Chapter 41 Respiratory Emergencies
ASTHMA
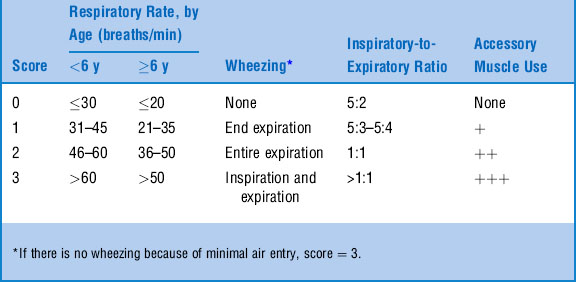
2 What is the pulmonary index?
The pulmonary index is one of many clinical scores used in the evaluation of acute asthma severity (Table 41-1). Although no single score has been shown to be superior, the pulmonary index has been used widely in asthma research. Also, there is not universal agreement on how to interpret the score. As a general guide, a score < 6 is considered mild, while a score > 10 is considered severe.
3 Describe the role of measuring peak expiratory flow rate during acute asthma exacerbations in children
6 What is Poiseuille’s law?
where n = viscosity coefficient of the gas, l = length of the tube, and r = radius of the tube. Thus, resistance to airflow increases in inverse proportion to the fourth power of the radius of the air passages. The take-home message is that a little narrowing goes a long way toward blocking air flow.
7 What are the indications for obtaining arterial blood gas (ABG) analysis in a patient with asthma?
9 A 6-year-old with asthma is treated for acute wheezing in the ED with only partial relief and needs to be admitted to the hospital. Should a chest x-ray be obtained?
10 What is the value of radiography in children with a first episode of wheezing?
Routine use of radiography in such children is of relatively low yield. However, most authorities recommend obtaining an x-ray in a child with a first episode of wheezing. A number of conditions other than reactive airways disease may present with wheezing, and these should be ruled out before a diagnosis of asthma is made (Table 41-2). Radiography is probably not necessary in children with clinical bronchiolitis of mild-to-moderate severity, or in older children with a family history of asthma who respond completely to inhaled bronchodilators; however, in most cases of first-time wheezing, a chest x-ray is prudent.
| Inflammatory/Infectious | Intraluminal Obstruction | Extraluminal Obstruction |
|---|---|---|
| Bronchiolitis | Foreign body | Vascular ring |
| Aspiration (gastroesophageal reflux, tracheoesophageal fistula) | Tracheomalacia | Mediastinal mass |
| Bronchopulmonary dysplasia | Congestive heart failure | Cystic malformation of the lung |
| Cystic fibrosis | α1-antitrypsin deficiency Cholinergic poisoning (e.g., organophosphate) | Congenital lobar emphysema |
12 What is the preferred initial treatment for children with acute asthma?
Expert Panel on Management of Asthma: Guidelines for the Diagnosis and Management of Asthma: Clinical Practice Guidelines. Available at: http://www.nhlbi.nih.gov/guidelines/asthma/asthgdln.htm
13 Isn’t nebulization a more effective means of delivering inhaled beta-agonists than a metered dose inhaler (MDI)?
Cates CJ, Bara A, Crilly JA, Rowe BH. Holding chambers versus nebulisers for beta-agonist treatment of acute asthma. Cochrane Database of Systematic Reviews 2003, Issue 2. Available at: http://www.cochrane.org/cochrane/revabstr/AB000052.htm
17 Which patients should receive ipratropium?
Plotnick LH, Ducharme FM: Combined inhaled anticholinergics and beta2-agonists for initial treatment of acute asthma in children. Cochrane Database of Systematic Reviews 2000, Issue 3. Available at: http://www.cochrane.org/cochrane/revabstr/AB000060.htm
20 What are the actions of corticosteroids in acute asthma?
22 How can steroids be given to the child who is vomiting but does not require hospital admission?
Edmonds ML, Camargo CA Jr, Brenner BE, Rowe BH: Inhaled steroids for acute asthma following emergency department discharge. The Cochrane Database of Systematic Reviews 2000, Issue 3: http://www.cochrane.org/cochrane/revabstr/AB002316.htm
23 What are the contraindications to systemic steroids?
24 Describe the role of magnesium sulfate in acute asthma
Rowe BH, Bretzlaff JA, Bourdon C, et al: Magnesium sulfate for treating exacerbations of acute asthma in the emergency department. Cochrane Database of Systematic Reviews 2000, Issue 1. Available at: http://www.cochrane.org/cochrane/revabstr/AB001490.htm
25 What is the dose of magnesium sulfate for asthma?
50–100 mg/kg (maximum 2–2.5 g) administered intravenously over 20–30 minutes.
26 What is heliox?
Rodrigo G, Pollack C, Rodrigo C, Rowe BH: Heliox for nonintubated acute asthma patients. Cochrane Database of Systematic Reviews 2003, Issue 2. Available at http://www.cochrane.org/cochrane/revabstr/AB002884.htm
27 What are the indications for endotracheal intubation and mechanical ventilation in a patient with asthma?
29 What are the two most common complications of mechanical ventilation?
 Air leak, including pneumomediastinum and pneumothorax, is common due to barotrauma.
Air leak, including pneumomediastinum and pneumothorax, is common due to barotrauma.
 Hypotension often occurs shortly after endotracheal intubation. It results from a combination of relative hypovolemia in severely ill patients and decreased venous return to the heart due to positive intrapleural pressure.
Hypotension often occurs shortly after endotracheal intubation. It results from a combination of relative hypovolemia in severely ill patients and decreased venous return to the heart due to positive intrapleural pressure.
KEY POINTS: TREATMENT OF ACUTE ASTHMA
1 Provide frequent (every 20 minutes) inhaled albuterol.
2 Provide early oral steroids (before or after first treatment).
3 Add ipratropium bromide to beta-agonists in case of incomplete response.
4 Monitor response to therapy with clinical assessment or peak expiratory flow.
5 Consider intravenous magnesium sulfate for severe or refractory cases.
BRONCHIOLITIS
33 Who is at risk for severe disease?
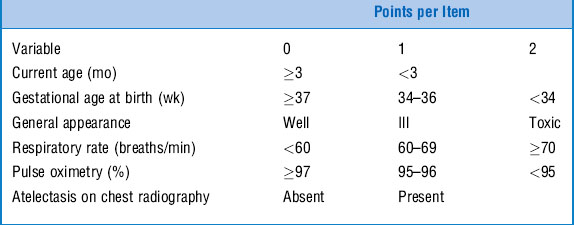
Among the risk factors for severe illness are very young age, prematurity, underlying cardiac or pulmonary disease, and immunodeficiency. Most previously healthy infants have mild to moderate disease and do not require hospitalization. However, several clinical features are predictive of development of more serious illness (Table 41-3). A score of 3 or more has a sensitivity and specificity of approximately 80% for severe disease (defined as needing hospitalization).
35 A 3-month-old child with bronchiolitis has moderate distress and a pulse oximetry of 93% in room air. She does not respond to inhaled albuterol. Is there any other effective treatment?
Hartling L, Wiebe N, Russell K, et al: Epinephrine for bronchiolitis. Cochrane Database of Systematic Reviews 2004, Issue 1: http://www.cochrane.org/cochrane/revabstr/AB003123.htm
36 Is there a role for corticosteroids in bronchiolitis?
Patel H, Platt R, Lozano JM, Wang EEL: Glucocorticoids for acute viral bronchiolitis in infants and young children. Cochrane Database of Systematic Reviews 2004, Issue 3. Available at: http://www.cochrane.org/cochrane/revabstr/AB004878.htm
CROUP
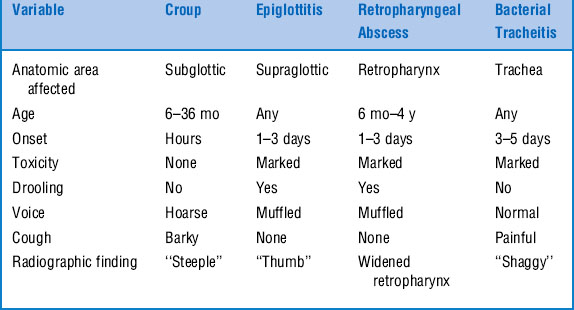
40 What is the differential diagnosis of croup?
Conditions that may be mistaken for croup include bacterial tracheitis, retropharyngeal abscess, and epiglottitis (Table 41-4). The last is a much less common entity since 1990, with the introduction of the Hib vaccine. In a 6- to 24-month-old afebrile child, an index of suspicion should be kept for an aspirated foreign body. Often a clear history of choking is not obtained.
41 When are diagnostic tests indicated (or of value) in croup?
Croup is diagnosed on the basis of presenting signs and symptoms. Children with characteristic disease do not require further diagnostic testing. Anteroposterior and lateral radiographs of the neck may be indicated in children with atypical features (e.g., age less than 6 months, recurrent or prolonged croup, toxicity on exam). The typical radiographic findings are shown in Table 41-4.
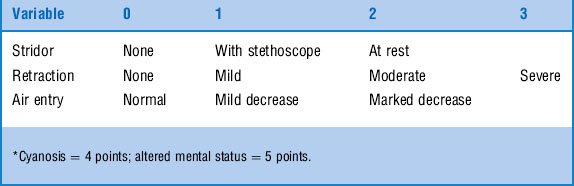
42 How do you assess the severity of croup?
Several scoring systems have been devised to assess croup severity. The most commonly used is the modified Westley score (Table 41-5). A score of < 4 indicates mild disease, 4–6 indicates moderate disease, and a score of 7 indicates severe disease.
44 Is there any scientific evidence that humidified air is beneficial in the treatment of children with croup?
45 Is there any scientific evidence that steroids are beneficial in the treatment of croup?
Russell K, Wiebe N, Saenz A, et al: Glucocorticoids for croup. Cochrane Database of Systematic Reviews 2004, Issue 1. Available at: http://www.cochrane.org/cochrane/revabstr/AB001955.htm
46 Which method of corticosteroid delivery is better: intramuscular, oral, or nebulized? What is the ideal dose?
PNEUMONIA
50 What are the most common bacterial causes of pneumonia in children?
Table 41-6 Most Common Bacterial Causes of Pneumonia In Children
| Neonate (0–2 mo) | Infant (2 mo–3 y) | Preschool/School Age (>3 y) |
|---|---|---|
| Group B streptococci | Streptococcus pneumoniae | Mycoplasma pneumoniae |
| Gram-negative bacilli | Staphylococcus aureus | Streptococcus pneumoniae |
| Staphylococcus aureus | Haemophilus influenzae* | Chlamydia pneumoniae |
| Chlamydia trachomatis | ||
| Streptococcus pneumoniae |