE 22-1
Changes in Pulmonary Function Associated With Obstructive and Restrictive Lung Disease
| Pulmonary Function Study | Obstructive Disease | Restrictive Disease |
| TLC | Normal or increased | Decreased |
| VC | Normal or decreased | Decreased |
| FRC | Increased | Normal or decreased |
| RV | Increased | Normal or decreased |
| RV/TLC ratio | Increased | Normal |
| FEV1% | Decreased | Normal |
| MMEFR25%-75% | Decreased | Normal or decreased |
1. Decreased or normal tidal volume (Vt).
2. Decreased or normal residual volume (RV).
3. Decreased or normal expiratory reserve volume (ERV).
4. Decreased or normal inspiratory reserve volume (IRV).
5. Decreased total lung capacity (TLC).
6. Decreased vital capacity (VC).
7. Decreased inspiratory capacity (IC).
8. Decreased or normal functional residual capacity (FRC).
9. Flow rate studies usually are normal in pure restrictive lung diseases; however, flow rates may be decreased when an obstructive component is also present.
10. Pulmonary and/or thoracic compliance and total compliance are usually severely decreased.
11. There is a progressive increase in the work of breathing as the severity of the disease increases.
a. Initially alveolar minute ventilation is normal or increased, but as the disease progresses alveolar minute ventilation progressively decreases.
b. Arterial blood gases may follow the same pattern as that seen in obstructive lung disease. The initial presenting symptom may be chronic respiratory alkalosis with hypoxemia, but as the disease progresses chronic respiratory acidosis with hypoxemia may develop.
II Pulmonary Restrictive Lung Diseases
A Interstitial pulmonary fibrosis: A disease characterized by the excessive formation of connective tissue in the process of repairing chronic or acute tissue injury.
1. Etiology: Any permanent injury to the lung (e.g., infection, inflammation, and allergy).
a. Causes of localized fibrosis
(1) Long-term exposure to various inhalants. Specific pneumoconioses are listed in Table 22-2.
TABLE 22-2
| Disease | Causative Agent |
| Silicosis | Silica dust |
| Farmer’s lung | Moldy hay |
| Stannosis | Tin dust |
| Silo-filler’s disease | Nitrogen dioxide |
| Coal worker’s pneumoconiosis | Coal dust |
| Asbestosis | Asbestos |
| Berylliosis | Beryllium |
| Siderosis | Iron dust |
(2) Short-term exposure to toxic inhalants may also cause diffuse fibrosis (e.g., chlorine gas, ammonia, polyvinyl chloride, smoke inhalation, and radiation therapy).
(3) Diseases of unknown etiology that often show diffuse fibrosis:
a. Inflammatory reaction in response to organic or inorganic foreign agents.
b. Inflammation is followed by cellular infiltration and acute vasculitis with local hemorrhage and thrombus formation, resulting in scar tissue.
a. Primary symptom: Progressive dyspnea on exertion and ultimately at rest.
c. As disease continues, progressive respiratory impairment and often cor pulmonale.
d. Physical examination findings:
(3) Restricted chest wall and diaphragmatic movement
(4) Diffuse, dry, crackling rales
(5) Increased work of breathing
(1) Small lung with large heart and elevated diaphragm
(2) Fine reticular or nodular pattern involving entire lung but predominantly the lower lobes
f. Arterial blood gases and pulmonary function studies as outlined in Section I, General Comments.
a. Removal of patient from environment causing the fibrotic changes if possible
b. Therapy for underlying disease entity
e. Oxygen therapy: As disease progresses, increased dyspnea is reported. Many patients are relatively refractory to oxygen therapy. Continuous positive airway pressure (CPAP) is often helpful. Care must be taken when disconnecting patient from CPAP because severe acute hypoxemia may ensue.
f. Penicillamine therapy has improved subjective assessment of patients.
g. Cyclosporine is used in late stages.
h. Plasmapheresis is effective in a few patients with high titers of immune complexes in later stages.
i. Total heart-lung transplant has been successful in some patients.
j. Mechanical ventilation: If these patients progress to mechanical ventilation, Vt delivery is limited because of decreased compliance. This results in increased inspiratory pressure that is not associated with overdistention of the lung.
B Pleural effusion: Accumulation of fluid in pleural space.
1. Normally the capillary network of the visceral pleural surface produces the fluid lining of the pleura, and any excess is removed by the lymphatic system.
2. Any disturbance in production of this fluid or in its removal can lead to the development of pleural effusion.
3. Primary causes: Inflammation and circulatory disorders.
4. The effusion compresses the lung on the affected side.
5. The effusion is gravity dependent and may shift with positional change.
a. Hydrothorax: A thin clear transudate caused by CHF, chronic nephritis, or pulmonary neoplasm.
b. Empyema (pyothorax): An effusion consisting entirely of pus caused by a bacterial infection.
c. Hemothorax: Frank blood caused by a malignancy, pulmonary infarction, or ruptured blood vessel.
d. Chylothorax: Accumulation of chyle resulting from the obstruction or trauma of the thoracic duct.
e. Fibrothorax: An accumulation of fibrous tissue normally secondary to a prolonged effusion.
C Pneumothorax: Accumulation of air within the pleural space.
1. If air enters the pleural space, the pressure within the space changes from subatmospheric to atmospheric or supraatmospheric pressure.
a. The increased pressure compresses lung tissue and results in atelectasis.
b. Ventilation of the lung on the affected side is decreased as a result of elimination of the subatmospheric intrapleural pressure.
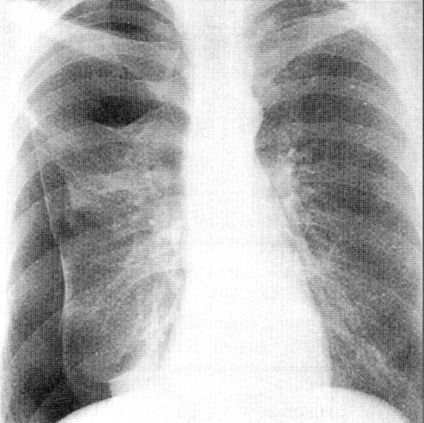
a. Diagnosis is suggested by history and clinical presentation.
b. Definitive diagnosis is confirmed by chest radiography (Figure 22-2).
3. Types: Open and under tension.
a. In an open pneumothorax, there is no buildup of pressure because the gas is allowed to move freely in and out of the pleural space.
b. A tension pneumothorax results from the presence of a one-way valve, which allows gas only to enter the pleural space and not to leave it. This results in significant increases in pressure within the pleural space. If untreated it may quickly result in cardiac arrest.
(a) Increased difficulty in ventilation: If patient is mechanically ventilated, airway pressure increases with each breath.
(b) Patient’s vital signs begin to deteriorate as mean intrathoracic pressure increases.
(c) Breath sounds are absent on the affected side.
(d) The affected side is hyperresonant to percussion.
(e) Trachea and mediastinum may be shifted toward the unaffected side as the extent of tension pneumothorax increases.
(h) These clinical signs are more predominant if the patient is using a mechanical ventilator than if he or she is ventilating spontaneously. This is because of the greater pressure gradients developed, forcing more gas into the pleural space.
(2) Treatment: Decompression of the thorax by chest tube insertion.
D Cardiogenic pulmonary edema: Active movement of fluid across alveolar capillary membrane into alveoli as a result of increased capillary hydrostatic pressures.
1. Normally a fine balance exists among capillary colloid osmotic (oncotic) pressure, capillary hydrostatic pressure, interstitial hydrostatic pressure, and interstitial colloid osmotic (oncotic) pressure across the pulmonary capillary bed (see Chapter 14).
2. Usually a small net pressure forces fluid into the interstitial space. This interstitial fluid is drained by the lymphatics.
3. If capillary hydrostatic pressure increases significantly, the net pressure forcing fluid into the interstitial space increases, and eventually fluid moves directly into the alveoli.
4. Primary cause: Acute left ventricular failure (CHF)
a. The hydrostatic pressure of the pulmonary vascular bed is increased because of the inability of the left side of the heart to accept the blood presented to it.
b. This increased pressure offsets the normal pressure dynamics at the alveolar capillary membrane.
5. Secondary cause: Increased vascular volume causing an increase in pulmonary capillary hydrostatic pressure.
6. Acute right ventricular failure (CHF)
a. Systemic edema develops as a result of right ventricular failure.
b. The inability of the right side of the heart to accept the blood presented to it results in blood pooling in the periphery.
c. Dependent edema (pedal edema), neck vein distention, and hepatomegaly are common clinical findings.
d. It is not unlikely for patients with right-sided heart failure to eventually develop left-sided heart failure and those with left-sided heart failure to develop right-sided heart failure.
b. Intraaortic balloon counterpulsation
c. Oxygen therapy: Frequently high FIO2 is required.
d. CPAP, by mask, at 8 to 12 cm H2O has been helpful in some patients and may avoid intubation if pulmonary edema can be stabilized quickly.
e. Noninvasive positive pressure ventilation (NPPV) has also been shown to improve oxygenation. It offers the added benefit of improving ventilation in patients who begin to develop respiratory muscle fatigue.
(1) Mechanical ventilation with PEEP can improve or further worsen cardiac function.
(2) The increased mean airway pressure (as with CPAP) decreases venous return in left-sided heart failure.
(3) Marked increases in mean airway pressure can markedly reduce pulmonary perfusion and increase deadspace ventilation.
(4) When mechanical ventilator settings are titrated, markedly increasing minute ventilation should be avoided because PCO2 increases with hemodynamic instability.
(5) Stabilization of cardiac function improves the deadspace volume/tidal volume (Vd/Vt) ratio and thus returns PCO2 to normal.
(6) If increases in minute ventilation result in no change or an increase in PCO2, lack of pulmonary perfusion is most likely the cause of the PCO2 increase.
(7) Ventilator settings generally are similar to those for all patients without lung disease. Efforts should be made to improve ventilation and oxygenation without causing a secondary, ventilator-induced lung injury (see Chapters 39, 40, and 41).
(8) These patients generally require pharmacologic control during ventilation.
E Noncardiogenic pulmonary edema
1. The development of interstitial or true pulmonary edema from noncardiogenic origins.
2. Pathophysiologic etiologies
a. Altered permeability of capillary endothelial cells, allowing an increased quantity of fluid into the interstitial space.
b. Decreased capillary colloid osmotic pressure, which increases the pressure gradient, allowing more fluid to enter the interstitial space.
c. Altered lymphatic function, preventing normal drainage of the pulmonary interstitium, thereby allowing fluid to accumulate.
d. Alveolar epithelial damage, allowing fluid to enter the alveoli.
(1) Neurogenic origin is primarily a result of an acute insult to the central nervous system.
(2) It causes an increased sympathetic discharge, leading to a sudden intravascular fluid shift into the pulmonary circulation.
(3) The imbalance in hydrostatic and osmotic pressures created causes fluid to enter the interstitial space.
(1) The exact mechanism is poorly defined.
(2) It is presumed that drugs, especially narcotics and sedatives, have a direct effect on increasing pulmonary capillary membrane permeability.
c. High-altitude pulmonary edema
(1) The mechanism is poorly understood.
(2) It is thought to be the result of severe hypoxemia and vasoconstriction of the microcirculation.
(3) Edema develops as blood flows under high pressure through the patent portion of the microvasculature.
(1) It develops after the sudden reexpansion of a lung that had been collapsed for several hours.
(2) The sudden reexpansion causes a negative pressure in the interstitium, creating a large pressure gradient across the capillary membrane and an increased transudation of fluid.
(3) The rapid removal of pleural effusion fluid (≥1000 ml) may produce edema.
e. Pulmonary edema associated with renal disease
(1) The mechanism is poorly defined.
(2) It may occur in patients with acute glomerulonephritis or nephrotic syndrome.
(3) It is also seen in patients with chronic uremia and in patients requiring long-term hemodialysis.
f. Other clinical conditions known to lead to noncardiogenic pulmonary edema:
F Acute respiratory distress syndrome (ARDS) (see Chapter 23).
G Pneumonia: Pneumonitis caused by a microorganism.
1. Pneumonias are a leading cause of death in the United States and account for 10% of admissions to general medical floors.
2. Pathophysiology of pneumonia
a. Microorganisms cause inflammation of pulmonary mucosa, resulting in edema and phagocytic infiltration.
b. Exudation and consolidation result.
c. Consolidation is typically localized, as in lobar pneumonias.
3. Bacterial pneumonia (Table 22-3)
TABLE 22-3
Comparison of Clinical and Laboratory Manifestations of Bacterial and Viral Pneumonias
| Symptom | Bacterial | Viral |
| Onset | Abrupt | Gradual |
| Fever | High | Low grade |
| Chills | Common | Uncommon |
| Sputum | Purulent, thick | Mucoid, thin |
| Tachycardia | Frequent | Rare |
| Hypoxemia | Common | Uncommon |
| Chest radiography results | Consolidation | Consolidation rare |
| White blood cell count | >10,000/mm3 | <10,000/mm3 |
| Pleuritic pain | Occasional | Uncommon |
4. Nonbacterial (viral or fungal) pneumonia (see Table 22-3)
a. Clinical signs and symptoms (occasionally mild and frequently undiagnosed)
1. Pulmonary embolism is the occlusion of the pulmonary artery or one of its branches by a substance carried in the blood, normally a blood clot.
2. A blood clot that is attached to its site of origin is referred to as a thrombus. Once detached it is referred to as an embolus.
3. The actual substance may be fat, blood, air, amniotic fluid, or a tissue fragment.
a. The most common sites of thrombus formation are the deep veins of the lower extremities and pelvis and within the right side of the heart.
b. Thrombus development is most prevalent in patients who are immobilized by pain or who are debilitated, paralyzed, or require prolonged bed rest.
c. Factors facilitating thrombus formation
d. Dependent lung regions are most commonly involved with pulmonary emboli.
e. Pulmonary infarction occurs in approximately 10% of patients with pulmonary emboli, especially if there is a history of cardiac disease.
a. Deadspace ventilation is significantly increased.
b. Total ventilation markedly increases in an effort to maintain normal PCO2.
c. A minute volume-PCO2 disparity develops (large minute ventilation with near-normal PCO2).
d. With large emboli pulmonary artery pressures increase, especially if there is underlying cardiac disease.
a. Patient has dyspnea and chest pain.
c. Frequently cough, faintness, and anxiety accompany pulmonary embolus.
d. Thrombophlebitis is often noted (frequently at the site of embolus formation).
e. If a massive embolus is present, there may be:
a. In some cases decreased lung volume, atelectasis, pleural effusion, and signs of pulmonary infarction may be present.
b. In rare cases there is a local reduction in vascular markings and an enlarged pulmonary artery.
a. Lung volumes and capacities are decreased.
b. Flow studies are usually normal.
c. Arterial blood gases usually reveal hypoxemia with a normal acid-base balance or a respiratory alkalosis.
a. Ventilation/perfusion scans may help differentiate pulmonary embolism from other perfusion abnormalities.
b. Findings must be correlated with patient’s clinical findings and history.
10. Pulmonary angiography is considered definitive in the diagnosis of pulmonary embolism.
I Pulmonary alveolar proteinosis
1. A disease characterized by alveoli filled with a liquid high in protein and lipid.
2. Alveolar walls are normal, but only scattered macrophages are noted.
a. The origin is unknown, but it is theorized that type II alveolar epithelial cells produce an excess of surfactant, lipid, and protein.
b. This substance is poorly cleared by defective macrophages.
6. Chest radiographic film reveals infiltrates in perihilar regions and bases of the lung.
7. Pulmonary function studies may be normal, but diffusing capacity is decreased.
8. Diagnosis is made primarily by open lung biopsy, bronchoalveolar lavage, or the measurement of lactic dehydrogenase levels.
III Thoracoskeletal Restrictive Lung Diseases
A Deformities of thoracic cage that result in limited movement of the chest demonstrate pulmonary function patterns consistent with restrictive lung disease.
B If the deformity is severe enough, a significant increase in the work of breathing results.
C Increased work of breathing eventually leads to hypoxemia, hypercapnia, and possible heart failure.
D Most commonly encountered thoracic abnormalities leading to restrictive lung disease are:
1. Scoliosis: Gradual curvature of vertebral column in lateral plane of body (Figure 22-3).

a. One of the most common thoracic deformities.
2. Kyphosis: Posterior curvature of thoracic vertebral column, resulting in a bony hump.
a. Frequently develops in older individuals with degenerative osteoarthritis.
b. May develop in individuals with chronic obstructive pulmonary disease (COPD).
3. Kyphoscoliosis: Combination of thoracic scoliosis and kyphosis.
1. No primary treatment is indicated in most cases.
2. Scoliosis may be managed surgically.
3. Most treatment focuses on secondary pulmonary problems (e.g., pneumonia and asthma).
4. Some patients with severe kyphoscoliosis develop progressive ventilatory muscle weakness and fatigue and may require nocturnal mechanical ventilatory assistance and oxygen therapy.
5. During acute pulmonary problems that require endotracheal intubation and mechanical ventilation, rates and Vt settings differ from normal because of decreased lung volumes.
IV Neurologic-Neuromuscular Restrictive Lung Diseases
A Weakness or paralysis of the muscles of ventilation results in a pulmonary function pattern consistent with restrictive lung disease.
B Myasthenia gravis: A disease of the myoneural junction in which transmission of impulses across the motor endplate is inhibited.
1. Etiology: Myasthenia gravis is most often an acquired immunologic abnormality, although some cases may be genetic. Functionally it appears that acetylcholine is improperly released, synthesized, or prematurely hydrolyzed before crossing the neuromuscular junction.
2. The disease is most common in women aged 20 to 49 years, but it affects individuals of both sexes and all ages, with approximately 10% of patients having a tumor of the thymus gland.
3. The disease is manifested by generalized muscle weakness and most commonly demonstrates a descending paralysis.
4. The primary symptoms normally are ocular, progressing to facial muscle weakness or paralysis, followed by pharyngeal and laryngeal weakness and finally respiratory muscle weakness.
5. Patients frequently have a chief complaint of easy fatigability.
a. Diagnosis is based primarily on history and symptomatology.
b. The administration of a parasympathomimetic of the cholinesterase inhibitor type confirms the diagnosis. Increased muscle strength is normally noted shortly after the administration of the drug.
a. Patients are maintained with cholinesterase inhibitor therapy.
b. Treatment with atropine to reverse the side effects of the cholinesterase inhibitor.
c. Thymectomy is recommended in most cases. In some patients complete remission has been reported.
(1) Adrenocorticotropic hormone; a 10-day course may be prescribed.
(3) Symptoms deteriorate during administration; however, remission is frequent after a 10-day course.
h. In severe cases, intubation and mechanical ventilation are used as supportive measures until drug therapy is titrated.
8. Myasthenic versus cholinergic crisis
a. An acute exacerbation of the disease process producing weakness is termed a myasthenic crisis.
b. An acute decrease in muscle strength as a result of the excessive use of cholinesterase inhibitors is termed a cholinergic crisis.
c. The Tensilon (generic name, edrophonium chloride) test is used to differentiate between a myasthenic and cholinergic crisis. Tensilon is a short-acting (5-min) cholinesterase inhibitor.
(1) If the patient has a myasthenic crisis, the administration of Tensilon will improve muscle strength.
(2) If a cholinergic crisis is present, Tensilon will increase muscle weakness and exacerbate symptomatology.
(3) Muscle strength can be evaluated using serial VC or maximum inspiratory pressure (MIP) measurements.
C Guillain-Barré syndrome: Polyneuritis primarily affecting the peripheral motor and sensory neurons.
1. The etiology is unclear. The disease may be viral or traumatic. An increase in the number of cases has been reported after viral infection (e.g., varicella-zoster, HIV, and cytomegalovirus) and vaccination (e.g., poliomyelitis and swine flu).
2. The syndrome affects those of all ages but is more prevalent in adults.
3. The signs and symptoms show a symmetric ascending pattern of sensory abnormalities that may progress to actual paralysis.
4. The disease is normally self-limiting and is reversible with time. The amount of residual effects depends on the extent of demyelination occurring during the active disease state.
5. Diagnosis is made by the presentation of the disease, high protein content in the cerebral spinal fluid, and the reversible nature of the disease.
6. Treatment is purely symptomatic, the patient frequently requiring ventilatory support.
7. As with myasthenia gravis, careful monitoring of the patient’s ventilatory reserves is indicated.
D Other neuromuscular or neurologic diseases that may show a restrictive lung disease pattern
1. Some of these patients require mechanical ventilation for varying time periods.
2. Unless compounding pulmonary problems develop, the lungs of these patients are normal. As a result mechanical ventilation is relatively uncomplicated.
3. Many of these patients want to feel the ventilator expand their lungs; thus Vt should be large, <12 ml/kg.
4. As a result the rate is frequently slow, 8 to 16 breaths/min.
5. All other variables are titrated based on the patient’s response.
V Abdominal Restrictive Lung Diseases
A Increased size of abdominal contents results in limited movement and elevation of the diaphragm.
B The limited diaphragmatic movement will demonstrate pulmonary function findings consistent with those of restrictive lung disease.
C Conditions that may show a restrictive pattern
D Pickwickian syndrome: A complex of cardiopulmonary symptoms primarily caused by obesity.
1. It is also referred to as obesity-hypoventilation syndrome.
2. The syndrome is characterized by:
b. Alveolar hypoventilation (more pronounced with sleep) with episodes of sleep apnea
d. Severe hypoxemia (more pronounced with sleep)
3. Etiology is unclear; however, the major cause appears to be extreme obesity. Genetics may also play a role.
a. Weight loss may reverse the syndrome.
b. A high percentage of patients experience upper airway obstruction during sleep, especially in the supine position. The obstruction is believed to be soft tissue obstruction.
4. Frequently the hypoxemia and hypoventilation develop only during sleep (obstructive sleep apnea).
A Usually associated with obesity.
B Soft tissue occludes the upper airway.
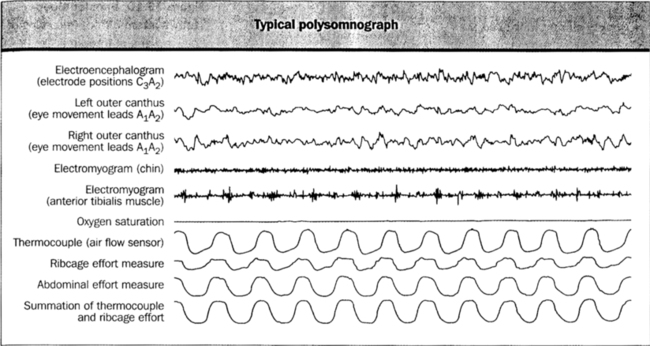
C Respiratory efforts are present; however, airflow is blocked (Figure 22-4).
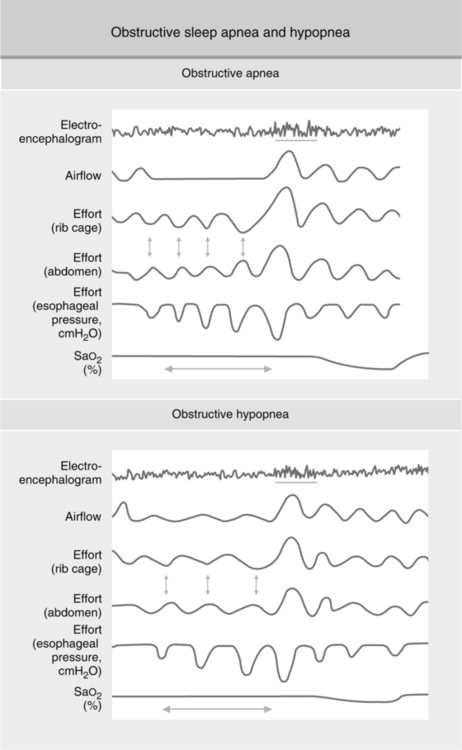
D These apneic episodes result in hypoventilation and hypoxemia.
E The sleep of these patients is commonly broken and restless, leading to generalized somnolence.
d. Increased neck circumference
e. Use of alcohol or other sedatives
f. Certain craniofacial abnormalities
(1) Primary treatment is weight loss.
(2) Body positioning (i.e., sleeping on one’s side or with extra pillows as adjuncts).
(3) No alcohol or heavy meals in the evening.
(4) Smoking cessation (to reduce airway inflammation).
(5) Nasal CPAP helps to relieve airway obstruction and prevents arterial desaturation and hypercarbia at night.
VII Smoke Inhalation and Carbon Monoxide Poisoning
1. Etiology: The inhalation of by-products of a fire (i.e., smoke and other noxious gases).
a. Edema, congestion, sloughing of mucosal membranes of the oral and nasal pharynx, larynx, trachea, and bronchi
b. Obliterative bronchiolitis and alveolar edema
c. Development of pulmonary edema
d. Atelectasis caused by airway obstruction with fibrin, edema, fluid, carbon particles, white blood cells, and epithelial debris
3. Clinical presentation (it may take 24 to 48 hours for symptoms to develop fully)
d. Facial burns, singed nasal hairs, stridor, and grunting (all indicative of upper airway burns)
e. Results of radiographic studies are normal for the first 24 to 48 hours; however, signs of pulmonary edema, atelectasis, and infiltrates subsequently develop.
a. Establishment of an artificial airway. This is imperative if upper airway burns accompany the smoke inhalation. If an airway is not established early, subsequent edema may prevent cannulation of the airway.
b. Oxygen therapy (100% if CO poisoning is also present)
c. Fluid and electrolyte therapy
g. Mechanical ventilation if pulmonary burns present
(1) Because pulmonary burns result in severe mucosal edema, air trapping and auto-PEEP frequently develop.
(2) As a result mechanical rates should be low, 8 to 16/min, and expiratory times should be long.
(3) The approach generally used is similar to that for those with COPD (see Chapters 39, 40, and 41).
(4) Some patients may develop acute lung injury and ARDS (see Chapter 23).
1. A result of inspiring by-products of the incomplete combustion of carbon or carbon-containing material
a. Carbon monoxide combines strongly with hemoglobin to form carboxyhemoglobin (hemoglobin’s affinity for CO is 210 times that of O2).
b. The total capability of the organism to carry oxygen to the tissues is reduced (anemic hypoxia).
c. The oxyhemoglobin dissociation curve also is shifted to the left, further limiting the amount of O2 available at the tissue level.
d. The likelihood of tissue hypoxia increases as COHb% saturation increases.
e. Increased levels of carbon monoxide interfere with intracellular oxygenation, resulting in histotoxic hypoxia.
3. Clinical manifestations (symptomatology based on carboxyhemoglobin levels):
a. Normally asymptomatic: <20%
b. Headache, exertional dyspnea, impaired judgment, nausea, and vomiting: 20% to 60%
c. Loss of consciousness, convulsions, and deep coma: 60% to 80%
4. Radiography findings: Chest radiographic film may show abnormalities consistent with pulmonary edema, usually interstitial in location.
a. Analysis of arterial blood for carboxyhemoglobin levels.
(1) A co-oximeter is required to determine actual carboxyhemoglobin and oxyhemoglobin levels.
(2) A pulse oximeter measures the oxygen saturation of functional hemoglobin, resulting in an erroneous (high) reading.
(3) Pao2 is a measure of oxygen dissolved in plasma; therefore, it is not a helpful measurement.
c. Frequently a metabolic acidosis caused by lactic acid accumulation is noted.
a. Oxygen therapy: One hundred percent O2 is indicated until COHb% levels reach ≤10%. Increasing the arterial Po2 decreases the half-life of COHb%. On inhalation of room air, the half-life of COHb is approximately 5 to 6 hours, whereas the inhalation of 100% O2 decreases the half-life to approximately 90 minutes.
b. Hyperbaric oxygen therapy: The inhalation of oxygen at greater than atmospheric pressure (usually 2 to 3 atmospheres). There is conflicting evidence over the use of hyperbaric oxygen therapy. It is generally indicated, where available, for patients with serious carbon monoxide poisoning. Hyperbaric oxygen therapy at 3 atmospheres can decrease the half-life of COHb to 23 minutes.
c. With high COHb levels (≥40% to 50%), intubation and mechanical ventilation may be necessary.
VIII Drug-Induced Pulmonary Disease
A Many drugs used for the management of various problems have been linked to pulmonary side effects.
B Pulmonary response is usually one of three types:
C Response and magnitude of a response depend on many factors.
D The group of drugs that most commonly induce a pulmonary reaction are cytotoxic drugs used in chemotherapy for cancer. Specific agents commonly causing problems are:
E Other agents that have been reported to produce pulmonary side effects are: