Respiratory System
ICD-10-PCS Example from Index
Rhinoplasty
Rhinorrhaphy—see Repair, Nose 09QK
Rhinoscopy 09JKXZZ
Functions of the Respiratory System
• Delivering oxygen (O2) to the blood for transport to cells in the body.
• Excreting the waste product of cellular respiration, carbon dioxide (CO2).
• Filtering, cleansing, warming, and humidifying air taken into the lungs.
• Regulating the pH of the blood.
• Helping the production of sound for speech and singing.
• Providing the tissue that receives the stimulus for the sense of smell, olfaction.
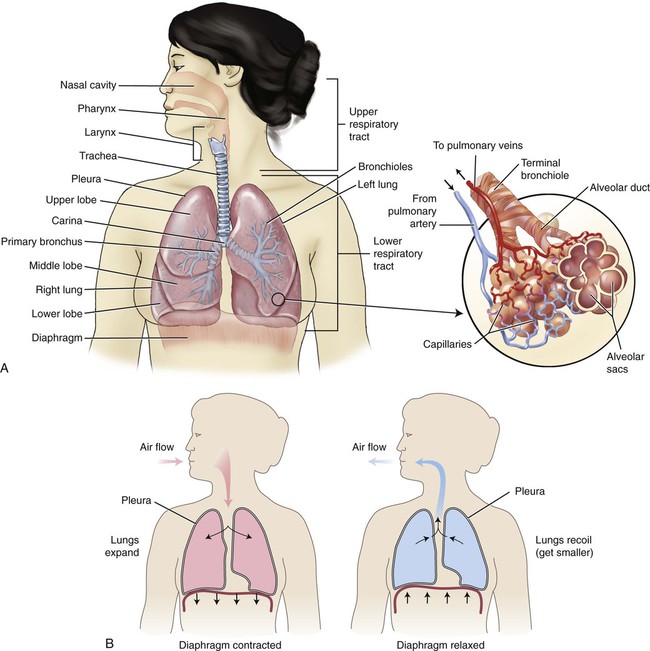
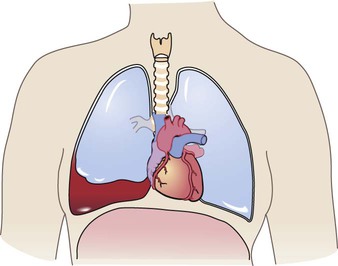
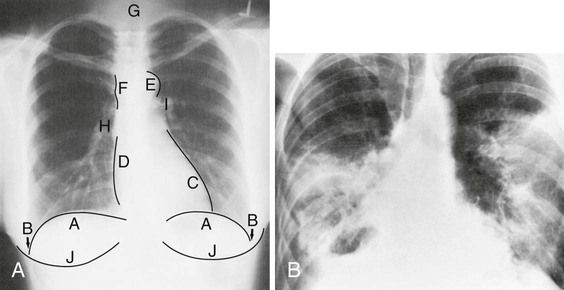
The respiratory system (Fig. 10-1) partners with the circulatory system to deliver oxygen to and remove carbon dioxide from the cells of the body. Breathing in (inspiration or inhalation) pulls air containing oxygen into the lungs, where it passes into the circulatory system. Carbon dioxide is released when air is pushed out of the lungs (expiration or exhalation). When one dies, one breathes out and no longer breathes in again—hence the expression the patient has “expired.” Using the combining form spir/o, meaning “to breathe,” we can see that respiration means to breathe again (and again). The term ventilation is used to describe the movement of air into the lungs, whether it is a natural or an artificial activity.
Anatomy and Physiology
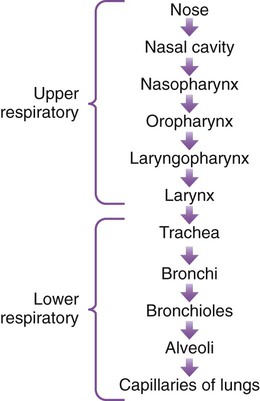
The respiratory system is anatomically divided into conduction passageways and gas exchange surfaces. The upper respiratory tract (the nose, pharynx, and larynx) and the lower respiratory tract (the trachea, bronchial tree, and lungs) (Fig. 10-1, A) make up the two sections of the conduction passageways. The gas exchange surfaces are the alveoli of the lungs and the cells of the body.
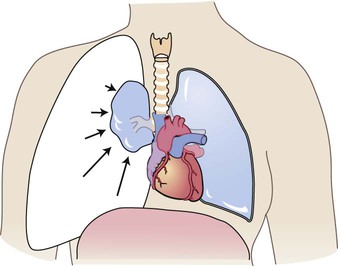
There are two main forms of respiration: external respiration and internal respiration. External respiration is the process of exchanging oxygen (O2) and carbon dioxide (CO2) between the lungs and the blood (Fig. 10-1, B). Internal respiration is the exchange of gases between the blood and the cells of the body. A third type of respiration, cellular respiration (also called cellular metabolism), is the use of oxygen to generate energy.
Upper Respiratory Tract
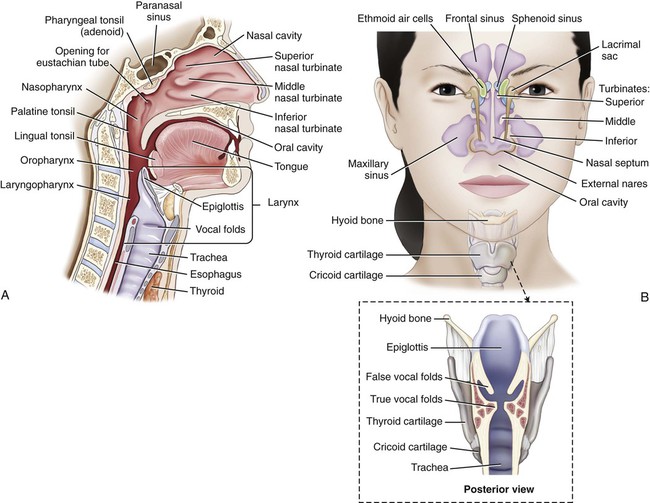
The upper respiratory system encompasses the area from the nose to the larynx (Fig. 10-2, A). Air can enter the body through the mouth, but for the most part it enters the body through the two nares (nostrils) of the nose that are separated by the nasal septum. The nasal turbinates (also called nasal conchae) are three scroll-shaped bones (inferior, middle, and superior) that increase the surface area that air must pass over on its way to the lungs (Fig. 10-2, B). The vibrissae (the coarse hairs in the nose) serve to filter out large particulate matter, and the mucous membrane and cilia (small hairs) of the respiratory tract provide a further means of keeping air clean, warm, and moist as it travels to the lungs. The cilia continually move in a wavelike motion to push the sticky mucus and debris out of the respiratory tract. The air then travels up and backward, where it is filtered, warmed, and humidified by the environment in the upper portion of the nasal cavity. Damage to the cilia keeps the germ-laden mucus from leaving the body and consequently provides a hospitable environment for infection. Figure 10-3 illustrates the route of air into the body. The receptors for olfaction are located in the nasal cavity, which is connected to the paranasal sinuses, collectively named for their proximity to the nose.
Lower Respiratory Tract
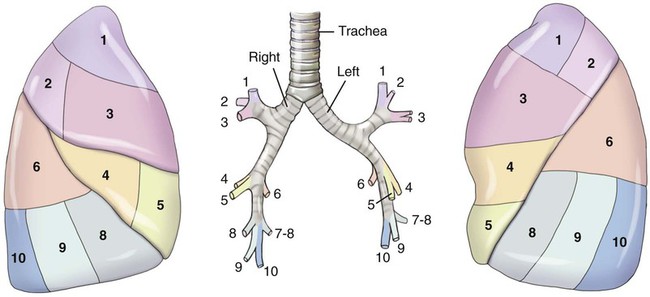
Each lung is composed of sections called lobes, which correspond to the secondary bronchi that supply these areas within each lung. The right lung is made up of three lobes, whereas the left has only two (see Fig. 10-1, A). The abbreviations for the lobes of the lungs are RUL (right upper lobe), RML (right middle lobe), RLL (right lower lobe), LUL (left upper lobe), and LLL (left lower lobe). Within each of these lobes, the secondary bronchi branch out to tertiary bronchi, and the areas that each supplies are referred to as segments (Fig. 10-4). Each segment is supplied with blood from a segmental artery that branches off the pulmonary arteries. The segments are named by their location (e.g., anterior, posterior, apical, basal, medial, or lateral). The lingula is the area where the superior and inferior segments appear on the left lung. Although named for its tongue-like shape, it has been postulated that it may represent the remnants of a left middle lobe. At the end of the segmental bronchi are still smaller branches called bronchioles. These bronchioles end in terminal bronchioles that branch to respiratory bronchioles. The respiratory bronchioles extend into microscopic alveolar ducts capped by air sacs called alveoli (sing. alveolus). Each alveolus is in contact with a blood capillary to provide a means of exchange of gases. At this point O2 is diffused across cell membranes into the blood cells, and CO2 is diffused out to be expired.
The muscles responsible for normal, quiet respiration are the dome-shaped diaphragm and the muscles between the ribs (intercostal muscles). On inspiration, the diaphragm is pulled down as it contracts and the intercostal muscles expand, pulling air into the lungs because of the resulting negative pressure (see Fig. 10-1, B). On expiration the diaphragm and intercostal muscles relax, pushing air out of the lungs.
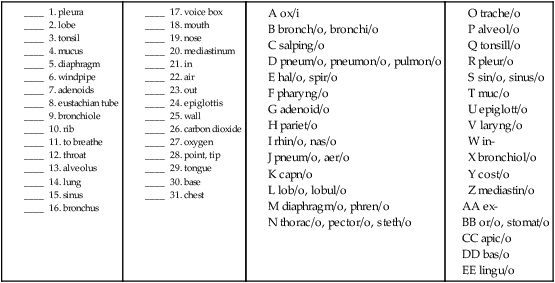
Combining Forms for the Anatomy and Physiology of the Respiratory System
| Meaning | Combining Form |
| adenoid | adenoid/o |
| air | pneum/o, aer/o |
| alveolus | alveol/o |
| base | bas/o |
| bronchiole | bronchiol/o |
| bronchus | bronch/o, bronchi/o |
| carbon dioxide | capn/o |
| chest | steth/o, thorac/o, pector/o |
| diaphragm | diaphragm/o, diaphragmat/o, phren/o |
| epiglottis | epiglott/o |
| eustachian tube | salping/o |
| larynx (voicebox) | laryng/o |
| lobe | lob/o, lobul/o |
| lung | pulmon/o, pneumon/o, pneum/o |
| mediastinum | mediastin/o |
| mouth | or/o, stomat/o |
| mucus | muc/o |
| nose | nas/o, rhin/o |
| oxygen | ox/i, ox/o |
| pharynx (throat) | pharyng/o |
| pleura | pleur/o |
| point, tip, apex | apic/o |
| rib | cost/o |
| septum, wall | sept/o, pariet/o |
| sinus | sinus/o, sin/o |
| sound | phon/o |
| to breathe | spir/o, hal/o |
| tongue | lingu/o |
| tonsil | tonsill/o |
| trachea (windpipe) | trache/o |
| viscera | viscer/o |
Prefixes for Anatomy and Physiology of the Respiratory System
| Prefix | Meaning |
| ex- | out |
| in- | in |
| inter- | between |
| oxy- | oxygen |
| para- | near |
| re- | again |
Pathology

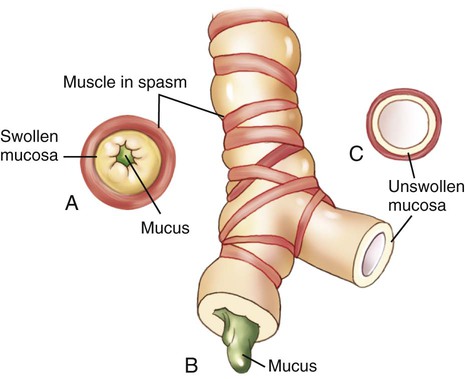
A, Cross section of a bronchiole occluded by muscle spasm, swollen mucosa, and mucus. B, Longitudinal section of an obstructed bronchiole. C, Cross-section of a clear bronchiole.
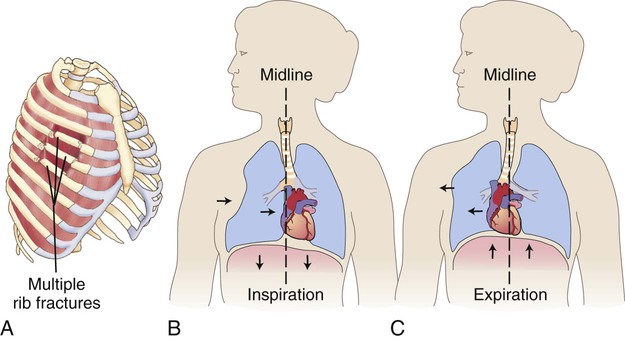
A, Fractured rib sections are unattached to the rest of the chest wall. B, On inspiration, the flail segment of ribs is sucked inward, causing the lung to shift inward. C, On expiration, the flail segment of ribs bellows outward, causing the lung to shift outward. Air moves back and forth between the lungs instead of through the upper airway.
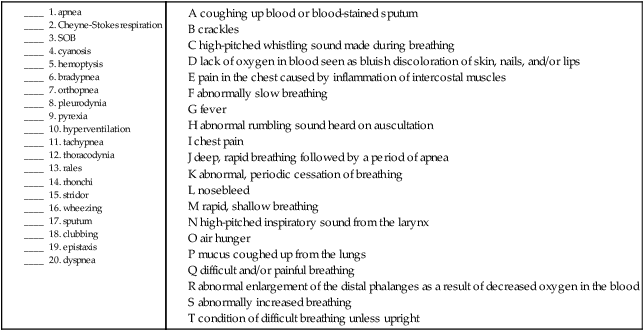
Terms Related to Symptoms and Signs Involving the Respiratory System (RØØ-R99)
| Term | Word Origin | Definition |
| aphonia | a- no, not, without phon/o sound -ia condition |
Loss of ability to produce sounds. Dysphonia is difficulty making sounds. |
| apnea | a- no, not, without -pnea breathing |
Abnormal, periodic cessation of breathing. |
| bradypnea | brady- slow -pnea breathing |
Abnormally slow breathing. |
| Cheyne-Stokes respiration | Deep, rapid breathing followed by a period of apnea. | |
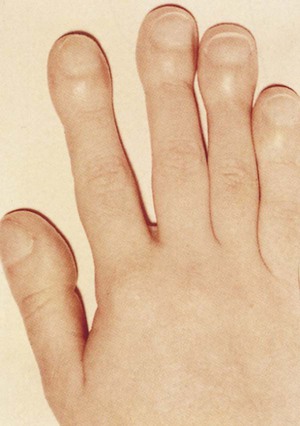
| clubbing | Abnormal enlargement of the distal phalanges as a result of diminished O2 in the blood (Fig. 10-5). | |
| cyanosis | cyan/o blue -osis abnormal condition |
Lack of oxygen in blood seen as bluish or grayish discoloration of the skin, nail beds, and/or lips. |
| dyspnea | dys- difficult -pnea breathing |
Difficult and/or painful breathing. DOE is dyspnea on exertion. Eupnea is good, normal breathing. (Eu- means healthy, normal). |
| epistaxis | Nosebleed. Also called rhinorrhagia. | |
| hemoptysis | hem/o blood -ptysis spitting |
Coughing up blood or blood-stained sputum. |
| hypercapnia | hyper- excessive capn/o carbon dioxide -ia condition |
Condition of excessive CO2 in the blood. |
| hyperpnea | hyper- excessive -pnea breathing |
Excessively deep breathing. Hypopnea is extremely shallow breathing. |
| hyperventilation | hyper- excessive | Abnormally increased breathing. |
| hypoxemia | hypo- deficient ox/o oxygen -emia blood condition |
Condition of deficient O2 in the blood. Hypoxia is the condition of deficient oxygen in the tissues. |
| orthopnea | orth/o straight -pnea breathing |
Condition of difficult breathing unless in an upright position (Fig. 10-6). |
| pleurodynia | pleur/o pleura -dynia pain |
Pain in the chest caused by inflammation of the intercostal muscles. |
| pyrexia | pyr/o fire -exia condition |
Fever. |
| shortness of breath (SOB) | Breathlessness; air hunger. | |
| sputum, abnormal | Mucus coughed up from the lungs and expectorated through the mouth. If abnormal, may be described as to its amount, color, or odor. | |
| tachypnea | tachy- fast -pnea breathing |
Rapid, shallow breathing. |
| thoracodynia | thorac/o chest -dynia pain |
Chest pain. |
Terms Related to Abnormal Breath Sounds (RØ6-RØ9)
| An important part of the diagnostic process is the evaluation of breath sounds, usually through the use of a stethoscope. This “listening” is termed auscultation, and the “tapping” is called percussion. Normal breath sounds are termed vesicular, misnamed by the inventor of the stethoscope, Laennec. He interpreted the sound as originating from the tiny sacs of the alveoli, instead of the trachea and bronchi, where they actually occur. Abnormal breath sounds are collectively referred to as adventitious sounds. | ||
| Term | Word Origin | Definition |
| friction sounds | Sounds made by dry surfaces rubbing together. Characteristic of inflamed pleurae; may also have a grating or creaking sound. | |
| hiccough | Sound produced by the involuntary contraction of the diaphragm, followed by rapid closure of the glottis. Also called hiccup, singultus. | |
| rales | Also called crackles or crepitations, an abnormal lung sound heard on inspiration, characterized by discontinuous bubbling, clicking, or rattling noises. May be associated with pneumonia or congestive heart failure and are characterized as moist, dry, fine, and/or coarse. | |
| rhonchi | If used as a term without further description (see wheezes), rhonchi are continuous abnormal rumbling sounds heard on expiration, caused by airways blocked with secretions. | |
| stridor | Continuous, high-pitched inspiratory sound from the larynx; a sign of upper airway obstruction or epiglottitis. | |
| wheezing | Continuous sounds heard during inspiration and/or expiration. If high pitched and having a whistling sound (as in an asthma attack), they may also be referred to as sibilant rhonchi. Sonorous rhonchi are those wheezes that are lower in pitch and having a snoring or rumbling sound (as in bronchitis). The sibilant rhonchi are caused by airways narrowed from constriction or swelling, while the sonorous rhonchi are caused by secretions in the bronchi. | |
21. condition of excessive carbon dioxide ____________________________________________________________
22. blood condition of deficient oxygen _____________________________________________________________
23. condition of without sound _____________________________________________________________________
24. chest pain _____________________________________________________________________________________
25. fast breathing __________________________________________________________________________________
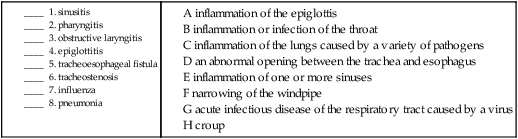
Terms Related to Congenital Disorders (QØØ-Q99)
| Term | Word Origin | Definition |
| tracheoesophageal fistula | trache/o trachea, windpipe esophag/o esophagus -eal pertaining to |
A congenital abnormal opening between the trachea and the esophagus. Can be acquired. |
| tracheomalacia | trache/o trachea, windpipe -malacia softening |
Congenital softening of the tissues of the trachea. Can also result from chronic ventilator use. |
| tracheostenosis | trache/o trachea, windpipe -stenosis narrowing |
Congenital narrowing of the windpipe. Can be acquired. |
Terms Related to Acute Upper Respiratory Infections (JØØ-JØ6)
| Term | Word Origin | Definition |
| epiglottitis | epiglott/o epiglottis -itis inflammation |
Inflammation of the epiglottis (Fig. 10-7). Supraglottitis is an inflammation of the area immediately above the glottis that includes the epiglottis. |
| laryngitis | laryng/o larynx, voicebox -itis inflammation |
Inflammation of the voice box. |
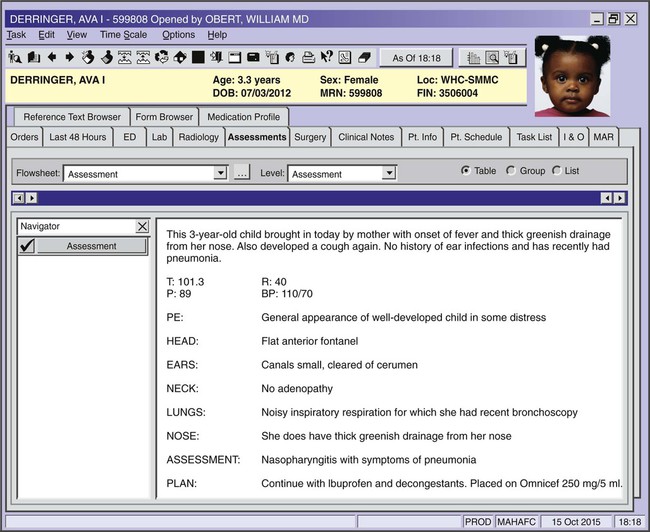
| nasopharyngitis | nas/o nose pharyng/o pharynx, throat -itis inflammation |
The common cold. Also referred to as coryza. |
| obstructive laryngitis | Acute viral infection of early childhood, marked by stridor caused by spasms of the larynx, trachea, and bronchi. Also called croup. | |
| pharyngitis | pharyng/o pharynx, throat -itis inflammation |
Inflammation or infection of the pharynx, usually causing symptoms of a sore throat. |
| sinusitis | sinus/o sinus -itis inflammation |
Inflammation of one or more of the paranasal sinuses. Pansinusitis refers to an inflammation of all of the sinuses (pan- means all). |
| tracheitis | trache/o trachea, windpipe -itis inflammation |
Inflammation of the windpipe. |
Terms Related to Influenza and Pneumonia (JØ9-J18)
| Term | Word Origin | Definition |
| influenza | Also known as the flu. Acute infectious disease of the respiratory tract caused by a virus. Avian (bird) flu is caused by type A influenza virus. The latest bird flu is caused by H7N9 virus. Swine flu is caused by H1N1 virus. | |
| pneumonia | pneumon/o lung -ia condition |
Inflammation of the lungs caused by a variety of pathogens. If infectious, it is termed pneumonia; if noninfectious, pneumonitis. The name(s) of the lobes are used to describe the extent of the disease (e.g., RUL pneumonia is pneumonia of the right upper lobe) (Fig. 10-8). If both lungs are affected, it is termed double pneumonia. |
| severe acute respiratory syndrome (SARS) | syn- together, with -drome to run |
Viral respiratory disorder caused by a coronavirus. Usually results in pneumonia. |
Terms Related to Other Acute Lower Respiratory Infections (J2Ø-J22)
| Term | Word Origin | Definition |
| bronchiolitis | bronchiol/o bronchiole -itis inflammation |
Viral inflammation of the bronchioles; more common in children younger than 18 months. |
| bronchitis | bronch/o bronchus -itis inflammation |
Inflammation of the bronchi. May be acute or chronic. |
9. nasolaryngitis __________________________________________________________________________________
10. tracheitis _______________________________________________________________________________________
11. tracheomalacia _________________________________________________________________________________
12. bronchiolitis ___________________________________________________________________________________
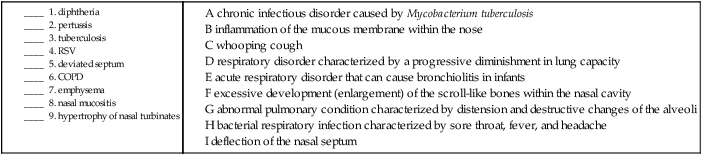
Terms Related to Other Diseases of Upper Respiratory Tract (J3Ø-J39)
| Term | Word Origin | Definition |
| deviated septum | sept/o wall, septum -um structure |
Deflection of the nasal septum that may obstruct the nasal passages, resulting in infection, sinusitis, shortness of breath, headache, or recurring epistaxis. |
| hypertrophy of nasal turbinates | hyper- excessive -trophy development |
Excessive development (enlargement) of the scroll-like bones within the nasal cavity. |
| laryngismus | laryng/o larynx, voicebox -ismus spasm condition |
A spasm of the larynx. Also called stridulus. |
| nasal mucositis (ulcerative) | mucos/o mucus -itis inflammation |
Inflammation of the mucous membrane within the nose. Ulcerative indicates that there is erosion of the mucous membrane. |
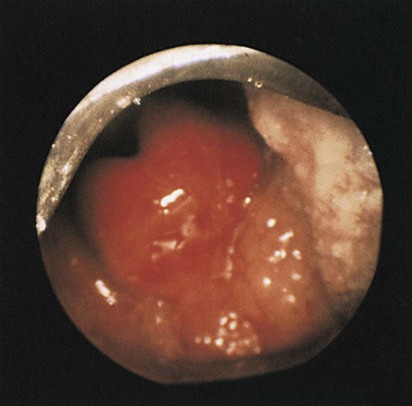
| polyps, nasal and vocal cord | Small, tumorlike growths that project from a mucous membrane surface, including the inside of the nose, the paranasal sinuses, and the vocal cords (Fig. 10-9). | |
| rhinorrhea | rhin/o nose -rrhea discharge, flow |
Discharge from the nose. |
Terms Related to Specific Infections of the Respiratory System (A15-B97)
| Term | Word Origin | Definition |
| diphtheria | Bacterial respiratory infection characterized by a sore throat, fever, and headache. | |
| pertussis | Bacterial infection of the respiratory tract with a characteristic high-pitched “whoop.” Also called whooping cough. | |
| respiratory syncytial virus (RSV) | Acute respiratory disorder usually occurring in the lower respiratory tract in children and the upper respiratory tract in adults. Most common cause of bronchiolitis and pneumonia in infants and highly contagious in young children. | |
| rhinomycosis | rhin/o nose myc/o fungus -osis abnormal condition |
Abnormal condition of fungus in the nose. |
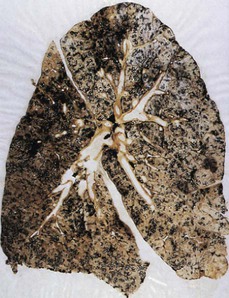
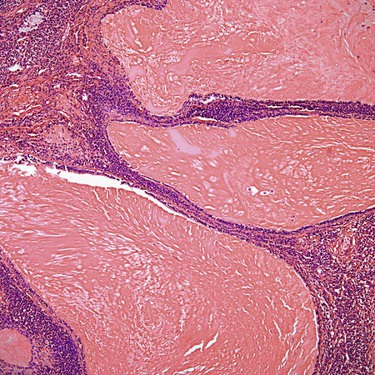
| tuberculosis (TB) | Chronic infectious disorder caused by an acid-fast bacillus, Mycobacterium tuberculosis (Fig. 10-10). Transmission is normally by inhalation or ingestion of infected droplets. Multidrug-resistant tuberculosis (MDR TB) is fatal in 80% of cases. |
Terms Related to Chronic Lower Respiratory Diseases (J4Ø-J47)
| Term | Word Origin | Definition |
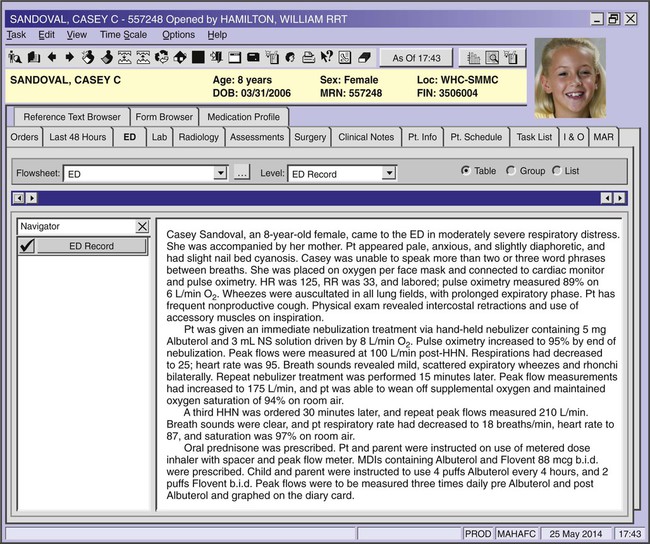
| asthma | Respiratory disorder characterized by recurring episodes of paroxysmal (sudden, episodic) dyspnea. Patients exhibit coughing, wheezing, and shortness of breath. If the attack becomes continuous (termed status asthmaticus), it may be fatal (Fig. 10-11). If described as extrinsic, the cause is from an allergic reaction to an inhaled substance. If intrinsic, the cause is unknown (idiopathic). Intermittent asthma is less than 2x a week, while persistent asthma is more than 2x per week. | |
| bronchiectasis | bronchi/o bronchus -ectasis dilation |
Chronic dilation of the bronchi. Symptoms include dyspnea, expectoration of foul-smelling sputum, and coughing. |
| chronic obstructive pulmonary disease (COPD) | pulmon/o lung -ary pertaining to |
Respiratory disorder characterized by a progressive and irreversible diminishment in inspiratory and expiratory capacity of the lungs. Patient experiences dyspnea on exertion (DOE), difficulty inhaling or exhaling, and a chronic cough. |
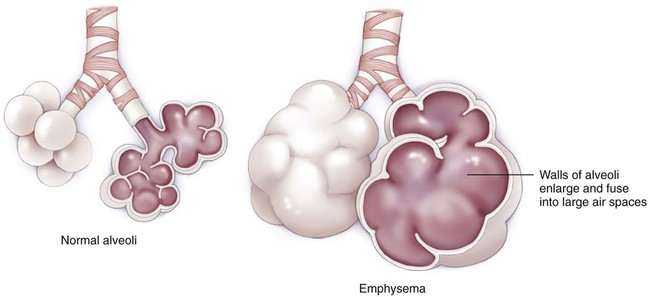
| emphysema (including panlobular) | Abnormal condition of the pulmonary system characterized by distension and destructive changes of the alveoli. The most common cause is tobacco smoking, but exposure to environmental particulate matter may also cause the disease (Fig. 10-12). |
Terms Related to Lung Disease Due to External Agents (J6Ø-J7Ø)
| Term | Word Origin | Definition |
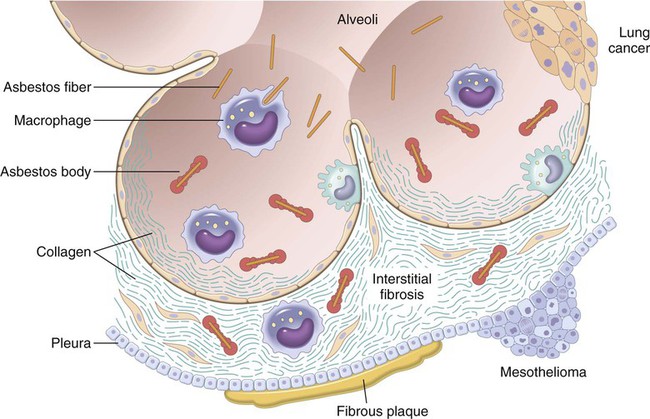
| pneumoconiosis | pneum/o lung coni/o dust -osis abnormal condition |
Loss of lung capacity caused by an accumulation of dust in the lungs. Types may include asbestosis (abnormal condition of asbestos in the lungs) (Fig. 10-13), silicosis (abnormal accumulation of glass dust in the lungs), and coal workers’ pneumoconiosis (CWP) (Fig. 10-14). |
10. spasm of the larynx _____________________________________________________________________________
11. abnormal condition of fungus in the nose ________________________________________________________
12. dilation of the bronchus _________________________________________________________________________
13. abnormal condition of dust in the lung __________________________________________________________
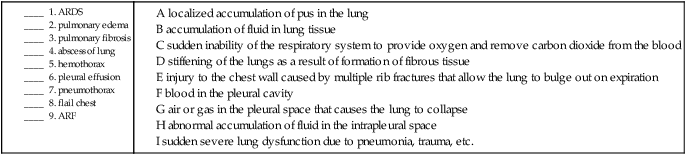
Terms Related to Other Respiratory Diseases Principally Affecting the Interstitium (J8Ø-J84)
| Term | Word Origin | Definition |
| acute respiratory distress syndrome (ARDS) | Sudden, severe lung dysfunction due to a number of different disorders (e.g., pneumonia, trauma). Patients have extreme difficulty with breathing and may need mechanical ventilation. | |
| pulmonary edema | pulmon/o lung -ary pertaining to |
Accumulation of fluid in the lung tissue. Often present in congestive heart failure, it is caused by the inability of the heart to pump blood. |
| pulmonary fibrosis | fibr/o fiber -osis abnormal condition |
A stiffening of the lungs as a result of the formation of fibrous tissue. Idiopathic in origin. |
Terms Related to Suppurative and Necrotic Conditions of the Lower Respiratory Tract (J85-J86)
| Term | Word Origin | Definition |
| abscess of lung | Localized accumulation of pus in the lung. | |
| pyothorax | py/o pus -thorax chest (pleural cavity) |
Pus in the pleural cavity. Also called empyema. |
Terms Related to Other Diseases of the Pleura (J9Ø-J94)
| Term | Word Origin | Definition |
| hemothorax | hem/o blood -thorax chest (pleural cavity) |
Blood in the pleural cavity (Fig. 10-15). |
| hydrothorax | hydr/o water -thorax chest (pleural cavity) |
An accumulation of serous fluid in the pleural cavity. |
| pleural effusion | pleur/o pleura -al pertaining to |
Abnormal accumulation of fluid in the intrapleural space. |
| pneumothorax | pneum/o air -thorax chest (pleural cavity) |
Air or gas in the pleural space causing the lung to collapse (Fig. 10-16). |
Terms Related to Other Diseases of the Respiratory System (J96-J99)
| Term | Word Origin | Definition |
| acute respiratory failure (ARF) | A sudden inability of the respiratory system to provide oxygen and/or remove CO2 from the blood. May be caused by cardiac or pulmonary dysfunction or drug intoxication. | |
| atelectasis | a- not tel/e complete -ectasis dilation |
Collapse of lung tissue or an entire lung. |
| bronchospasm | bronch/o bronchus -spasm sudden, involuntary contraction |
A sudden involuntary contraction of the bronchi, as in an asthma attack. |
Terms Related to Injuries to the Thorax (S2Ø-S29)
| Term | Word Origin | Definition |
| flail chest | A condition in which multiple rib fractures cause instability in part of the chest wall and in which the lung under the injured area contracts on inspiration and bulges out on expiration (Fig. 10-17). |
10. bronchospasm __________________________________________________________________________________
11. atelectasis ______________________________________________________________________________________
12. pyothorax ______________________________________________________________________________________
13. hydrothorax ____________________________________________________________________________________
Respiratory Neoplasms
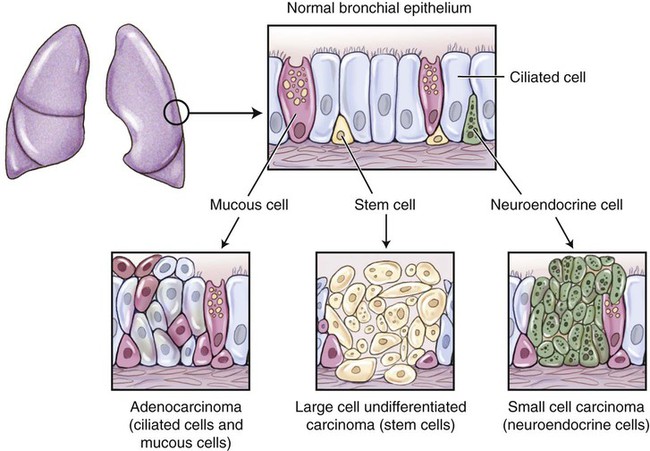
Because organs are composed of tissues and tissues are constructed from a variety of cell types, cancer of an organ can occur in a number of different varieties, depending on which types of cells mutate. Figure 10-18 shows the three main categories of lung cancer along with the types of cells from which they originate.
Terms Related to Benign Neoplasms
| Term | Word Origin | Definition |
| mucous gland adenoma | muc/o mucus -ous pertaining to aden/o gland -oma tumor, mass |
A benign tumor of the mucous glands of the respiratory system (Fig. 10-19). |
| papilloma | papill/o nipple -oma tumor, mass |
A benign tumor of epithelial origin named for its nipplelike appearance. |
Terms Related to Malignant Neoplasms
| Term | Word Origin | Definition |
| mesothelioma | -oma tumor, mass | A rare malignancy of the pleura or other protective tissues that cover the internal organs of the body. Often caused by exposure to asbestos (Fig. 10-20). |
| non–small cell lung cancer (NSCLC) | Group of cancers that arise from cells that line the bronchi (squamous and adenocarcinoma) or are on or near the surface of the lung (large cell). | |
| adenocarcinoma | aden/o gland -carcinoma cancer of epithelial origin |
NSCLC derived from the mucus-secreting glands in the lungs (see Fig. 10-18). |
| large cell carcinoma | carcinoma cancer of epithelial origin | NSCLC originating in the lining of the smaller bronchi (see Fig. 10-18). |
| squamous cell carcinoma | squam/o scaly -ous pertaining to carcinoma cancer of epithelial origin |
NSCLC originating in the squamous epithelium of the larger bronchi. |
| small cell lung cancer (carcinoma) (SCLC) | carcinoma cancer of epithelial origin | Second most common type of lung cancer. Associated with smoking. Derived from neuroendocrine cells in the bronchi (see Fig. 10-18). Also called oat cell carcinoma. |
Procedures

A, Simple face mask. B, Venturi mask. C, Nasal cannula. D, CPAP.
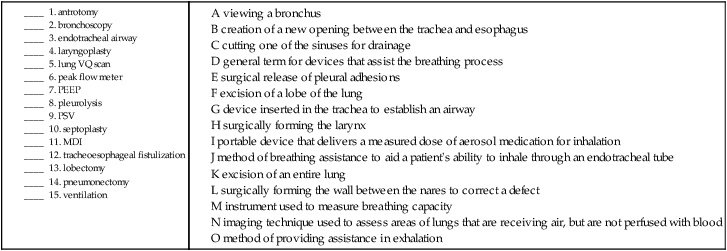
| Term | Word Origin | Definition |
| arterial blood gases (ABG) | arteri/o artery -al pertaining to |
Blood test that measures the amount of oxygen and carbon dioxide in the blood. |
| adenoidectomy | adenoid/o adenoid -ectomy cutting out |
Removal of the adenoids. Also called the pharyngeal tonsils. |
| antrotomy | antr/o antrum -tomy cutting |
Cutting one of the sinuses for the purpose of drainage. Also called sinusotomy. |
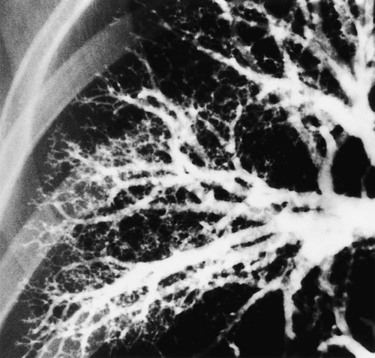
| bronchography | bronch/o bronchus -graphy recording |
Recording the bronchi through imaging techniques using a contrast medium (Fig. 10-21). |
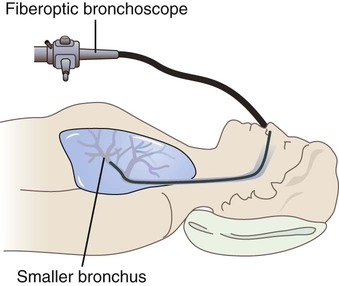
| bronchoscopy | bronch/o bronchus -scopy viewing |
Viewing a bronchus using an instrument (Fig. 10-22). |
| endotracheal airway | endo- within trache/o trachea, windpipe -al pertaining to |
A device that is positioned in the trachea for the purposes of establishing an airway. |
| ethmoidectomy | ethmoid/o ethmoid -ectomy cutting out |
Cutting out part or all of the ethmoid bone. Usually done to treat a chronic sinus infection. |
| laryngoplasty | laryng/o larynx, voicebox -plasty surgically forming |
Surgically forming the larynx for the purpose of improving the voice for patients with hoarseness. |
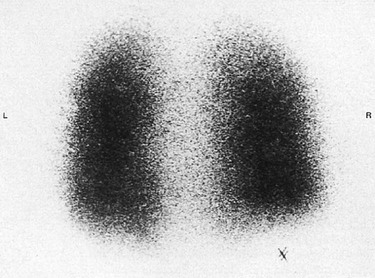
| lung VQ scan | An imaging technique used to assess the areas of the lungs that are receiving air, but are not perfused with blood, possibly as a result of a blood clot (Fig. 10-23). | |
| Mantoux skin test | Intradermal injection of purified protein derivative (PPD) used to detect the presence of tuberculosis antibodies. | |
| metered dose inhaler (MDI) | A portable device that delivers a measured dose of an aerosol medication for inhalation. An additional device, a spacer, is an add-on chamber that holds the dispensed dose of medication, allowing the user to inhale it more slowly. | |
| nebulizer | A battery- or electric-powered device/machine used to turn a liquid medication into a fine mist for inhalation through a mouthpiece or facemask. A hand-held nebulizer (HHN) is the portable form. | |
| peak flow meter | Instrument used in a pulmonary function test (PFT) to measure breathing capacity (Fig. 10-24). | |
| plain radiography, chest (CXR) | radi/o rays -graphy recording |
One of the most common imaging techniques; used to visualize abnormalities of the respiratory system (Fig. 10-25). X-rays may also include the use of a contrast medium, as in a pulmonary angiography, which uses a dye injected into the blood vessels of the lung, followed by subsequent x-ray imaging to demonstrate the flow of blood through these vessels. |
| pleurocentesis | pleur/o pleura -centesis surgical puncture |
Surgical puncture to remove fluid or air from the pleural cavity. |
| pleurodesis | pleur/o pleura -desis fixation |
The mechanical fixation of the two pleural membranes in order to prevent pleural effusions. If the fixation is done chemically, it is called pleurosclerosis. |
| pleurolysis | pleur/o pleura -lysis breaking down |
The surgical separation of pleural adhesions through the use of an endoscope and electrical cauterization. The adhesions are often caused by scarring from repeated pleural inflammation. |
| positive end expiratory pressure (PEEP) | A method of providing assistance in exhalation through the use of an endotracheal tube, a tracheostomy, a face mask, or nasal prongs. | |
| positive support ventilation (PSV) | A method of breathing assistance to increase a patient’s ability to inhale through an endotracheal tube. | |
| pulmonary function tests (PFTs) | pulmon/o lung -ary pertaining to |
Procedures for determining the capacity of the lungs to exchange O2 and CO2 efficiently. See the table on the following page for examples of PFTs. |
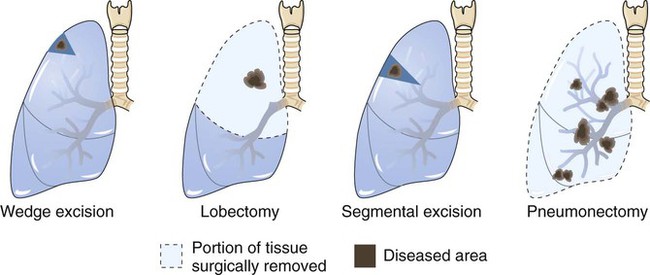
| pulmonary resections and excisions | Excision of a segment or a lobe of the lung or the entire lung. Called a lobectomy when an entire lobe is resected and a pneumonectomy when the entire lung is resected (Fig. 10-26). | |
| pulse oximetry | ox/i oxygen -metry measuring |
Measuring the oxygen level of the blood using a pulse oximeter. A noninvasive, cliplike device is attached to either the ear lobe or fingertip (Fig. 10-27). |
| quantiferon-TB gold test (QFT) | Definitive blood test used to diagnose tuberculosis. |
Examples of Pulmonary Function Tests
| Function | Abbreviation | Description |
| Forced expiratory volume | FEV | Amount of air that can be exhaled with force in one breath. |
| Forced residual capacity | FRC | Amount of air remaining after a normal exhalation. |
| Forced vital capacity | FVC | Amount of air that can be exhaled with force after one inhales as deeply as possible. |
| Inspiratory capacity | IC | Amount of air that can be inspired after a normal expiration. |
| Tidal volume | TV | Amount of air normally inspired and expired in one respiration. |
| Total lung capacity | TLC | Amount of air in the lungs after one inhales as deeply as possible. |
Terms Related to Procedures—cont’d
| Term | Word Origin | Definition |
| rhinoplasty | rhin/o nose -plasty surgically forming |
Surgically forming by correcting, altering, supplementing, or replacing the nose. |
| septoplasty | sept/o septum, wall -plasty surgically forming |
Surgically straightening the wall between the nares to correct a deviation. |
| spirometry | spir/o to breathe –metry measuring |
Test to measure the air capacity of the lungs. A spirometer is an instrument to measure breathing. |
| sputum culture and sensitivity | Cultivation of microorganisms from sputum that has been collected from expectoration (spitting). | |
| tracheoesophageal fistulization (TEF) | trache/o trachea, windpipe esophag/o esophagus -eal pertaining to |
The creation of a new opening between the trachea and the esophagus after a laryngectomy to preserve the ability to speak. |
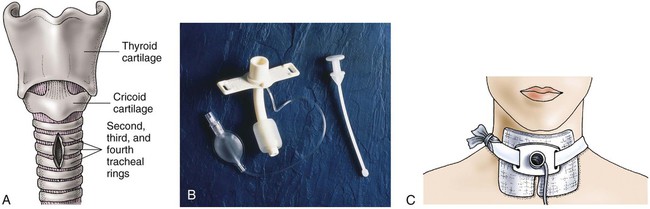
| tracheostomy | trache/o trachea, windpipe -stomy making a new opening |
New opening of the trachea. A tracheostomy device is an instrument used to facilitate the maintenance of an opening in the trachea (Fig. 10-28). |
| tracheotomy | trache/o trachea, windpipe -tomy cutting |
Cutting the trachea to establish an airway. |
| turbinectomy | turbin/o turbinate bone -ectomy cutting out |
Cutting out part or all of a turbinate bone, usually the inferior turbinate, to allow for greater air flow. |
| ventilation | A general term for devices that assist the breathing process. Patients who need assistance in attaining adequate O2 levels may need a mechanical device called a ventilator to provide positive-pressure breathing. The device delivers the O2 in different ways. If a low level of O2 is required, a nasal cannula (tube) may be adequate. Face masks are another option. The amount of O2 may be monitored more accurately with a Venturi mask. If high O2 concentrations are necessary, a nonrebreathing or partial rebreathing mask may be used. Positive-pressure breathing (PPB) is a respiratory therapy technique designed to deliver air at greater than atmospheric pressure to the lungs. Continuous positive airway pressure (CPAP) may be delivered through a ventilator and endotracheal tube or a nasal cannula, face mask, or hood over the patient’s head. Figure. 10-29 presents several examples of oxygenation therapy. |
16. recording the bronchi ___________________________________________________________________________
17. cutting out the ethmoid bone ___________________________________________________________________
18. fixation of the pleura ____________________________________________________________________________
19. making a new opening of the trachea ____________________________________________________________
20. cutting out a turbinate __________________________________________________________________________
21. surgically forming the nose _____________________________________________________________________
22. surgical puncture of the pleura __________________________________________________________________
Pharmacology
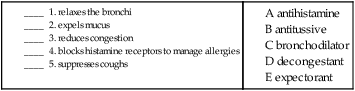
antihistamines: Block histamine receptors to manage allergies associated with allergic rhinitis or allergy-induced asthma. Examples are clemastine (Tavist), diphenhydramine (Benadryl), loratadine (Claritin), and fexofenadine (Allegra).
antitussives: Suppress the cough reflex. Examples include dextromethorphan (Delsym), codeine (Robitussin AC), and benzonatate (Tessalon).
bronchodilators: Relax bronchi to improve ventilation to the lungs. Examples include theophylline (Theo-Dur), ipratropium (Atrovent), and albuterol (Proventil, Ventolin), often administered through inhalers or nebulizers.
decongestants: Reduce congestion or swelling of mucous membranes. Examples are pseudoephedrine (Sudafed) and phenylephrine (Sudafed PE).
expectorants: Promote the expulsion of mucus from the respiratory tract. An example is guaifenesin (Mucinex).
inhaled corticosteroids: Reduce airway inflammation to improve ventilation or reduce nasal congestion. Administered via oral or nasal inhalation accordingly. Examples include fluticasone (Flovent, Flonase), mometasone (Nasonex), and beclomethasone (Qvar).
mucolytics: Break up thick mucus in the respiratory tract. An example is N-acetyl-cysteine (Mucomyst).
6. What type of mechanical device is used to produce a fine spray for inhaled medications?
_________________________________________________________________________________________________
7. What type of nonmechanical device is used to administer medications that are inhaled, such as fine powders or vapors? _____________________________________________________________________________
8. A/An ____________________ is a device designed to assist in respiration and intensive positive-pressure breathing.
Recognizing Suffixes for PCS
Suffixes and Root Operations for the Respiratory System
| Suffix | Root Operation |
| -centesis | Drainage |
| -ectomy | Excision, resection |
| -lysis | Release |
| -plasty | Alteration, reposition, repair, replacement, supplement |
| -rrhaphy | Repair |
| -tomy | Drainage |
| Abbreviation | Meaning |
| ABG | arterial blood gases |
| ARDS | acute respiratory distress syndrome |
| ARF | acute respiratory failure |
| CO2 | carbon dioxide |
| COPD | chronic obstructive pulmonary disease |
| CPAP | continuous positive airway pressure |
| CWP | coal workers’ pneumoconiosis |
| CXR | chest x-ray |
| DOE | dyspnea on exertion |
| HHN | hand-held nebulizer |
| LLL | left lower lobe |
| LUL | left upper lobe |
| MDI | metered dose inhaler |
| MDR TB | multidrug-resistant tuberculosis |
| NSCLC | non–small cell lung cancer |
| O2 | oxygen |
| PEEP | positive end expiratory pressure |
| PFT | pulmonary function test |
| PSV | positive support ventilation |
| QFT | quantiferon—TB gold test |
| RLL | right lower lobe |
| RML | right middle lobe |
| RSV | respiratory syncytial virus |
| RUL | right upper lobe |
| SARS | severe acute respiratory syndrome |
| SCLC | small cell lung cancer |
| SOB | shortness of breath |
| TB | tuberculosis |
| TEF | tracheoesophageal fistula |