Respiratory Disorders of the Pediatric Patient
I Pediatric Patients Are Classified by Age as Follows
A Premature: <37 weeks gestational age
C Infant: 30 days to 12 months
II Evaluation of the Pediatric Patient for Respiratory Distress
1. Is the problem acute, recurrent, or chronic?
2. Is the problem from ingestion, inhalation, trauma, or accident?
E The majority of pediatric admissions are for respiratory-related problems.
F Causes of respiratory problems
G Clinical identification of respiratory distress
3. Tracheal tug (suprasternal retractions)
5. Seesaw (paradoxical) breathing
H Other signs of clinical significance
a. Normal temperature: 36.1° C to 37° C
b. Low-grade fever: 37.1° C to 38.4° C (normally viral infection)
c. High-grade fever: ≥38.4° C (normally bacterial infection)
III Croup (Laryngotracheobronchitis or LTB)
1. Viral infection involving the larynx and subglottic area
2. Infectious agent: Parainfluenza virus (most common) or Mycoplasma pneumoniae and respiratory syncytial virus (RSV)
C Radiologic presentation (Figure 29-1)
1. Most children are treated at home after consult with a physician.
3. Keep child calm, prevent agitation and crying.
4. Audible stridor and restlessness may require hospitalization.
5. Cool aerosol therapy via mask (mist/croup tents are no longer the standard).
6. Inhaled racemic epinephrine via small volume nebulizer every 1 to 2 hours.
7. Intramuscular or intravenous steroids; dexamethasone 0.6 mg/kg is the treatment of choice.
8. Severe cases may require He/O2 therapy for maximum deposition of aerosolized medication.
9. Sedation is contraindicated secondary to possible respiratory depression.
10. Monitor using pulse oximetry and use of arterial or capillary blood gases once patient is stabilized.
11. Observe for signs of impending respiratory failure, including
1. Bacterial infection affecting the supraglottic structures
2. Causative agent in >80% of cases is Haemophilus influenzae type B bacteria.
3. Produces an enlarged cherry red epiglottis, which can either partially or completely obstruct the airway
4. Decreased incidence of complete obstruction secondary to conjugate H. influenzae vaccinations
2. Noticeable signs of upper airway obstruction
8. Drooling (inability to swallow)
9. Hyperextension of the neck and chest thrust forward (characteristic sitting or tripod position)
C Radiologic findings (Figure 29-2)
1. For typical clinical presentations, radiographs may not be needed.
2. A lateral neck film may differentiate croup from epiglottitis.
3. Lateral neck radiograph revealing classic “thumb sign” of a swollen epiglottis and enlarged aryepiglottic folds.
1. Keep child as calm as possible.
2. Deliver cool mist aerosol to patient as tolerated.
3. Have parent or guardian hold child if possible to keep calm.
4. Have intubation and resuscitation equipment ready at the bedside.
5. Child’s mouth, tonsils, or oropharynx should not be examined unless under controlled situation.
6. If intubation required, patient should be taken to an operating room.
7. Only skilled anesthesiologists should intubate.
8. Standby tracheotomy/cricothyroidotomy equipment should also be available.
9. Use of an oral or nasal endotracheal tube (ETT) should be 0.5 mm smaller than predicted to prevent possible trauma.
10. After the airway is secured, provide patient with good pulmonary toilet.
11. Sedate patient as necessary.
12. Obtain sputum and blood cultures.
13. Hydrate patient intravenously.
14. Initiate antibiotic therapy.
15. Maintain patient intubated for 24 to 48 hours.
17. Extubate only when an audible leak is heard around the ETT.
18. Aerosolized racemic epinephrine may be required after extubation.
19. Also provide patient with cool mist aerosol, and look for signs of possible tracheal/glottic swelling postextubation.
20. Table 29-1 compares and contrasts the signs and etiology of croup and epiglottitis.
TABLE 29-1
Comparison of Croup and Epiglottitis
| Factor | Croup | Epiglottitis |
| Etiology | Virus: Parainfluenza | Bacteria: Haemophilus influenzae |
| White blood cell count | Normal | Elevated |
| Onset | Gradual | Sudden |
| Cough | Dry, barking | Muffled |
| Lateral neck radiographic film | Subglottic inflammation | Supraglottic inflammation |
| Treatment | Symptomatic | Symptomatic, artificial airway frequently required |
1. An inflammatory disease of the bronchioles
2. The most common cause of lower respiratory tract obstruction in the young child
3. Most common in children aged <2 years
4. Most common infectious agents are RSV and parainfluenza viruses.
5. Other infectious agents include parainfluenza types 1 and 3, adenovirus, and M. pneumoniae.
6. Chemical factors may also precipitate condition (e.g., cigar, cigarette smoke).
7. Occurs most frequently in the fall and winter
8. Viruses are transmitted via contact with infected secretions.
1. A lower respiratory tract infection after 2 to 3 days of
2. It may be difficult to differentiate bronchiolitis from asthma in the younger patient.
1. Usually made by analysis of nasopharyngeal cultures
3. Clinical signs and symptoms
4. Use immunofluorescent staining techniques for presence of RSV antigen.
F Management of severe symptoms
a. Respiratory rate: >45 breaths/min
b. Distant or inaudible breath sounds
a. Its use in the clinical arena is highly controversial and has fallen out of favor in most institutions.
b. Ribavirin is delivered via small particle aerosol generator (SPAG) unit.
c. Patient must have underlying cardiac disease.
d. Underlying chronic lung disease (e.g., bronchopulmonary dysplasia [BPD])
e. Immunosuppressed children (e.g., HIV, organ transplant)
3. Monitor the Pao2 and Paco2 for impending respiratory failure.
4. Monitor patient’s fluid status.
5. Follow weight loss and gain closely.
b. The patient is lethargic and difficult to arouse.
c. The patient appears exhausted.
d. Desaturation continues despite increased FIO2 requirement.
a. Provide patient with adequate sedation.
b. Vigorous chest physiotherapy (CPT) should be performed.
c. Continue bronchodilator treatment through mechanical ventilator.
d. Maintain appropriate fluid status.
e. Monitor input and output closely.
f. Look for resolution of symptoms 3 to 5 days postintubation.
g. May take longer if patient has underlying disease process.
1. Inherited as a recessive disorder that involves the exocrine glands
2. Disorder prompted by mutations of a single gene pinpointed on the seventh chromosome
3. Autosomal recessive means that the CF gene can occur in either male or female children.
4. Disease affects nearly every organ system in the body that contains epithelial surfaces.
5. CF causes exocrine glands to produce abnormally viscid secretions, as well as pancreatic deficiency and a high sweat electrolyte concentration.
6. Sixty percent of patients are diagnosed during the first year of life, and 90% are diagnosed by age 5 years.
7. Median survival age greatly increased because of newer treatment modalities, now >30 years of age.
B Clinical manifestations result from abnormal secretions from the sweat glands, bronchial glands, mucosal glands, small intestine, pancreas, and bile ducts of the liver.
1. Sweat glands: There is abnormal absorption of sodium and chloride (two to five times normal), but water reabsorption is normal.
2. Pancreas: Eighty percent of patients with CF have pancreatic deficiency. A low-volume, highly viscid fluid that has few enzymes to break down ingested fat is secreted. Insulin secretion is impaired as a result of fibrosis. Diabetes is often present in older children.
3. Intestine: Mucous glands of the intestine are involved, causing tarry, viscous feces in the newborn. A distended abdomen results from failure to pass feces.
4. Liver: Lesions found in the liver are similar to those of the pancreas. Blockage of bile ducts and fibrosis results.
5. Bronchial glands: Excessive thick, tenacious mucus is produced, which obstructs small airways and produces respiratory insufficiency and pulmonary hypertension.
1. At birth the size of the bronchial glands is normal, but hypertrophy and hypersecretion quickly develop.
2. Obstruction of small bronchi and bronchioles from thick, tenacious secretions occurs.
3. Overdistention of the lung and dilation of airways follow.
4. Infection from stagnant mucus, Pseudomonas aeruginosa, and Staphylococcus aureus is common.
5. Progression of the disease results in
a. Consolidation and atelectasis
b. Destruction of respiratory epithelium and simple squamous epithelium
6. Progressive respiratory failure occurs with marked hypercapnia, hypoxemia, and pulmonary hypertension.
7. Congestive heart failure follows.
8. Ninety-eight percent of patients die from cardiorespiratory failure.
1. Diagnosis is based on clinical symptoms and family history.
2. In the newborn failure to pass meconium (first feces) within 12 hours of birth is common.
3. CFTR is the gene responsible for CF.
4. Diagnosis is based on the combination of one or more typical phenotypic features and evidence of CFTR malfunction.
a. Chronic sinopulmonary disease
b. Persistent infection with typical CF pathogen (e.g., S. aureus, P. aeruginosa)
d. Persistent chest radiographic abnormality (e.g., bronchiectasis, hyperinflation, and atelectasis)
e. Airway obstruction (e.g., wheezing, decreased expiratory flows)
5. Gastrointestinal, nutritional abnormality
a. Intestinal: Meconium ileus, rectal prolapse, and distal intestinal obstruction syndrome
b. Pancreatic: Pancreatic insufficiency, recurrent pancreatitis
c. Hepatic: Focal biliary cirrhosis
d. Nutritional: Malnutrition, hypoproteinemia, and fat-soluble vitamin deficiency
7. Male urogenital abnormality
8. Presence of the CFTR gene abnormality
a. Determined by a sweat chloride test
b. A result >60 mmol/L on two occasions (minimum 75 mg of sweat collected during 30 minutes) indicates a positive presence.
d. Two mutant CTFR alleles required
e. Nasal potential difference (PD) testing
g. Greater amiloride-sensitive PD
h. Absent or minimal change in PD after isoproterenol in chloride-free perfusion solution
1. Earliest pulmonary symptoms
b. Progression of cough to more frequent coughing spells with production of large quantities of secretions
d. Fatigue, anorexia, and weight loss
e. Chest radiograph shows hyperinflation (with flattened diaphragms in the older child).
h. Airways become persistently infected with gram-negative pathogens, such as P. aeruginosa.
i. Symptoms recur more often than usual and become less responsive to intensive and aggressive therapy.
2. The older child has muscular weakness and growth retardation, short stature, reproductive tract underdevelopment, and clubbing of the digits.
3. Development of subpleural air cysts is likely responsible for increased incidence of spontaneous pneumothorax; 5% to 8% in children and 16% to 20% in adults.
4. Hemoptysis (>240 ml in 24 hours) can occur, although it is now less common, occurring in approximately 5% of patients.
5. Respiratory failure caused by progressive airway obstruction and destruction is the universal cause of death in 98% of CF patients.
1. Pulmonary function testing is a sensitive and reliable way to evaluate the severity of CF lung disease.
2. It is an objective means to determine when a patient’s clinical status has deteriorated and requires more intensive therapy.
3. Primary alteration is a decrease in compliance and an increase in respiratory rate.
4. The Paco2 level is reduced or near normal in the early stages of the disease, progressing to hypercapnia.
5. The first abnormality detected is obstruction of small airways.
6. Indicated by reduced flow rates at low lung volumes (FEF 25% to 75%).
7. Elevation of residual volume-to-total lung capacity ratio also seen (RV/TLC).
8. FEV1 is the best indicator of exercise capacity and disability and somewhat predictive of length of survival.
9. Hypoxemia develops as airway obstruction worsens as a result of ventilation/perfusion mismatching.
10. Spirometric parameters are poor predictors for the need of oxygen therapy.
11. Supplemental oxygen is most always required in later stages of disease.
12. Oxygen therapy generally is effective for the prevention of pulmonary hypertension and cor pulmonale.
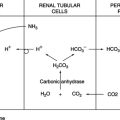
13. Severe airway disease causes retention of carbon dioxide because of an increased dead space-to-tidal volume ratio (Vd/Vt), which in turn may worsen hypoxemia.
14. Carbon dioxide retention and severe airway obstruction along with resting hypoxemia are negative predictors of survival.
15. Lung transplantation is another option for those with deteriorating pulmonary function tests (PFTs).
16. FEV1 of approximately 30% of predicted maximum FEV1considered an indication for lung transplantation, although other factors should be considered.
1. Often normal in the early course of the disease
2. Hyperinflation may be the first radiologic finding in children.
3. Increased interstitial markings are common.
4. These progress to typical findings of cystic bronchiectasis.
5. Atelectasis in the right upper lobe frequently is seen.
6. Progression of the disease leads to hyperinflation and flattening of the diaphragms and increased anteroposterior diameter.
7. The heart shadow is narrowed.
8. Chest computerized tomography (CT) scans may be useful to detect earlier physiologic changes not visible on routine chest radiographs.
9. Chest CT indicated for the CF patient suspected of having nontuberculous mycobacterium (NTM). NTM infection demonstrates multiple small parenchymal nodules primarily in the middle and lower lobes and patchy airspace disease.
1. Airway clearance techniques (see Chapter 36)
a. Physical maneuvers to promote the movement of airway secretions from small toward central airways where they may be removed by cough.
b. Chest percussion and postural drainage are most effective.
c. Postural drainage uses multiple body positions to facilitate drainage of individual lung segments via gravity.
d. Performed in conjunction with chest percussion and vibration
e. Has been shown to improve mucus clearance and pulmonary function in otherwise stable patients
f. Time consuming and often difficult for patient to tolerate
g. Mechanical percussors are sometimes used.
h. Forced expiratory maneuvers, positive expiratory pressure (PEP) devices, the flutter valve, and exercise all assist in airway clearance.
i. The high frequency chest compression vest (ThAIRapy vest), autogenic drainage, and the active cycle of breathing technique are also used.
j. Exercise has been shown to assist secretion removal, but the need for oxygen therapy during exercise should be assessed periodically.
2. Aerosolized recombinant human DNase (rhDNase; Pulmozyme) (see Chapter 17)
a. Used to modify the transportability of secretions
b. DNA is a major component of CF secretions, which are extremely viscous and poorly transportable within the airway.
c. rhDNase was developed and approved for use in patients with CF in 1994.
d. A single daily use has been shown to improve FEV1 by 6% and to decrease exacerbations by 28%, but response can be variable.
e. Most patients show a response within 1 to 3 months after initiation of drug use.
f. Efficacy of rhDNase over longer periods and its impact on mortality remain unknown.
3. Other mucus-modifying agents
a. N-acetyl-L-cysteine (Mucomyst) is most commonly used.
b. Agent reduces disulfide bonds in mucins, thus making them less viscous.
c. This agent is known to increase epithelial injury or inflammation.
d. Despite its common use it is not approved for inhalation, and no data demonstrate it improves secretion removal when aerosolized.
4. Hypertonic saline solutions are used to promote hydration of inspissated mucous secretions.
a. Three percent NaCl is used after albuterol pretreatment.
a. Oral and inhaled antibiotics are an important part of a standard CF regimen.
b. Oral antibiotics are used episodically when new respiratory symptoms develop.
c. Ciprofloxacin is the primary oral agent to manage P. aeruginosa, but rapid development of resistance should be considered.
d. There are a limited number of oral agents available for management of P. aeruginosa.
e. Inhaled aminoglycosides and other parenteral antibiotics are now used.
f. Inhaled route of administration has the benefit of achieving high drug levels in airway secretions.
g. Minimal systemic levels are developed during inhalation, avoiding toxicity.
h. High drug concentrations in secretions, beneficial for the management of organisms resistant to antibiotic concentrations, are achieved intravenously.
i. The most effective inhaled antibiotic is high-dose tobramycin (300 mg, twice daily).
j. An alternative to inhaled tobramycin is inhaled colistin (75 to 150 mg, twice daily), good in vitro activity against P. aeruginosa.
k. Colistin is less well studied in clinical trials, and bronchospasm is a more common side effect with its continued use.
a. Inhaled bronchodilators are commonly prescribed for management of CF.
b. Twenty-five percent of CF patients have bronchial reactivity and do respond to bronchodilator therapy.
c. Bronchodilators may improve respiratory symptoms and airway secretion clearance.
d. Inhaled anticholinergic agents, especially ipratropium bromide, may also have a role in CF.
a. Used to lessen neutrophilic inflammation and harmful effects of neutrophil products
b. Use of high-dose corticosteroids has yielded mixed results.
c. Patients receiving 1 to 2 mg/kg of prednisolone on alternate days have shown a slowed decrease in lung function.
d. Inhaled steroids have been studied in patients with CF, and their efficacy is yet to be determined.
e. High-dose ibuprofen is used to lessen neutrophilic inflammation, although further studies are needed to determine benefit of such therapy.
a. Has become an accepted therapy for end-stage CF lung disease
b. Waiting times >2 years at some centers
c. Indications for transplantation
(1) Accelerated clinical decline
(2) Exacerbations not responding to aggressive therapy
(3) Recurrent pneumothoraces, recurrent hemoptysis, and presence of pan-resistant organisms should prompt consideration for early referral.
d. Optimal candidates should not have significant other organ dysfunction (e.g., kidney, liver).
e. Candidate should be motivated and compliant with therapy.
f. Candidate should have adequate psychosocial support.
g. Five-year survival rate is approximately 48%. Survival is limited by opportunistic infections and chronic graft rejection, manifesting as bronchiolitis obliterans.
VII Foreign Body Aspiration (FBA)
1. Children aged 7 months to 4 years are at risk for aspirating a foreign body.
2. Foreign bodies usually obstruct the larynx, trachea, or bronchi.
3. Majority of materials aspirated are radiolucent and cannot be seen on typical chest radiographs.
4. The major cause of death in children aged <6 years
5. Common aspirated objects include small toys, balloons, hot dogs, beans, peanuts, coins, nuts, raisins, and buttons.
1. Aspirated material obstructing the trachea is a medical emergency. Symptoms include
2. Aspirated material lodged in the trachea or bronchus usually stimulates a violent cough, sneezing, and possibly bloody sputum if the material is sharp.
a. Foreign bodies may create a partial or complete obstruction.
b. Foreign bodies lodged in the trachea or larynx that completely occlude the airway are most life threatening.
c. Can lead quickly to respiratory arrest and death if object cannot be removed quickly.
d. Heimlich maneuver is most effective or by other means available to trained health care personnel.
e. For more definitive management of upper airway obstruction in children refer to the American Heart Association Basic Life Support Guide.
C Management and complications
1. Children who aspirate foreign bodies seldom cough up the object spontaneously.
2. Objects deposited in the laryngeal area may be removed via direct laryngoscopy by a skilled physician.
3. The presence of a foreign body in the trachea or bronchi can be confirmed with the use of a flexible fiberoptic bronchoscope.
4. Definitive management and removal of a foreign body located distal to the larynx should be done with a rigid bronchoscope while the child is under general anesthesia.
5. Potential complications of FBA include pulmonary air leak if object is lodged distal to the trachea.
6. Cardiopulmonary arrest and death may occur if foreign body is dislodged from the lower airway and then occludes the opposite mainstem bronchus or trachea.
7. Bronchiectasis can develop if the object is left in the airway for an extended period.
8. Pneumonia can develop if certain materials are aspirated or if incomplete removal occurs during bronchoscopy.
9. Repeat bronchoscopy, antibiotic therapy, and postural drainage/CPT may also be necessary as adequate treatment modalities.
A Etiology (Modified from National Asthma Education and Prevention Program of the National Institutes of Health, 1997)
1. Asthma is a condition caused by hyperactive airways.
2. The patient can have an exacerbation triggered by various allergic and nonallergic stimuli.
3. The most common mechanism for asthma is allergy.
4. Other mechanisms include cold exposure, stress, exercise, infection, and other nonspecific inhaled irritants, cigarette smoke, pollen, animal dander, viruses, and exhaust fumes.
5. Pediatric asthma affects 5% to 10% of all children in the United States.
6. Common cause of absenteeism in school-aged children
7. Hospitalization and mortality rates in pediatric asthma have increased dramatically in the past decade.
8. Exacerbations are often reversible either spontaneously or with treatment.
1. Hyperresponsive lower airways to various allergic and nonallergic stimuli
2. Classic presentation is an “attack” or spasm of bronchial smooth muscle.
3. Bronchospasm occurs within the first hour after exposure to airway stimuli.
4. Histamine and other mast cell mediators are released to prolong reaction.
5. Airways release a host of inflammatory mediators leading to hypersecretion of mucus.
6. Airway response includes goblet cell hyperplasia, smooth muscle hypertrophy, and other inflammatory reactions.
7. Increased volume of mucus mixes with inflammatory cells to form thick, tenacious plugs that occlude small airways.
8. Combination of bronchospasm and inflammation causes a significant degree of airway obstruction.
9. Resultant obstruction leads to air trapping and a potential auto-positive end-expiratory pressure effect.
10. This produces ventilation/perfusion abnormalities with hypoxic vasoconstriction.
11. Air trapping and hyperinflation can occur.
12. Changes in pulmonary mechanics include reduced compliance, increased airway resistance, and increased functional residual capacity.
1. A child with an asthma exacerbation may first present with a cough and dyspnea.
2. Wheezing with decreased air entry is heard on auscultation.
3. Audible wheezing without use of a stethoscope indicates possible moderate or severe attack.
4. Child may be diaphoretic or cyanotic.
5. Absence of wheezing does not rule out attack because poor airflow may be severe enough as to not elicit audible wheeze.
6. Cyanosis is a late grave sign of respiratory insufficiency that must be managed immediately.
7. Tachypnea and tachycardia are almost always present.
8. Use of accessory muscles is common.
9. Pulsus paradoxus is present in moderate and severe attacks.
11. Hypercarbia, Pco2 >50, should alert clinician of a deteriorating condition, usually in need for intubation.
12. Inability to speak in complete sentences in older children is another sign of pulmonary insufficiency.
1. Initial chest film reveals hyperinflated lungs with flattened diaphragms.
2. Lungs fields may otherwise appear relatively clear.
3. Follow-up films may show increased opacity with consolidated lung.
4. If inflammatory process is allowed to continue, infiltrates can develop.
1. Atopy (familial or genetic)
a. Strongest identifiable predisposing factor for development of asthma
b. Familial or genetic predisposition to develop an immunoglobulin E (IgE)-mediated response to allergens in the environment
c. More prevalent in pediatric or allergic asthma
d. Easiest diagnosis is through skin-prick testing.
e. Most common method is the radioallergosorbent (RAST) test, which measures antigen-specific IgE.
f. Highest risk factors of atopic asthma are for inner-city children, where cockroach antigen, animal dander, and dust mites are common.
g. Other factors that may contribute to development of asthma include environmental pollution, low birth weight, tobacco smoke, diet, or viral infections.
a. Attacks are exacerbated by inhalation of an allergen.
b. Indoor allergens include mold, animal dander, cleaning chemicals, cockroach antigen, and dust mites.
c. Outdoor allergens include cold air, noxious fumes, grass, and tree pollens.
a. Role of indoor and outdoor air pollution in development of asthma remains unproved and controversial.
b. Research has failed to develop a direct link between air pollution and asthma.
c. Mainly associated with industrialized nations with large amounts of industrial or photochemical smog
d. Indoor air pollutants have a higher association with development of respiratory symptoms.
e. Smoking has not been indicated as a general risk factor for development of asthma.
f. Smoking does seem to play a role in eliciting exacerbations in patients with asthma who are exposed.
g. Other potential sources of indoor air pollution include nitric oxide, carbon dioxide, carbon monoxides, sulfur dioxides, formaldehydes, and biologic endotoxins.
a. Patients with food allergies increase their potential to develop exacerbations.
b. Foods containing salicylates, certain food-coloring agents, food preservatives, and monosodium glutamate are substances known to trigger responses.
c. Many drugs are associated with an increased likelihood of a response.
d. Primary risk is with nonsteroidal antiinflammatory agents and aspirin.
e. Patients with sensitivity to aspirin have increased risk of developing asthma later in life.
a. Viral illness seasons (October through December and February through April) are the most prevalent periods for hospitalizations for asthma in children and adults.
b. Evidence of respiratory tract infection is indicative of a viral response.
c. Often called intrinsic asthma
d. Inflammatory responses to viral infections may start a cascade of symptomatic wheezing and excessive mucous production in the airways.
e. Induced sputum analysis can be a useful marker of the effects of natural colds and influenza on the airways of the lungs.
f. A relationship exists between respiratory viral infections in early childhood and the development of asthma.
g. Most prominent viral infection is RSV.
h. Respiratory tract infections are a significant risk factor for the initiation of an asthma exacerbation.
i. Families of children with asthma have benefited from written treatment plans that initiate more aggressive outpatient treatment with the onset of coldlike symptoms.
1. Asthma in the child is primarily based on a history of recurrent episodes of reversible airway obstruction triggered by certain allergic or nonallergic stimuli.
2. A family history of atopy predisposes a child to the development of asthma.
3. Children with history of repeated episodes of viral bronchiolitis, pneumonia, and gastroesophageal reflux are at increased risk to develop reactive airways.
4. Children with a history of BPD are also at higher risk to develop reactive airways.
5. A definitive diagnosis is difficult to obtain in the young child.
6. PFTs may prove useful to detect small airway obstruction in the older child.
7. Reversibility of a child’s airway obstruction can be assessed with pre- and post-bronchodilator spirometry.
8. Degree of airway responsiveness may also be assessed through the use of a metacholine challenge.
a. Child inhales a small amount of aerosolized metacholine.
b. After inhaling the irritant the child performs a forced vital capacity maneuver.
c. The more responsive the child’s airways, the smaller the amount of metacholine required to produce a significant decrease in pulmonary function.
9. Another measurement is a test for the presence of specific IgE antibodies; many children with asthma and atopy have elevated levels of IgE present in their serum.
H Management (Refer to Chapter 20 for exact details of the NHLBI Global Strategy for asthma management and prevention guidelines.)
1. Treatment of a child with an asthma attack is based on relief of airway obstruction.
2. The second objective is to prevent “late phase” inflammatory reactions through the use of certain antiinflammatory agents.
3. Primary medications used for the management of asthma in children are inhaled β-adrenergic bronchodilators and corticosteroids.
4. Oxygen therapy also is used to keep Pao2 at 60 to 70 mm Hg and Sao2 at >90%.
5. “Quick relief” medications are primarily short acting β-agonists used to combat acute exacerbations of bronchoconstriction.
6. “Controller medications” are taken daily in an attempt to control mediator release in the airways.
7. Management of severe asthma (status asthmaticus) (Tables 29-2 and 29-3)
TABLE 29-2
| Severity Level | Symptoms/Day Symptoms/Night | Daily Medications* |
• High-dose inhaled corticosteroids AND
• Long-acting inhaled β2-agonists AND, if needed,
• Corticosteroid tablets or syrup long term (2 mg/kg/day, generally do not exceed 60 mg/day). (Make repeated attempts to reduce systemic corticosteroids and maintain control with high-dose inhaled corticosteroids.)
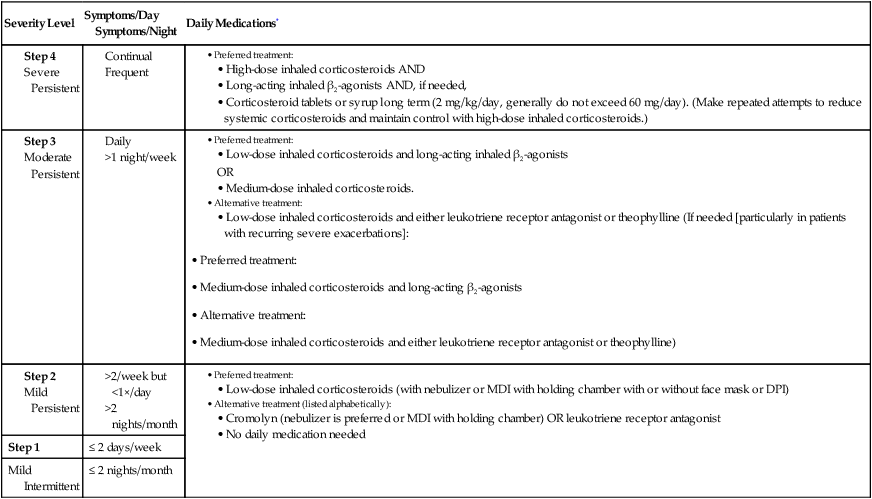
*Medications required to maintain long-term control. MDI, Metered dose inhaler; DPI, dry powder inhaler.
From Making a Difference in the Management of Asthma: A Guide for Respiratory Therapists. Washington DC, U.S. Department of Health and Human Resources, 2003, NIH publication no. 02-1964.
TABLE 29-3
Dosages of Drugs for Asthma Exacerbations in Emergency Medical Care or Hospital
| Child Dose* | Comments | |
| Albuterol | ||
| Nebulizer solution (5.0 mg/ml, 2.5 mg/3 ml, 1.25 mg/3 ml, 0.63 mg/3 ml) | 0.15 mg/kg (minimum dose, 2.5 mg) every 20 min for 3 doses, then 0.15-0.3 mg/kg up to 10 mg every 1-4 hr as needed, or 0.5 mg/kg/hr by continuous nebulization | Only selective β2-agonists are recommended. For optimal delivery, dilute aerosols to minimum of 3 ml at gas flow of 6-8 L/min |
| MDI (90 μg/puff) | 4-8 puffs every 20 min for 3 doses, then every 1-4 hr. Use spacer/holding chamber. | As effective as nebulized therapy if patient is able to coordinate |
| Bitolterol | ||
| Nebulizer solution (2 mg/ml) | See albuterol dose; thought to be half as potent as albuterol on a milligram basis | Has not been studied in severe asthma exacerbations; do not mix with other drugs |
| MDI (370 μg/puff) | See albuterol dose | Has not been studied in severe asthma exacerbations |
| Levalbuterol (R-albuterol) | ||
| Nebulizer solution (0.63 mg/3 ml, 1.25 mg/3 ml) | 0.075 mg/kg (minimum dose, 1.25 mg) every 20 min for 3 doses, then 0.075-0.15 mg/kg up to 5 mg every 1-4 hr as needed, or 0.25 mg/kg/hr by continuous nebulization. | 0.63 mg of levalbuterol is equivalent to 1.25 mg of racemic albuterol for efficacy and side effects |
| Pirbuterol | ||
| MDI (200 μg/puff) | See albuterol dose; thought to be half as potent as albuterol on a milligram basis | Has not been studied in severe asthma exacerbations |
| Systemic (Injected) β2-Agonists | ||
| Epinephrine 1:1000 (1 mg/ml) | 0.01 mg/kg up to 0.3-0.5 mg every 20 min for 3 doses subcutaneous | No proven advantage of systemic therapy over aerosol |
| Terbutaline (1 mg/ml) | 0.01 mg/kg every 20 min for 3 doses, then every 2-6 hr as needed subcutaneous | No proven advantage of systemic therapy over aerosol |
| Anticholinergics | ||
| Ipratropium bromide | ||
| Nebulizer solution (0.25 mg/ml) | 0.25 mg every 20 min for 3 doses, then every 2-4 hr | May mix in same nebulizers with albuterol. Should not be used as first-line therapy; should be added to β2-agonist therapy |
| MDI (18 μg/puff) | 4-8 puffs as needed | Dose delivered from MDI is low and has not been studied in asthma exacerbations |
| Ipratropium with Albuterol | ||
| Nebulizer solution (Each 3-ml vial contains 0.5 mg ipratropium bromide and 2.5 mg albuterol) | 1.5 ml every 20 min for 3 doses, then every 2-4 hr | Contains EDTA to prevent discoloration; this additive does not induce bronchospasm |
| MDI (Each puff contains 18 μg ipratropium bromide and 90 μg of albuterol) | 4-8 puffs as needed | Combivent MDI |
| Systemic Corticosteroids | ||
| Prednisone, methylprednisolone, prednisolone† | 1 mg/kg every 6 hr for 48 hr, then 1-2 mg/kg/day (maximum = 60 mg/day) in 2 divided doses until PEF 70% of predicted or personal best | For outpatient “burst” use 40-60 mg in single or 2 divided doses for adults (children, 1-2 mg/kg/day; maximum, 60 mg/day) for 3-10 days |
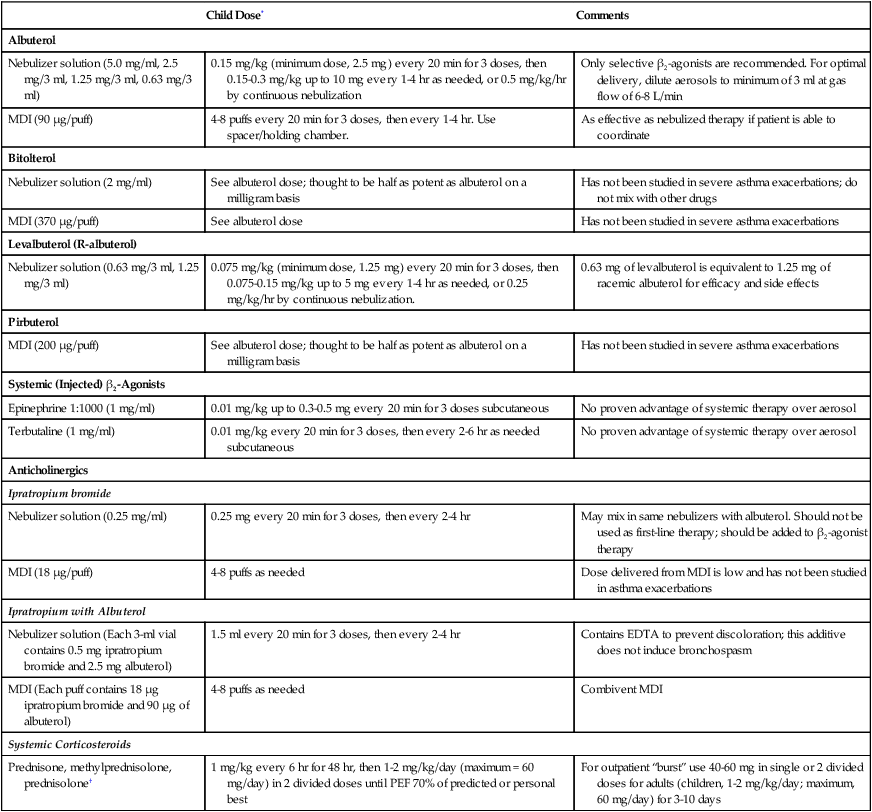
MDI, Metered dose inhaler; EDTA, ethylenediaminetetraacetic acid; PEF, peak expiratory flow.
†Dosages and comments apply to all three corticosteroids.
From Making a Difference in the Management of Asthma: A Guide for Respiratory Therapists. Washington, DC, U.S. Department of Health and Human Resources, 2003, NIH publications no. 02-1964.
a. Inhaled β2-specific bronchodilators first-line therapy for management of an attack
b. Inhaled albuterol, as well as intravenous terbutaline, has proved safe and effective for the management of childhood asthma.
c. Recommended frequency of albuterol is every 4 to 6 hours with a maximum dosage of 5 mg.
d. However, albuterol aerosols may be given every 20 minutes to the unstable patient in the emergency department under constant monitoring.
e. Newer guidelines suggest the use of continuous bronchodilator therapy for the severely exacerbated patient not responding to conventional care.
f. Pediatric patients are more tolerant of specific side effects associated with aggressive treatment: tachycardia, tachypnea, and increased work of breathing.
g. A small volume nebulizer (SVN) is the most effective way to deliver aerosolized medication to the child.
h. Depending on the patient’s age the parent may have to hold the nebulizer to the child’s face.
i. Additional intravenous medications are also used to manage exacerbations.
(1) Intravenous corticosteroids are effective; initially high doses are given, but they may take several hours to demonstrate effects.
(2) Intravenous magnesium sulfate is also used.
(3) Magnesium is a calcium channel blocker in the airway smooth muscle and an inhibitor of acetylcholine and histamine release.
(4) Onset of action can occur within minutes, but effectiveness is difficult to quantify.
(5) Use of magnesium sulfate for the management of status asthmaticus remains controversial.
j. Usual signs of improvement after treatment(s) include decreased wheezing, improved work of breathing, improved O2 saturations, improved peak flow, and overall improvement in patient’s mental and anxiety status.
k. Signs of failure or nonresponse to therapy include Paco2 >40 mm Hg, refractory hypoxemia (Pao2, <60 mm Hg and FIO2, >50%), mental status deterioration, decreased or absent breath sounds, and apneic episodes.
1. Corticosteroids are considered the most potent antiinflammatory agents available.
a. Daily antiinflammatory therapy has shown to actively control severe cases of asthma.
b. Corticosteroids have been shown to suppress the release of certain inflammatory mediators.
c. Shown to decrease airway hyperresponsiveness
d. Can be inhaled, taken orally, or administered intravenously
e. Dosage and frequency can vary depending on patient condition and present physiology.
f. Some studies have demonstrated that once-daily dosing can be effective therapy for patients with mild, persistent asthma.
g. The effect of corticosteroids on the growth of preadolescents who are taking this type of medication is controversial.
2. Nonsteroidal antiinflammatory medications
a. Most common type of long-term controller medications used in adolescents and children
b. The two most popular are cromolyn sodium (Intal) and nedocromil (Tilade).
c. Similar method of action; chloride channel blocker acting to disrupt mast cell mediator release and promote eosinophil release
d. These medications can reduce the need for quick relievers and reduce bronchial hyperresponsiveness.
e. They can also improve morning peak flows and decrease symptoms of nocturnal asthma.
a. Considered a long-term controller medication
b. Not intended for acute bronchospasm relief
c. Medication acts as a stimulant to increase cyclic adenosine monophosphate and produce antagonistic reactions to bronchoconstriction.
d. Long-acting β2-agonists appear to target asthma symptoms that seem to worsen at night.
e. Duration of effect: approximately 12 hours
f. Salmeterol (Serevent) is the drug of choice for this group of patients.
a. Long-term controller used predominantly to provide mild to moderate bronchodilation.
b. Principal medication in this class is theophylline.
c. Slow-release theophylline is used as an adjunctive therapy for nocturnal asthma.
d. Acts as a nonselective phosphodiesterase inhibitor
e. The drug is relatively safe but requires frequent monitoring of serum drug levels to keep patient within therapeutic range for maximum effect.
f. Increased serum drug levels are associated with tachycardia, nausea and vomiting, headache, seizures, hyperglycemia, and hypokalemia.
g. Therapeutic serum range has recently been decreased to 5 to 15 mcg/L.
a. Newest class of medications introduced to clinicians in >20 years
b. Considered controller medications
c. Leukotrienes are considered inflammatory mediators.
d. They are mediators responsible for release of chemicals from inflammatory cells, mast cells, eosinophils, and basophils.
e. These reactions lead to bronchoconstriction, increased vascular permeability, and secretion production.
f. Leukotriene modifiers appear to work via two routes: leukotriene modifiers (zafirlukast/montelukast) and a leukotriene receptor antagonist.
g. Other agents (zileuton) act as inhibitors of leukotriene release.
h. They both act to block leukotriene receptor sites.
i. Can be an oral alternative therapy to inhaled corticosteroids.
j. Zileuton is more controversial because of its potential to induce liver toxicity.
1. Begins at diagnosis and is reinforced with each visit
2. Teach patient or parent of a child the basic facts about asthma.
3. Teach necessary medication skills, techniques, delivery devices, and dosing regimens.
4. Teach self-monitoring skills and symptom-based, peak flow monitoring.
5. Teach relevant environmental control and avoidance strategies.
6. Provide a written asthma exacerbation treatment plan.
7. Children as young as 2 years of age can begin learning about asthma and its management.
8. The asthma educator must be prepared to intervene and solve problem areas that may appear to be neglected by the patient.
9. Educator should be well versed in knowledge of medications, level of treatment, trigger avoidance, compliance, and self-management skills.