13 Respiratory disease
Approach to the patient
For management of a massive haemoptysis, see Box 13.1.
Box 13.1 Management of massive haemoptysis
Shortness of breath
Most people get breathless on exertion; exercise tolerance should be documented. Breathlessness can be of sudden onset, e.g. in acute left ventricular failure, or more progressive, as in COPD. It may vary at different times of the day, e.g. in asthma it is usually worse in the morning.
Breathlessness on lying flat occurs in, for example, pulmonary oedema (p. 425). Breathlessness with a wheeze occurring on exposure to an allergen is seen in asthma (e.g. horse riding). It can occur many hours after exposure to an allergen (p. 520) in, for example, hypersensitivity pneumonitis.
Inhalation of foreign bodies can cause choking and acute shortage of breath. Treatment is with the Heimlich manoeuvre. See Emergencies in Medicine p. 714.
Chest pain
Chest pain in respiratory disease is usually pleuritic. Pain can be due to other causes, e.g. localized pain in costochondritis. Shoulder tip pain suggests irritation of the diaphragmatic pleura. Retrosternal soreness occurs with tracheitis but also in other conditions, e.g. oesophagitis, when it is usually burning. Chest pain should always be differentiated from cardiac pain, which is usually a central crushing chest pain radiating to the jaw, neck and left arm (p. 431).
Chronic obstructive pulmonary disease
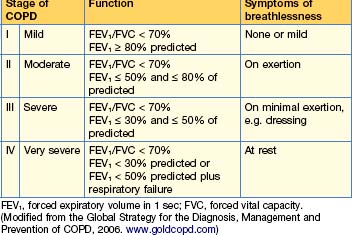
Chronic obstructive pulmonary disease (COPD) is a slowly progressive condition predominantly caused by smoking and is the sixth commonest cause of death worldwide; its incidence is increasing. It is characterized by airflow limitation, which is not fully reversible. The lungs have an abnormal inflammatory response to inhaled particles or gases, resulting in airflow limitation. The GOLD (Global Initiative for Chronic Obstructive Lung Disease, WHO) criteria for the diagnosis of lung disease are shown in Table 13.1.
Pathogenesis
Clinical features
COPD is suspected on the basis of chronic progressive symptoms, usually with a smoking history of more than 20 pack years (1 pack year = 20 cigarettes per day for 1 year). It is supported by objective evidence of airflow limitation (or obstruction), usually with spirometry, which does not return to normal with treatment.
Signs
Diagnosis and investigations
Lung function tests
Other tests
Management
Smoking cessation
Drug therapy
Bronchodilator therapy
Side-effects include fine tremor, nervous tension, tachycardia, arrhythmias and hypokalaemia.
In mild disease short-acting β2 agonists or short-acting antimuscarinic bronchodilators should be prescribed as required. Their effects are additive and once airflow becomes more severe a regular antimuscarinic can be added to a β agonist. Some patients prefer to use just one combined inhaler ipratropium bromide 20 mcg and salbutamol 100 mcg/metered dose 2 puffs 4 times a day.
Corticosteroids
There are many side-effects associated with corticosteroids (see Box 15.2, p. 585). Inhaled steroids cause considerably fewer systemic side-effects, although at high doses adverse effects have been reported.
Combination therapy
Oxygen therapy
The following patients should be assessed for oxygen therapy:
Patients fulfil the criteria for LTOT when they have:
Guidelines for domiciliary oxygen are shown in Box 13.2.
Box 13.2 Guidelines for domiciliary oxygen (Royal College of Physicians, 1999)
Non-invasive ventilation (NIV)
This is mainly used for exacerbations of COPD — see p. 485. The ventilators are small and can be used at home. Patients should be considered for home NIV if, despite maximal treatment, they have hypercapnic respiratory failure and have required ventilatory support during an exacerbation, or are acidotic or hypercapnic on LTOT.
Diuretic therapy (p. 420)
This is necessary for all oedematous patients. Patients should be weighed daily.
Other agents
• Antibiotics
• Vaccination/antiviral therapy
Non-pharmacological interventions
Acute exacerbations of COPD (type II respiratory failure)
Investigations
Treatment
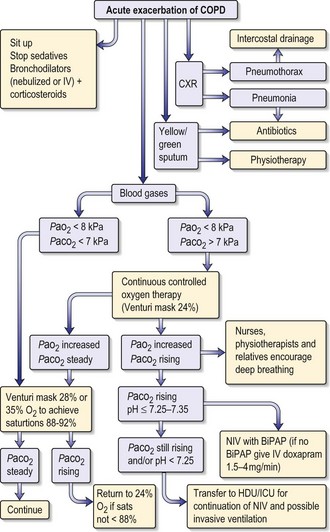
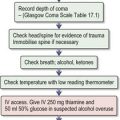
The treatment of respiratory failure in COPD is shown in Fig. 13.1. General care includes prophylaxis against deep vein thrombosis, optimizing fluid status and ensuring adequate nutrition.
• Non-invasive ventilation (NIV)
A tight-fitting facial mask delivers bi-level positive airway pressure ventilatory support (BiPAP). Continuous positive airway pressure (CPAP, p. 542) is also used. NIV can avoid the need for endotracheal intubation.
Prognosis of COPD
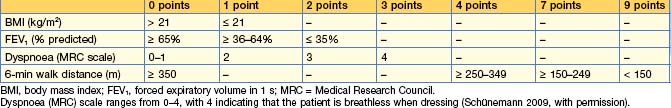
The predictors of a poor prognosis are increasing age and worsening airflow limitation, i.e. a fall in FEV1. A predictive index (BODE = body mass index, degree of airflow obstruction, dyspnoea and exercise capacity) has recently been modified, improving prediction of outcome, and is shown in Table 13.2. A patient with a BODE index of 0–2 has a mortality rate of 10% and with 7–10 it rises to 80% at 4 years. A simpler index using age, dyspnoea and airflow obstruction (ADO) gives a similar prognosis.
Discharge planning
Obstructive sleep apnoea/hypopnoea syndrome
Investigations
Sleep studies
Treatment
Behavioural interventions
Treatment of underlying conditions such as hypothyroidism may greatly improve symptoms of OSAHS.
Non-surgical interventions
• NIV
Surgery
Cystic fibrosis
Genetics
Pathophysiology
Clinical features
Respiratory
Gastrointestinal
About 85% of patients have pancreatic insufficiency from birth, resulting in malabsorption of fat and protein, and causing steatorrhoea and malnutrition. Infants and children may present with failure to thrive, diarrhoea or acute pancreatitis. Bowel obstruction secondary to meconium ileus (10%) can occur soon after birth; if it occurs later in life, it is known as ‘meconium ileus equivalent’ or ‘distal intestinal obstructive syndrome’ (DIOS). These patients present with volvulus or rectal prolapse. Biliary obstruction may result in cholecystitis, while chronic liver disease and cirrhosis can lead to portal hypertension, varices and splenomegaly. There is an increased prevalence of gallstones (especially cholesterol), reflux oesophagitis, peptic ulceration and gastrointestinal malignancy in CF.
Diagnosis and investigations
• Positive family history.
Treatment
Antibiotics
Many patients receive IV antibiotics at home, although a test dose is usually given in hospital first. Colomycin 1–2 MU twice daily can cause bronchoconstriction, so a test dose should always be given.
Anti-inflammatory agents
Airway clearance
Respiratory complications
Extrapulmonary disease
Gastrointestinal disease
Liver disease
Endocrine disease
• Fertility
Non-pharmacological therapies
Asthma
Clinical features
Cough, wheeze, shortness of breath and chest tightness occur. These symptoms are intermittent, variable, worse at night and provoked by triggers such as exercise. Cough variant asthma is cough without a wheeze. There is often a family history of asthma or other atopic disease, such as eczema or hay fever, and patients often know triggers that worsen symptoms.
Investigations
Management
The aims of treatment are symptom control, reduction of exacerbations and restoration of normal or best possible lung function with minimal side-effects from medication, minimal absences from work or school, and no limitation on physical activity. In children treatment is to enable a normal growth pattern to occur.
Non-pharmacological therapies
Secondary prophylaxis
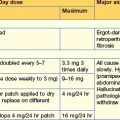
Drug treatment (Table 13.3)
| Drug | Regimen |
|---|---|
| Inhaled drugs | |
| Inhaled short-acting β2 agonists | |
| Salbutamol (called albuterol in USA) Aerosol and powder preparations available |
100 mcg per puff (metered dose) Take 2 puffs as required |
| Terbutaline Powder and nebulized solutions available |
500 mcg per puff Up to 4 times daily as required |
| Inhaled long-acting β2 agonist | |
| Formoterol Powder and aerosol formulations available |
12 mcg twice daily Up to 24 mcg twice daily |
| Salmeterol | 50 mcg (2 puffs or 1 blister) twice daily Up to 100 mcg (4 puffs or 2 blisters) twice daily |
| Inhaled corticosteroids | |
| Beclometasone dipropionate Dry (in blisters) and aerosol preparations |
50, 100 or 200 mcg per metered dose 100–400 mcg twice daily, rising to 0.4–1 mg twice daily |
| Budesonide Powder or aerosol preparations |
100, 200, 400 mcg per metered dose 100–800 mcg twice daily |
| Fluticasone propionate | 50 mcg metered dose (powder) and 125 mcg (aerosol) 100–500 mcg twice daily |
| Mometasone furoate | 200–400 mcg (powder) as a single dose in evening or in 2 divided doses |
| Compound inhaled long-acting β2 agonist and inhaled corticosteroids | |
| Budesonide and formoterol |
100/6 combination 1–2 puffs, up to 4 puffs daily (combinations in higher concentrations available 200/6 and 400/12) |
| Fluticasone and salmeterol |
100, 250 or 500 mcg 50 mcg 1–2 puffs twice daily |
| Other inhaled preventer therapy | |
| Antimuscarinic bronchodilators Ipratropium bromide Tiotropium |
(Aerosol 20–40 mcg 3–4 times daily) (Nebulized solutions 250–500 mcg 3–4 times daily) 18 mcg (powder) once daily 2.5 mcg (solution) 2 puffs once daily |
| Sodium cromoglicate | 10 mg (2 puffs) 4–8 times daily |
| Nedocromil sodium | 2 puffs (4 mg) 2–4 times daily |
| Oral agents | |
| Leukotriene modifiers | |
| Montelukast | 10 mg once daily (evening) |
| Zafirlukast | 20 mg twice daily |
| Theophylline | |
| Theophylline modified release | 200–400 mg every 12 hours (tablets) 250–500 every 12 hours (capsules) |
| Aminophylline | 225 mg (tablets) twice daily, rising to 450 mg twice daily if necessary |
| Corticosteroids | |
| Prednisolone | 5 mg tablets 30–60 mg daily for acute asthma attack |
| β2 agonists | |
| Salbutamol | 2–4 mg 3–4 times daily |
| Terbutaline | 2.5 mg 3 times daily |
| Steroid-sparing agents, e.g. methotrexate, ciclosporin | Specialist centres only |
Table 13.4 The stepwise management of asthma
| Step | PEFR | Treatment |
|---|---|---|
| 1 Occasional symptoms, less frequent than daily | 100% predicted | As-required short-acting β2 agonists If used more than once daily, move to step 2 |
| 2 Daily symptoms | ≤ 80% predicted | Regular inhaled preventer therapy Anti-inflammatory drugs: inhaled low-dose corticosteroids up to 800 mcg daily. LTRAs, theophylline and sodium cromoglicate are less effective If not controlled, move to step 3 |
| 3 Severe symptoms | 50–80% predicted | Inhaled corticosteroids and long-acting inhaled β2 agonist Continue inhaled corticosteroid Add regular inhaled LABA If still not controlled, add either LTRA, modified-release oral theophylline or β2 agonist If not controlled, move to step 4 |
| 4 Severe symptoms uncontrolled with high-dose inhaled corticosteroids | 50–80% predicted | High-dose inhaled corticosteroid and regular bronchodilators Increase high-dose inhaled corticosteroids up to 2000 mcg daily Plus regular LABAs Plus either LTRA or modified-release theophylline or β2 agonist |
| 5 Severe symptoms deteriorating | ≤ 50% predicted | Regular oral corticosteroids Add prednisolone 40 mg daily to step 4 |
| 6 Severe symptoms deteriorating in spite of prednisolone | ≤ 30% predicted | Hospital admission |
LABA, long-acting β2 agonist; LTRA, leukotriene receptor agonist; PEFR, peak expiratory flow rate.
Step 1: Mild intermittent asthma
Ipratropium bromide, an antimuscarinic bronchodilator, is used for short-term relief in chronic asthma 20–40 mcg 3–4 times daily by inhaler.
Step 2: Regular preventer therapy
Step 4: Persistent poor control
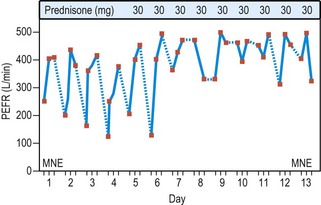
Step 5: Continuous or frequent use oral corticosteroids
Prednisolone is the oral corticosteroid of choice and should be used at the lowest dose that controls symptoms. Patients taking long-term steroids or 3–4 courses a year are at increased risk of side-effects (p. 324). Patients receiving steroids for more than 3 months should be prescribed a long-acting bisphosphonate to prevent osteoporosis. BP and blood glucose should be checked regularly. Methods of trying to decrease oral steroids include maximizing other therapy and using maximal doses of inhaled corticosteroids. Immunosuppressants (steroid-sparing agents), such as methotrexate, ciclosporin or oral gold, can be tried for 3 months.
Management of acute exacerbations of asthma
Severity of disease
Investigations
Treatment
In severe asthma not responding to the initial nebulizer:
Pneumonia
Pneumonia is an inflammation of the substance of the lungs. It can be classified by site (e.g. lobar, diffuse, bronchopneumonia) or by aetiological agent (e.g. bacterial, viral, fungal, aspiration, or due to radiotherapy or allergic mechanisms). Pneumonias can be community-acquired (CAP; commonest Strep. pneumoniae), hospital-acquired (often Gram-negative bacteria) or ventilator-associated (p. 548).
Causes
Strep pneumonia often follows a viral infection with influenza (p. 50) or parainfluenza viruses. Precipitating factors include cigarette smoking, alcohol excess, bronchiectasis, bronchial obstruction (e.g. carcinoma) or inhalation from oesophageal obstruction. IV drug users can contract a Staph. aureus infection and patients who are immunosuppressed (e.g. those having AIDS or receiving treatment with cytotoxic agents) develop pneumonia; the organisms include Pneumocystis jiroveci, Mycobacterium avium intracellulare and cytomegalovirus.
Community-acquired pneumonia (CAP)
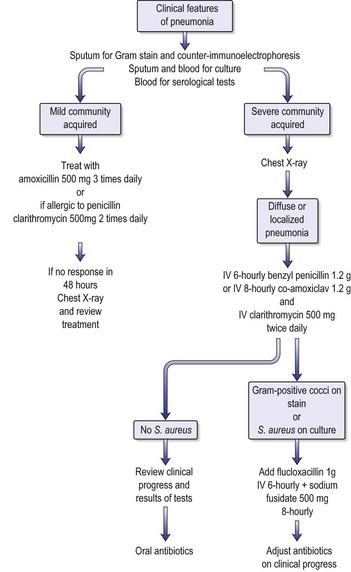
The majority of patients with CAP are treated outside hospital with amoxicillin (see Fig. 13.4) but they should be reviewed at 48 hours. If the mild case has not improved or CAP is very severe, the patient should be admitted to hospital. There is a significant mortality, particularly in those over 65 years old. Overall mortality for those admitted to hospital is about 5%.
Strep. pneumoniae accounts for the majority of cases and for two-thirds of the mortality.
Clinical features
This varies according to the infecting agent (Table 13.5) or the immune state of the patient.
Table 13.5 Clinical features of community-acquired pneumonia
| Pneumonia | Clinical features |
|---|---|
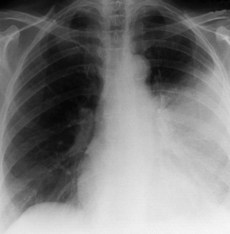
| Streptococcus pneumoniae | Patient is ill with a high temperature (39.5°C). Dry cough becomes productive, with rusty-coloured sputum after 1–2 days. Labial herpes simplex. Breathlessness. Pleuritic pain. Crackle and wheezes with signs of consolidation and pleural rub. CXR is shown in Fig. 13.3 |
| Mycoplasma pneumoniae | Common in young. Cycles of 3–4 years. Headaches and malaise often precede chest symptoms by 1–5 days. Rare extrapulmonary complications include myocarditis, pericarditis, erythema multiforme, haemolytic anaemia, meningoencephalitis. Recovery usually in 10–14 days. Can be protracted, with cough and X-ray changes lasting for weeks; relapses occur. Lung abscesses and pleural effusions rare |
| Legionella pneumophila | Sporadic or in outbreaks in e.g. hotels or foreign travel, or in immunocompromised. Middle to old age. Males > females 2 : 1. Incubation period 2–10 days. Malaise, myalgia, headache, fever (up to 40°C), rigors. Nausea, vomiting, diarrhoea, abdominal pain. Can be acutely ill with mental confusion and other neurological signs. Haematuria, occasional renal failure and deranged liver function tests. Breathlessness with initially dry cough, which can become productive and purulent. CXR slow to resolve |
| Viral pneumonias | Uncommon in adults — influenza A virus or adenovirus infection is commonest cause. May predispose patients to bacterial pneumonia Cytomegalovirus pneumonia is seen in immunocompromised patients (p. 3) Influenza A (H5N1) (p. 50) Management is as for ARDS (p. 549) |
| Other pneumonias | |
| Haemophilus influenzae | Frequent cause of exacerbation of chronic bronchitis and can cause pneumonia in COPD patients. Pneumonia is diffuse or confined to one lobe. No special features to separate it from other bacterial pneumonias |
| Staphylococcus aureus | Rarely causes pneumonia, except after preceding influenzal viral illness. Patients are very ill. Patchy consolidation in one or more lobes, which break down to form abscesses. Pneumothorax, effusion and empyemas are frequent. Septicaemia develops with metastatic abscesses in other organs |
| Staphylococcal septicaemia | Areas of pneumonia (septic infarcts) frequently seen in IV drug users, and in patients with central catheters being used for parenteral nutrition. Infected puncture site is source of staphylococcus. Pulmonary symptoms often few but breathlessness and cough occur and CXR reveals areas of consolidation. Abscess formation is frequent |
ARDS, acute respiratory distress syndrome; COPD, chronic obstructive pulmonary disease; SARS, severe acute respiratory syndrome.
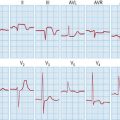
Following a radiological (Fig. 13.3) and microbiological (if possible) diagnosis of the pneumonia, an early assessment of the severity of the pneumonia must be made in order to admit the patient to a medical ward or to ICU. The CURB-65 (Box 13.3) is a useful guide for doing this.
Investigations
All hospitalized patients should have the following:
• Pneumococcal antigen
• Legionella antigen
Management
Management of CAP is shown in Fig. 13.4.
The patient in hospital should be re-evaluated regularly by the nursing staff, depending on the severity of the illness (see MEWS, p. 2).
Hospital-acquired pneumonia
Tuberculosis
TB is an AIDS-defining illness. It may arise in a patient with HIV from rapid progression of primary infection, reactivation of disease or re-infection (p. 115).
Diagnosis
Treatment (p. 86)
Drug-resistant organisms
Monitoring response to therapy
Patients with smear-positive TB should have regular (every 1–2 weeks) sputum examination for acid-fast bacilli with smear and culture. Once sputum becomes negative for acid-fast bacilli, patients should have a monthly sputum examination until culture is also negative. This is the most reliable indicator of a response to therapy. If, after 3 months of treatment, symptoms have not resolved or sputum smear or culture is still positive, either there is non-compliance with medication or drug resistance has immerged. Specialist TB nurses and health visitors should monitor patients’ compliance with treatment. If drug resistance occurs, the addition of a single drug is not recommended. If new drugs are added, at least two or preferably three should be commenced which the patient has not already received. Subsequent treatment should be fully supervised.
Chemoprophylaxis
Chemoprophylaxis is used in the following groups of patients:
Diffuse parenchymal lung disorders
Clinical features
Patients may be asymptomatic or present in one of the following ways:
Investigations
Invasive diagnostic procedures
Sarcoidosis
Diagnosis
Treatment
Mortality is usually < 5% in the UK but can be up to 10% in black Americans.
Idiopathic interstitial pneumonias (IIPs)
Idiopathic pulmonary fibrosis
Investigations (p. 516)
Hypersensitivity pneumonitis
Drugs and radiation-induced respiratory reactions
Drugs can produce a wide variety of respiratory problems. Mechanisms include direct toxicity (e.g. bleomycin), immune complex formation with arteritis, hypersensitivity and autoimmunity. TB reactivation is seen with immunosuppressive drugs, e.g. monoclonal antibodies. Table 13.6 gives some drugs and their respiratory reactions. For further interactions see www.pneumotox.com.
| Disease | Drugs |
|---|---|
| Bronchospasm | Penicillins, cephalosporins |
| Sulphonamides | |
| Aspirin/NSAIDs | |
| Monoclonal antibodies, e.g. infliximab | |
| Iodine-containing contrast media | |
| β-Adrenoceptor-blocking drugs (e.g. propranolol) | |
| Non-depolarizing muscle relaxants | |
| IV thiamine | |
| Adenosine | |
| Diffuse parenchymal lung disease and/or fibrosis | Amiodarone |
| Anakinra (interleukin-1 receptor antagonist) | |
| Nitrofurantoin | |
| Paraquat | |
| Continuous oxygen | |
| Cytotoxic agents (many, particularly busulfan, CCNU, bleomycin, methotrexate) | |
| Pulmonary eosinophilia | Antibiotics (penicillin, tetracycline) |
| Sulphonamides, e.g. sulfasalazine | |
| NSAIDs | |
| Cytotoxic agents | |
| Acute lung injury | Paraquat |
| Pulmonary hypertension | Fenfluramine, dexfenfluramine, phentermine |
| SLE-like syndrome including pulmonary infiltrates, effusions and fibrosis | Hydralazine |
| Procainamide | |
| Isoniazid | |
| Phenytoin | |
| ACE inhibitors | |
| Monoclonal antibodies | |
| Reactivation of TB | Immunosuppressant drugs, e.g. steroids |
| Biological agents, e.g. tumour necrosis factor blockers |
CCNU, chloroethyl-cyclohexyl-nitrosourea (lomustine); NSAIDs, non-steroidal anti-inflammatory drugs; SLE, systemic lupus erythematosus.
Pulmonary hypertension
Classification WHO
Clinical features and diagnosis of PH
These are mainly breathlessness, fatigue, chest pain and syncope. A similar classification to the New York scheme for heart failure (p. 417) is used for assessment.
Pulmonary embolism (PE) (pulmonary thromboembolism)
Clinical features
The revised Geneva score (Table 13.7) gives the clinical probability of a PE.
Table 13.7 Revised Geneva score for the clinical prediction of a pulmonary embolism
| Criterion | Score |
|---|---|
| Risk factors | |
| Age > 65 years | +1 |
| Previous deep venous thrombosis or pulmonary embolism | +3 |
| Surgery or fracture within 1 month | +2 |
| Active malignancy | +2 |
| Symptoms | |
| Unilateral leg pain | +3 |
| Haemoptysis | +2 |
| Clinical signs | |
| Heart rate (bpm) | |
| 75–94 | +3 |
| ≥ 95 | +5 |
| Pain on leg deep vein palpation and unilateral oedema | +4 |
| Clinical probability | |
| Low | 0–3 |
| Intermediate | 4–10 |
| High | ≥ 11 |
(Righini M, et al 2008, with permission)
Investigations
• Small/medium or recurrent emboli
 scan). This is a good initial test after measurement of D-dimers. It demonstrates ventilation/perfusion defects, i.e. areas of ventilated lung with perfusion defects. Pulmonary 99mtechnetium scintigraphy demonstrates the under-perfused areas, while a scintigram, performed after inhalation of radioactive xenon, shows no ventilatory defect. A matched defect may, however, arise with a PE that causes an infarct, or with emphysematous bullae. This test is therefore conventionally reported as a probability (low, medium or high) of PE and should be interpreted in the context of the history, examination and other investigations.
scan). This is a good initial test after measurement of D-dimers. It demonstrates ventilation/perfusion defects, i.e. areas of ventilated lung with perfusion defects. Pulmonary 99mtechnetium scintigraphy demonstrates the under-perfused areas, while a scintigram, performed after inhalation of radioactive xenon, shows no ventilatory defect. A matched defect may, however, arise with a PE that causes an infarct, or with emphysematous bullae. This test is therefore conventionally reported as a probability (low, medium or high) of PE and should be interpreted in the context of the history, examination and other investigations.• Massive pulmonary emboli
Acute treatment (See Ch. 20 p. 716)
Prevention of further emboli (p. 243)
Pleural effusion
An effusion is an excessive accumulation of fluid within the pleural space.
Causes
Clinical features
Investigations
CXR
Over 300 mL of pleural fluid can be detected on a CXR (Fig. 13.6). Small effusions can be seen as obliteration of the costophrenic angle, whilst large effusions produce a dense homogeneous shadow occupying part of the hemithorax.
Pleural aspiration
Pleural fluid analysis
• Appearance and odour
Management
Empyema
Management
Management of malignant pleural effusion
Pneumothorax
Investigations
Treatment of primary pneumothorax (see Emergencies in Medicine p. 715)
Treatment of secondary pneumothorax
Calvaley PMA, Walter P. Chronic obstructive pulmonary disease. Lancet. 2008;362:1053-1081.
Jaff MR. Management of massive and sub-massive pulmonary embolism. A scientific statement from the American Heart Association. Circulation. 2011;123:1-43.
Lim WS, et al. Defining community acquired pneumonia severity on presentation to hospital. Thorax. 2003;58:377-382.
National Collaborating Centre for Chronic Conditions. Chronic obstructive pulmonary disease. National clinical guideline on management of chronic obstructive pulmonary disease in adults in primary and secondary care. Thorax. 2004;59(Supp 1):1-232.
Nava S, Hill N. Non-invasive ventilation in acute respiratory failure. Lancet. 2009;374:250-259.
Puhan MA, Garcia-Aymerich J, Frey M, et al. Expansion of the prognostic assessment of patients with chronic obstructive pulmonary disease: the updated BODE index and the ADO index. Lancet. 2009;374(9691):704-711.
Righini M, Le Gal G, Aujesky G, et al. Diagnosis of pulmonary embolism by multidetector CT alone or combined with venous ultrasonography of the leg: a randomized non-inferiority trial. Lancet. 2008;371:1343-1352.
Schünemann H. From BODE to ADO to outcomes in multimorbid COPD patients. Lancet. 2009;374(9691):667-668.
Simonneau G, et al. Clinical classification of pulmonary hypertension. J Am Coll Cardiol. 2004;43:5S-12S.
Tapson VF. Acute pulmonary embolism. New Engl J Med. 2008;358:1037-1052.
Van De Poll T, Opal SM. Pathogenesis, treatment and prevention of pneumococcal pneumonia. Lancet. 2009;374:1543-1556.
Wedzicna JA. Choice of bronchodilator therapy for patients with COPD. NEJM. 2011;64:1167-1168.