Chapter 13 Reports
Anaesthetic Guidelines
Guidelines of the Association of Anaesthetists of Great Britain and Ireland
Immediate Post-Anaesthetic Recovery 1993
Association of Anaesthetists of Great Britain and Ireland 1993
Association of Anaesthetists of Great Britain and Ireland, 1998
Recommendations
Provision of Anaesthetic Services in Magnetic Resonance Units 2002
Summary
Recommendations
Good Practice in the Management of Continuous Epidural Analgesia in the Hospital Setting 2004
Royal College of Anaesthetists & Association of Anaesthetists of Great Britain & Ireland (www.aagbi.org/publications/guidelines/docs/epidanalg04.pdf)
OAA/AAGBI Guidelines for Obstetric Anaesthesia Services 2005
Association of Anaesthetics of Great Britain and Ireland and the Obstetric Anaesthetists Association. Revised Guidelines
Infection Control in Anaesthesia 2008
Summary
National Institute for Health and Clinical Excellence Guidelines
Guidance on the Use of Ultrasound Locating Devices for Placing Central Venous Catheters 2002
(www.nice.org.uk/nicemedia/pdf/49_English_patient.pdf)
Summary
Atrial Fibrillation: the Management of Atrial Fibrillation 2006
Ultrasound-Guided Regional Nerve Block 2009
Ultrasound-Guided Catheterization of the Epidural Space 2008
Other guidelines
Local Anaesthesia for Intraocular Surgery
Royal College of Anaesthetists and Royal College of Ophthalmologists 2001
Guidelines for Autologous Blood Transfusion
British Committee for Standards in Haematology Blood Transfusion Task Force 1997
Guidelines on Post-Exposure Prophylaxis (PEP) for Health Care Workers Occupationally Exposed to HIV
Department of Health 1997 (www.dh.gov.uk/prod_consum_dh/groups/dh_digitalassets/@dh/@en/documents/digitalasset/dh_4072980.pdf)
Cadaveric Organs for Transplantation. A Code of Practice for the Diagnosis of Brain Stem Death
Department of Health 1998 (www.dh.gov.uk/prod_consum_dh/groups/dh_digitalassets/@dh/@en/documents/digitalasset/dh_4011718.pdf)
Guidelines for the Prevention of Endocarditis
Report of the Working Party of the British Society for Antimicrobial Chemotherapy 2006 (http://jac.oxfordjournals.org/cgi/reprint/dkl121v1)
Guidelines on the Prevention of Postoperative Vomiting (POV) in Children
The Association of Paediatric Anaesthetists of Great Britain and Ireland 2007 (www.apagbi.org.uk/docs)
Consensus Guideline on Perioperative Fluid Management in Children V 1.1
Association of Paediatric Anaesthetists of Great Britain and Ireland 2007 (www.apagbi.org.uk/docs/Perioperative_Fluid_Management_2007.pdf)
British Consensus Guidelines on Intravenous Fluid Therapy for Adult Surgical Patients 2008
(www.ics.ac.uk/ downloads/2008112340_GIFTASUP\%20FINAL_31-10-08.pdf)
Association of Anaesthetists of Great Britain and Ireland. Checklist for anaesthetic machines. London: AAGBI; 1990.
Association of Anaesthetists of Great Britain and Ireland. HIV and other blood borne viruses – guidance for anaesthetists. London: AAGBI; 1992.
Association of Anaesthetists of Great Britain and Ireland. Immediate postanaesthetic recovery. London: AAGBI; 1993.
Association of Anaesthetists of Great Britain and Ireland. Recommendations for standards of monitoring during anaesthesia and recovery, 4th ed. Reproduced with the kind permission of the Association of anaesthetists of Great Britain and Ireland; 2007.
Association of Anaesthetists of Great Britain and Ireland. Peri-Operative Management of the Morbidly Obese Patient. Reproduced with the kind permission of the Association of anaesthetists of Great Britain and Ireland; 2007.
Infection control in anaesthesia. Reproduced with the kind permission of the Association of anaesthetists of Great Britain and Ireland, 2008.
Association of Anaesthetists of Great Britain and Ireland. Recommendations for the safe transfer of patients with brain injury. Reproduced with the kind permission of the Association of anaesthetists of Great Britain and Ireland; 2006.
Association of Anaesthetists of Great Britain and Ireland. Blood transfusion and the anaesthetist – red cell transfusion. Reproduced with the kind permission of the Association of anaesthetists of Great Britain and Ireland; 2008.
Association of Anaesthetists of Great Britain and Ireland. Blood transfusion and the anaesthetist – blood component therapy. Reproduced with the kind permission of the Association of anaesthetists of Great Britain and Ireland; 2005.
Association of Anaesthetists of Great Britain and Ireland. Post-anaesthetic recovery. Reproduced with the kind permission of the Association of anaesthetists of Great Britain and Ireland; 2002.
Association of Anaesthetists of Great Britain and Ireland and the British Society of Allergy and Clinical Immunology. Revised guidelines. Suspected anaphylactic reactions associated with anaesthesia. Reproduced with the kind permission of the Association of anaesthetists of Great Britain and Ireland; 4th ed., 2009.
Association of Anaesthetists of Great Britain and Ireland. A report received by Council of the Association of Anaesthetists on blood borne viruses and anaesthesia – an update. London: AAGBI; 1996.
Association of Anaesthetists of Great Britain and Ireland. Checking anaesthetic equipment 3. Reproduced with the kind permission of the Association of anaesthetists of Great Britain and Ireland; 2004.
Consent for anaesthesia. Reproduced with the kind permission of the Association of anaesthetists of Great Britain and Ireland, 2006.
Association of Anaesthetists of Great Britain and Ireland. Guidelines for the management of a malignant hyperthermia crisis. Reproduced with the kind permission of the Association of anaesthetists of Great Britain and Ireland; 2007.
Association of Anaesthetists of Great Britain and Ireland. Pre-operative assessment. The role of the anaesthetist. Reproduced with the kind permission of the Association of anaesthetists of Great Britain and Ireland; 2001.
Association of Anaesthetists of Great Britain and Ireland. The anaesthesia team. London: AAGBI; 1998.
Association of Anaesthetists of Great Britain and Ireland. Management of anaesthesia for Jehovah’s witnesses, 2nd ed. Reproduced with the kind permission of the Association of anaesthetists of Great Britain and Ireland; 2005.
Association of Anaesthetists of Great Britain and Ireland and the Obstetric Anaesthetists Association. Revised Guidelines, OAA/AAGBI guidelines for obstetric anaesthesia services. Reproduced with the kind permission of the Association of anaesthetists of Great Britain and Ireland; 2005.
Association of Anaesthetists of Great Britain and Ireland. Peri-Operative Management of the Morbidly Obese Patient. Reproduced with the kind permission of the Association of anaesthetists of Great Britain and Ireland; 2007.
Association of Anaesthetists of Great Britain and Ireland. Peri-Operative Management of the Morbidly Obese Patient. Reproduced with the kind permission of the Association of anaesthetists of Great Britain and Ireland; 2007.
Association of Anaesthetists of Great Britain and Ireland: Immediate postanesthetic recovery. Reproduced with the kind permission of the Association of anaesthetists of Great Britain and Ireland, 1993.
The anaesthesia team, 1998. Reproduced with the kind permission of the Association of anaesthetics of Great Britain and Ireland. www.aagbi.org/publications/guidelines/docs/epidanalg04.pdf. Reproduced with the kind permission of the Association of anaesthetists of Great Britain and Ireland.
British Committee for Standards in Haematology Blood Transfusion Task Force: Autologous Transfusion Working Party, Napier J.A., Bruce M., Chapman J., et al. Guidelines for autologous transfusion. II. Perioperative haemodilution and cell salvage. Br J Anaesth. 1997;78:768-771.
British Consensus Guidelines on Intravenous Fluid Therapy for Adult Surgical Patients, 2008 http://www.bapen.org.uk/pdfs/bapen_pubs/giftasup.pdf.
British National Formulary. Infective endocarditis prophylaxis. British National Formulary. 37(5.1), 1999.
Department of Health. A code of practice for the diagnosis of brain stem death including guidelines for the identification and management of potential organ and tissue donors. London: HMSO; 1998.
Department of Health. Guidelines on post-exposure prophylaxis (PEP) for health care workers occupationally exposed to HIV, 1997 www.dh.gov.uk/en/PublicationsAndStatistics/LettersAndCirculars/ProfessionalLetters/ChiefOfficerLetters/DH_4004143.
Neuroanaesthesia Society of Great Britain and Ireland and the Association of Anaesthetists of Great Britain and Ireland. Recommendations for the transfer of patients with acute head injuries to neurosurgical units. London: NSGBI/AAGBI; 1996.
NICE. Guidance on the use of ultrasound locating devices for placing central venous catheters, 2002 http://guidance.nice.org.uk/TA49/Guidance/pdf/English.
NICE. Atrial fibrillation: the management of atrial fibrillation. London: National Institute for Health and Clinical Excellence; 2006. 2006 www.nice.org.uk/CG036NICEguideline
NICE. Obesity – Guidance on the prevention, identification, assessment and manage-ment of overweight and obesity in adults and children. London: National Institute for Health and Clinical Excellence; 2006. 2006 www.nice.org.uk/CG043
NICE. Ultrasound guided catheterisation of the epidural space, 2008 http://guidance.nice.org.uk/IPG249/Guidance/pdf/English.
NICE. Antimicrobial prophylaxis against infective endocarditis in adults and children undergoing interventional procedures. London: National Institute for Health and Clinical Excellence; 2008. 2008 www.nice.org.uk/nicemedia/pdf/CG64PIEQRG.pdf
NICE. Inadvertent perioperative hypothermia. NICE clinical guideline, 2008 www.nice.org.uk/CG065.
NICE. Ultrasound guided regional nerve block. London: National Institute for Health and Clinical Excellence; 2009. 2009 http://guidance.nice.org.uk/IPG285/PublicInfo/pdf/English
O’Driscoll B.R., Howard L.S., Davison A.G. on behalf of the: British Thoracic Society: British Thoracic Society guideline for emergency oxygen use in adult patients. Thorax. 2008;63(Suppl VI):vi1-vi68.
Royal College of Anaesthetists & Association of Anaesthetist of Great Britain & Ireland. Good practice in the management of continuous epidural analgesia in the hospital setting, 2004 www.aagbi.org/publications/guidelines/docs/epidanalg04.pdf.
Royal College of Anaesthetists. Sedation and anaesthesia in radiology. In Report of a Joint Working Party. London: RCA; 1992.
Royal College of Anaesthetists and College of Ophthalmologists. Report of the Joint Working Party on Anaesthesia in Ophthalmic Surgery. London: RCA and Co, 1993.
Royal College of Anaesthetists. Standards and guidelines for general anaesthesia and dentistry. London: RCA; 1999.
Royal College of Radiologists. Making the best use of a department of clinical radiology. Guidelines for doctors, 3. RCR, London, 1995.
National confidential enquiries into perioperative deaths (NCEPOD)
NCEPOD 1991/2 – Specific Procedures
Reviewed 15 specific surgical procedures from all specialities.
Reviewed 19 816 deaths in patients aged 6–70 years.
Recommendations
NCEPOD 1993/4 – Postoperative Deaths
NCEPOD 1994/5 – Postoperative Deaths
Reviewed 1818 deaths within 3 days of surgery.
Recommendations
NCEPOD 1995/6 – Out-of-Hours Operating
Key points
Recommendations
NCEPOD 1996/7 – Specific Surgical Procedures
Reviewed 2541 deaths following specific surgical operations.
NCEPOD 1997/8 – Deaths at the Extremes of Age
Recommendations: Paediatric surgery
Recommendations: Surgery for the elderly
NCEPOD 1998/9 – One in Ten Sample of Death
Will allow comparison with the 1992 NCEPOD report which considered one in five deaths. Will be available on NCEPOD website (www.ncepod.org.uk).
Buck N., Devlin H.B., Lunn J.N. The Report of a Confidential Enquiry into Perioperative Deaths. London: Nuffield Provincial Hospitals Trust and the King Edward’s Hospital Fund for London; 1987.
Callum K.G., Gray A.J.G., Hoile R.W., et al. Extremes of Age: The Report of the National Confidential Enquiry into Perioperative Deaths 1999. London: NCEPOD; 1999.
Campling E.A., Devlin H.B., Lunn J.N. The Report of the National Confidential Enquiry into Perioperative Deaths 1989. London: NCEPOD; 1990.
Campling E.A., Devlin H.B., Hoile R.W., et al. The Report of the National Confidential Enquiry into Perioperative Deaths 1990. London: NCEPOD; 1992.
Campling E.A., Devlin H.B., Hoile R.W., et al. The Report of the National Confidential Enquiry into Perioperative Deaths 1991/2. London: NCEPOD; 1993.
Campling E.A., Devlin H.B., Hoile R.W., et al. The Report of the National Confidential Enquiry into Perioperative Deaths 1992/3. London: NCEPOD; 1995.
Campling E.A., Devlin H.B., Hoile R.W., et al. The Report of the National Confidential Enquiry into Perioperative Deaths 1995/6. London: NCEPOD; 1997.
Gallimore S.C., Hoile R.W., Ingram G.S., et al. The Report of the National Confidential Enquiry into Perioperative Deaths 1994/5. London: NCEPOD; 1997.
Gray A.J.G., Hoile R.W., Ingram G.S., et al. The Report of the National Confidential Enquiry into Perioperative Deaths 1996/7. London: NCEPOD; 1998.
Lunn J.N., Devlin H.B., Hoile R.W. The Report of the National Confidential Enquiry into Perioperative Deaths 1993/4. London: NCEPOD; 1996.
Summary of the revised guidelines for the management of massive obstetric haemorrhage
Report on Confidential Enquiries into Maternal Deaths in the United Kingdom 1994
Report on Confidential Enquiries into Maternal Deaths in the United Kingdom 1996
Reports on confidential enquiries into maternal and child health
Definitions of maternal deaths
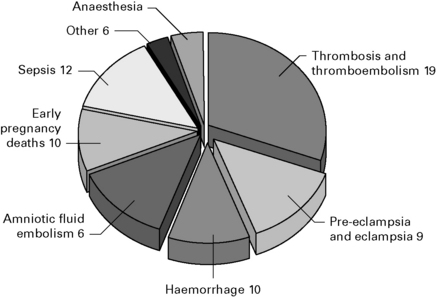
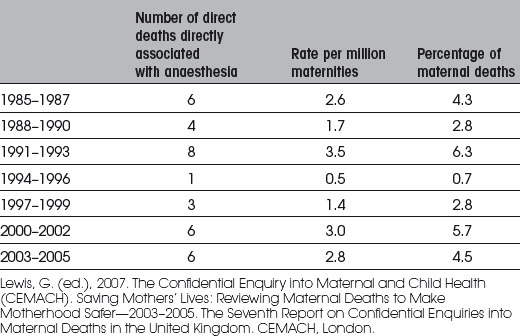
Figure 13.1 Percentage of direct deaths assessed as having substandard care by cause of death—United Kingdom: 2003–2005.
Confidential Enquiries into Maternal and Child Health (CEMACH) 2005
Confidential Enquiries into Maternal and Child Health (CEMACH). Why mothers die 2000–2002. The 6th Report of the Confidential Enquiries into Maternal Deaths in the United Kingdom, 2005. December www.cemach.org.uk
Confidential Enquiries into Maternal and Child Health (CEMACH). Saving mothers’ lives: Reviewing maternal deaths to make motherhood safer 2003–2005. The 7th Report of the Confidential Enquiries into Maternal Deaths in the United Kingdom, 2007. December www.cemach.org.uk