Chapter 8 Respiratory emergencies
the acutely breathless patient
GENERAL PRINCIPLES
Exclude airway compromise, which may be subtle, as the cause of acute breathlessness. Management of airway problems always comes first. Dyspnoea is a sensation which has multiple aetiologies and can be difficult to assess.
Initial goals in assessment and management are:
OXYGEN THERAPY
Delivery of oxygen is one of the most common therapies in the emergency department and an important component of resuscitation. Acute hypoxaemia is immediately life-threatening and the ‘first-line drug’ for hypoxaemia is oxygen! It is a safe drug: the complications of oxygen therapy are concentration- and time-dependent, uncommon and take time to develop. Other aspects of oxygen delivery may also need to be improved in the hypoxaemic patient, especially cardiac output, haemoglobin, tissue perfusion and reducing tissue O2 requirements.
| SaO2 (%) | PaO2 (mmHg) | Level |
|---|---|---|
| 98 | 100 | Arterial blood |
| 90 | 60 | |
| 75 | 40 | Venous blood |
| 50 | 26 | |
| ∼33 | ∼20 | Tissue |
SaO2, oxygen saturation; PaO2, partial pressure of oxygen in arterial or venous blood or tissue
Note: When SaO2 ≈ 60–90%, there is a linear relationship between SaO2 and PaO2.
Oxygen delivery systems
Simple delivery systems
These are variable performance systems—the FiO2 delivered not only depends upon the oxygen flow rate, but also on the rate and depth of respiration. The FiO2 delivered by various systems can be estimated (Table 8.2).
Table 8.2 Estimation of the fraction of inspired oxygen (FiO2) achieved by simple delivery systems
| Flow rate (L/min) | FiO2 |
|---|---|
| 2 (nasal prongs) | 0.25 |
| 3 (nasal prongs) | 0.28 |
| 4 (nasal prongs) | 0.30 |
| 6 | 0.40 |
| 8 | 0.45 |
| 15 | 0.65 |
| 15 (reservoir mask)∗ | 0.70 |
∗ If a double wall supply is used, a flow rate of 30 L/min and FiO2 up to 0.90 can be achieved.
Partial rebreathing systems
Anaesthetic circuits. Mentioned for completeness; rarely used in the emergency department setting.
INVESTIGATIONS IN RESPIRATORY EMERGENCIES
Arterial blood gases: oxygenation and ventilation
Arterial blood gases (ABGs) reflect oxygenation (PaO2), ventilation (PaCO2) and acid–base status. The last is dealt with in more detail in Chapter 27, ‘Metabolic disorders’.
Oxygenation
Remember that, even for ‘normal’ lungs, the PaO2 varies with the following parameters.
pH. For each 0.1 decrease (or increase) in pH, the PaO2 will increase (or decrease) by ∼ 10%.
The gradient varies with age: add 3 for each decade over the age of 30 years.
The PAO2 can also be quickly estimated using one of the following rules of thumb:
Ventilation
The clinical effects of hypercarbia
Respiratory drive will typically be increased, unless it is suppressed due to the underlying cause of the hypercarbia (e.g. CNS disorders, narcotics). There is a rise in endogenous catecholamines leading to tachycardia, hypertension, increased CO, increased cerebral blood flow and raised intracranial pressure (ICP). Peripheral vasodilatation typically occurs. The patient initially becomes anxious and restless, followed by a decreased level of consciousness and eventually coma if it remains uncorrected.
Other investigations in respiratory emergencies
The chest X-ray
The chest X-ray (CXR) is one of the most useful investigations in the patient with respiratory failure. In order to interpret the film correctly, and to avoid missing important findings, a good routine for assessing the CXR is a must. The principles of chest radiography, and other chest imaging modalities, are dealt with in more detail in Chapter 4, ‘Diagnostic imaging in emergency patients’.
Tests of forced expiration
Peak expiratory flow rate (PEFR) is measurable using a simple, portable flow meter. It is reproducible by most patients after several practice efforts. PEFR may be reduced in COPD, asthma and respiratory muscle weakness. PEFR may be normal or increased in restrictive lung diseases such as fibrosis. It is perhaps most useful as a monitor for asthmatic patients in the outpatient/home setting. It may also be helpful in the emergency department as one of the means to assess discharge suitability of asthmatic patients (e.g. PEFR should be at least 75% of predicted or best).
Invasive respiratory investigations
Invasive techniques such as percutaneous needle biopsy, diagnostic bronchoscopy, transbronchial biopsy and bronchoalveolar lavage are rarely undertaken in Australasian emergency departments. An exception is diagnostic and/or therapeutic thoracentesis. Pleural fluid is normally a pale yellow colour. It is turbid in the setting of empyema or parapneumonic effusion. Blood in pleural fluid may be due to trauma, malignancy or pulmonary infarction. Other common analyses of pleural fluid include: protein (pleural fluid protein < 30 g/L represents a transudate; > 30 g/L represents an exudate); lactate dehydrogenase (LDH) (pleural fluid:serum LDH ratio < 0.6 represents a transudate; > 0.6 represents an exudate); white cell count (leukocytes may be due to a parapneumonic effusion, pulmonary embolus or empyema; lymphocytes may be due to tuberculosis, malignancy or a vasculitis); glucose (pleural fluid glucose may be < 50% serum glucose levels in bacterial infections, malignancy, rheumatoid arthritis and systemic lupus erythematosus (SLE)); cytology (malignant cells, mesothelial cells); and culture.
LIFE-THREATENING CONDITIONS PRESENTING WITH BREATHLESSNESS
Acute asthma
Initial management
Assess severity
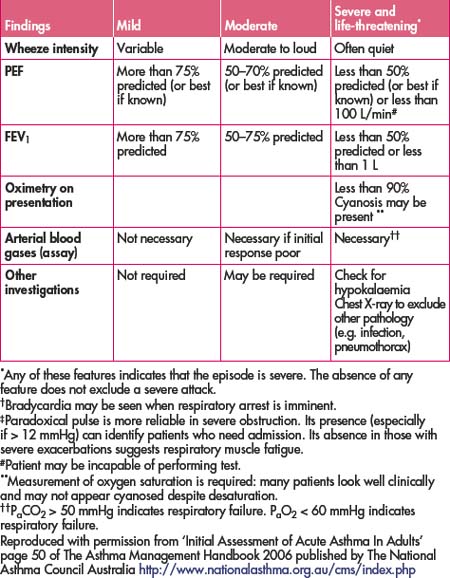
Assess severity as mild, moderate or severe and life-threatening using signs of physical exhaustion, cyanosis, speech, PEFR, spirometry (the most accurate test, but may not be possible initially), oxygen saturation, heart rate, respiratory rate and pulsus paradoxus (abnormal decrease in blood pressure on inspiration). Refer to Table 8.3.
Features of severe and life-threatening asthma include: paradoxical chest wall movement, exhaustion, sweating, vomiting, panic, speaking in short phases or words only, pulse rate > 120/min, pulsus paradoxus >12 mmHg, central cyanosis, quiet, NOT wheezy chest, PEFR < 50% predicted or < 100 L/min, FEV1 < 50% predicted or < 1 L, pulse oximetry < 90%.
Also observe carefully the patient who has childhood onset of asthma, is steroid dependent, has previously been intubated or has a history of severe episodes, especially requiring ICU admission, as they are at increased risk.
Further treatment
Assess response to therapy
Acute exacerbation of COPD
Patients with COPD, because of their marginal lung function at diagnosis, are prone to significant symptoms with minor precipitants. The precipitant may include acute infection (most commonly), small pneumothoraces, deteriorations in cardiac performance and arrhythmias and may be complicated by acute anxiety and increasing O2 consumption.
Initial stabilisation
Further treatment
Pneumonia
Management
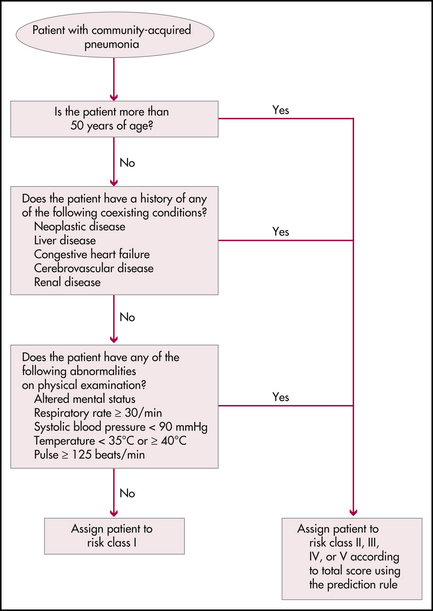
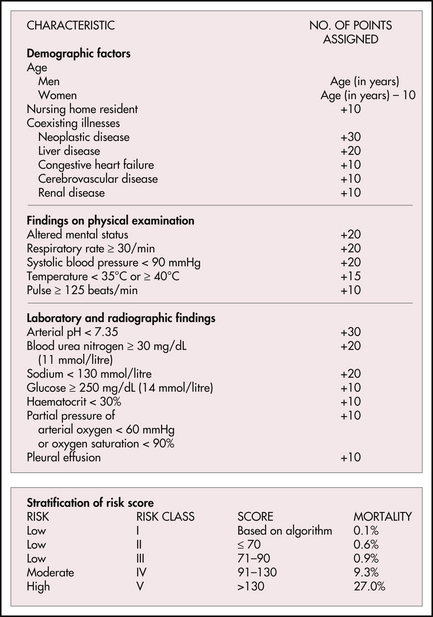
Figure 8.1 The Pneumonia Severity Index
Based on Fine MJ, Auble TE, Yealy DM et al. A prediction rule to identify low-risk patients with community-acquired pneumonia. N Engl J Med 1997; 336:243-250, as presented in Halm EA, Teirstein AS. Management of communityacquired pneumonia. N Engl J Med. 2002; 347(25):2039-2044
Consider that respiratory symptoms may be secondary to severe sepsis from another source.
Spontaneous pneumothorax
Traumatic pneumothoraces are treated more aggressively and are covered in Chapter 3, ‘Resuscitation and emergency procedures’.
Illness such as COPD and asthma may be associated with spontaneous pneumothorax, especially in association with acute exacerbations where the pneumothorax may have precipitated the presentation.
Initial stabilisation
Tension pneumothorax leading to significant compromise will be obvious clinically.
Specific treatment
Suitable for patients with moderate symptoms and a 20–40% pneumothorax with no underlying lung disease (secondary spontaneous pneumothorax).
An IV cannula and three-way tap or other catheters designed for the purpose may be used.
The pneumothorax is aspirated using a three-way tap and then X-rays are repeated.
The best choice for those with a large pneumothorax or significant underlying lung disease.
Place the tube in the 4th–5th intercostal space and directed superiorly.
Male smokers have a 20-fold increased risk of primary spontaneous pneumothorax.
COPD and cystic fibrosis patients have increased risk and associated mortality.
Acute lung injury (noncardiogenic pulmonary oedema)
Wet, stiff lungs make gas exchange and ventilation difficult.
Causes include pulmonary contusion, aspiration, chemical pneumonitis, narcotic overdose, near drowning, transfusion of blood products, SARS, avian influenza and severe sepsis.
Anaphylaxis with bronchospasm
(See also Chapter 40, ‘Dermatological presentations to emergency’.)
Hyperventilation
Blackwell N., Foot C., Thomas C. Examination intensive care and anaesthesia. Elsevier Australia; 2007.
Hillman K., Bishop G., editors. Clinical intensive care and acute medicine, 2nd edn., Cambridge: Cambridge University Press, 2004.
McKenzie DK, Abramson M, Crockett IJ et al. The COPD-X Plan: Australian and New Zealand guidelines for the management of chronic obstructive pulmonary disease 2007. Online. Available: http://www.copdx.org.au/search.asp?zoom_query=management; December 2008.
National Asthma Council of Australia. Asthma management handbook 2006. Online. Available: http://www.nationalasthma.org.au/cms/index.php; December 2008.
Sigillito R.J., DeBlieux P.M. Evaluation and initial management of the patient in respiratory distress. Emerg Med Clin N Am. 2003;21:239-258.
Warrell D.A., Cox T.M., Firth J.D., editors. Oxford textbook of medicine, 4th edn., Oxford: Oxford University Press, 2003.
Webb A.J., Shapiro M.J.. Singer M., et al, editors. Oxford textbook of critical care. Oxford: Oxford University Press, 1999.