Repair of Urethrovaginal Fistula
Most urethrovaginal fistulas result in urinary incontinence and require surgical repair (Fig. 83–1). Rarely, a distal urethrovaginal fistula may be asymptomatic and not require repair. A nonirradiated primary fistula can usually be successfully repaired by a layered tension-free closure of the fistula (Figs. 83–2 through 83–4). If the surrounding tissue appears to be devascularized, the tissue has been irradiated, or the fistula is recurrent, it is probably best to interpose a labial fat pad between the urethra and the anterior vagina (see section on Martius Fat Pad Transposition) (Fig. 83–5). If the fistula is in the proximal urethra or at the bladder neck and the continence mechanism is thought to have been compromised, an anti-incontinence procedure, most commonly a suburethral sling, may be performed at the time of the fistula repair.
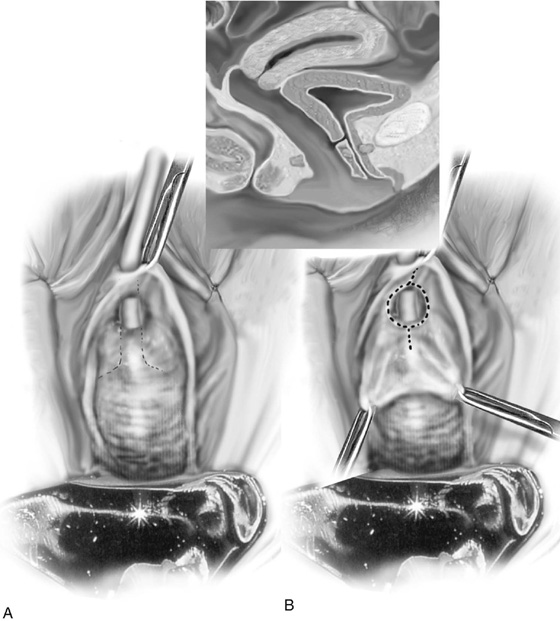
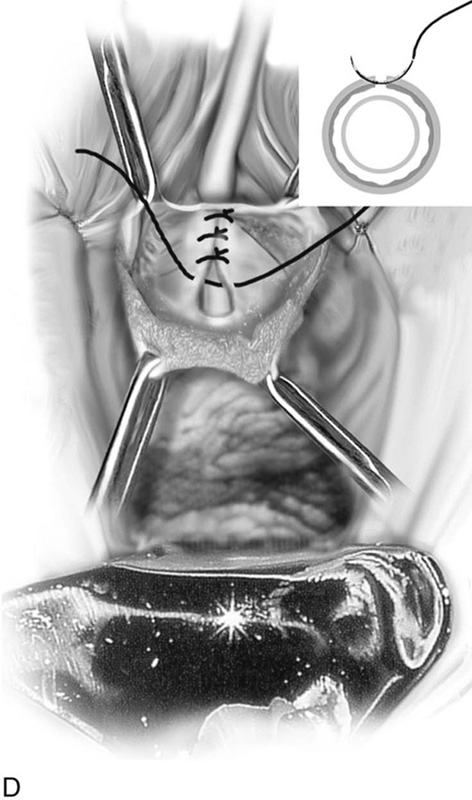
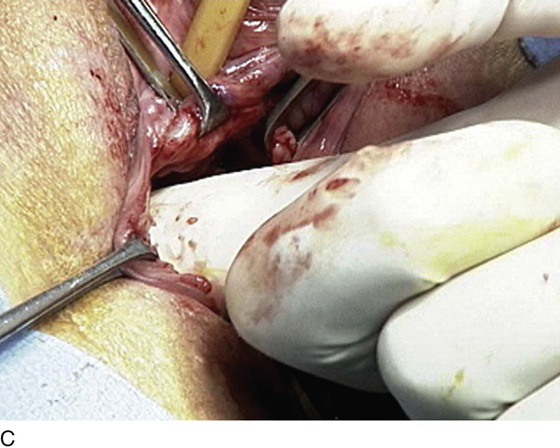
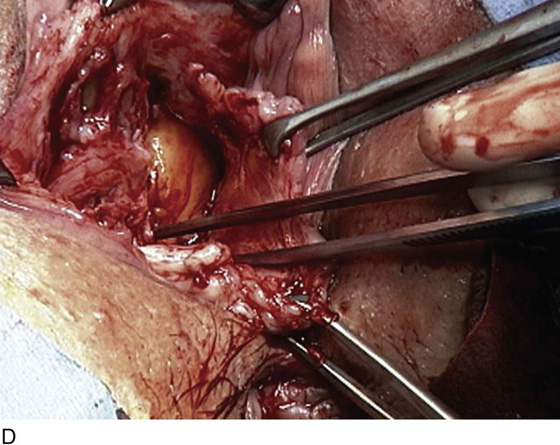
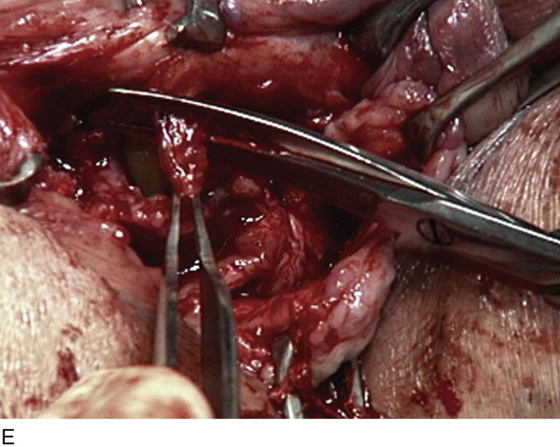
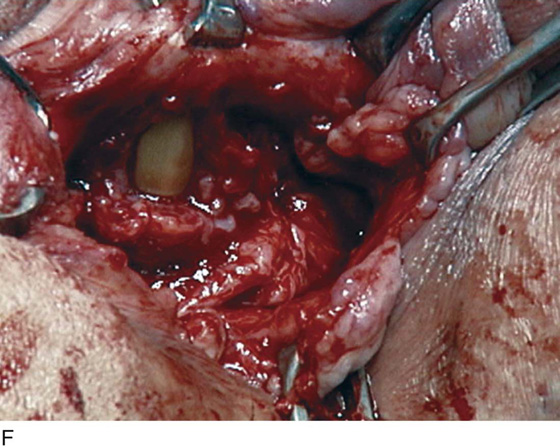
The repair begins with the placement of a transurethral Foley catheter. The anterior vaginal wall is then injected with a dilute hemostatic solution to facilitate dissection in the appropriate plane and decrease bleeding. A midline anterior vaginal wall incision or an inverted-U incision is made and extended on both sides of the urethral defect (see Fig. 83–2). The edges of the vagina are grasped with Allis clamps, and the vaginal wall is sharply separated from the underlying tissue (see Fig. 83–2C). This dissection should be extended laterally to the descending pubic rami and posteriorly until the urethra is mobilized as much as possible to allow a tension-free closure. Rarely, the retropubic space must be entered vaginally to facilitate this urethral mobility (see Fig. 83–5) (see section on Vaginal Urethrolysis). The edges of the wall of the urethra are then approximated with fine delayed absorbable interrupted sutures. The sutures should be placed in the extramucosal position (see Figs. 83–2 and 83–3). The initial suture line is then inverted with a second suture incorporating the pubocervical fascia (see Figs. 83–2E and 83–3). The vaginal incision is closed with interrupted 3-0 delayed absorbable sutures (see Fig. 83–2F). A Foley or suprapubic catheter should be left in place for 7 to 10 days.
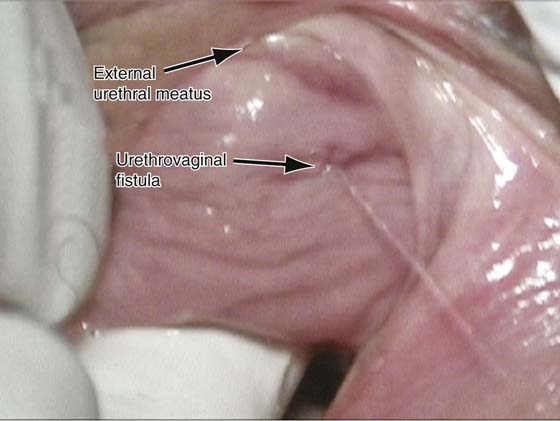
FIGURE 83–1 Urethrovaginal fistula. Note the fistula is in the midportion of the urethra, and urinary incontinence is readily demonstrated through the fistulous tract.
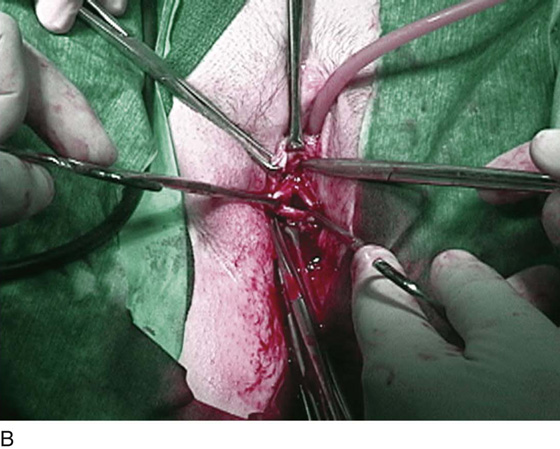
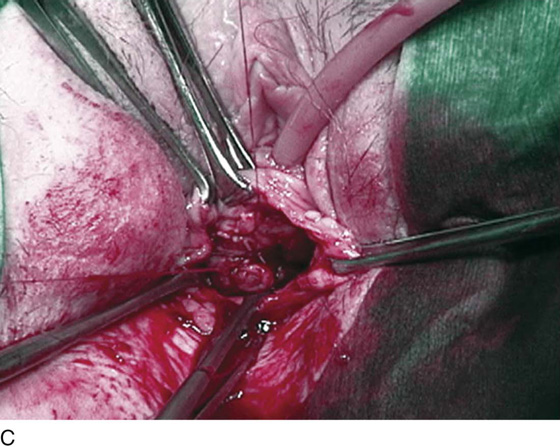
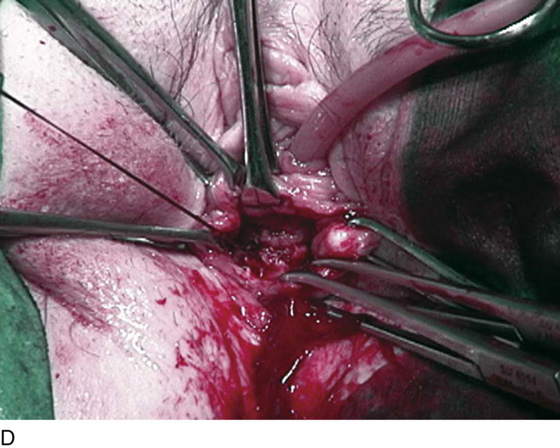
FIGURE 83–2 Repair of urethrovaginal fistula. A. Urethrovaginal fistula. B. Anterior vaginal wall incision is made and extended on both sides of the urethral defect. C. Vaginal wall is sharply separated from the underlying pubocervical fascia. D. Fine delayed absorbable interrupted sutures are placed in an extramucosal fashion. E. The initial suture line is then inverted with a second suture incorporating the pubocervical fascia. F. Vaginal incision is closed with interrupted 2-0 delayed absorbable sutures.
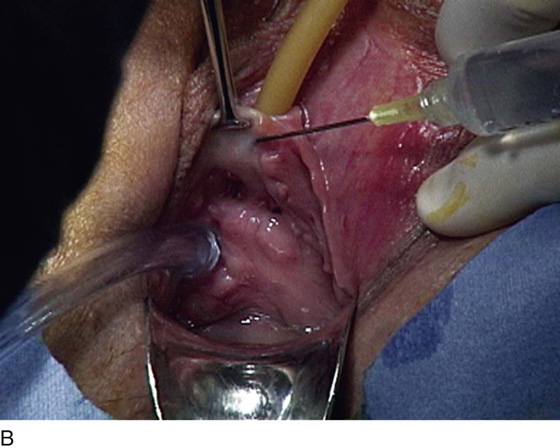
FIGURE 83–3 Urethrovaginal fistula at the level of the proximal urethra. A. A pediatric Foley catheter has been placed in the urethrovaginal fistula, and a hemostatic solution is injected to hydrodistend the anterior vaginal wall. B. The anterior vaginal wall has been dissected off the posterior wall of the urethra, and the edges of the fistula are grasped with Allis clamps. C. An initial layer of 4-0 delayed absorbable sutures has been placed in an interrupted fashion approximating the edges of the urethra mucosa. D. A second layer of 3-0 delayed absorbable sutures has been placed, imbricating the muscular portion of the wall of the urethra over the initial layer.
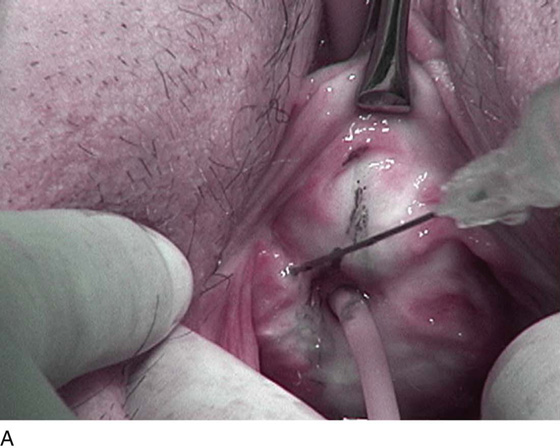
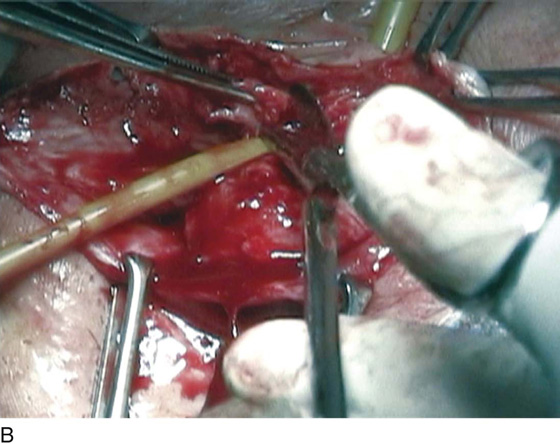
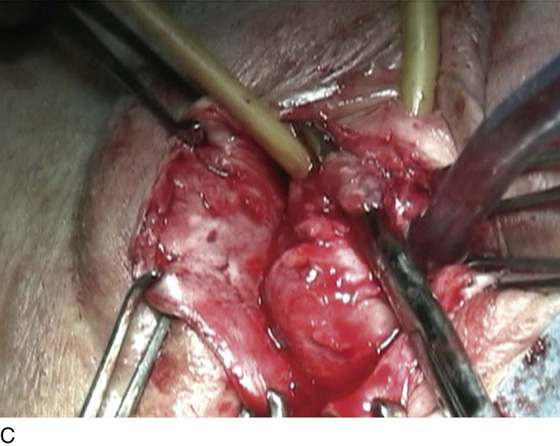
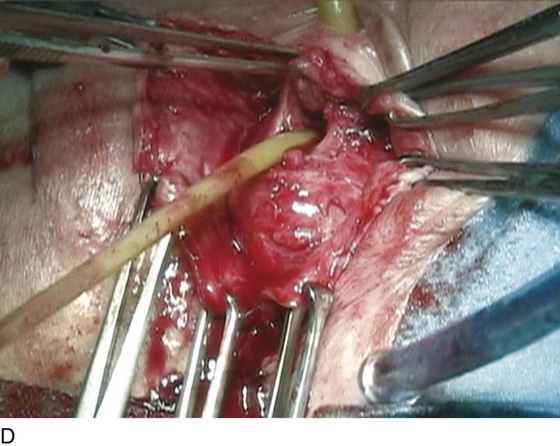
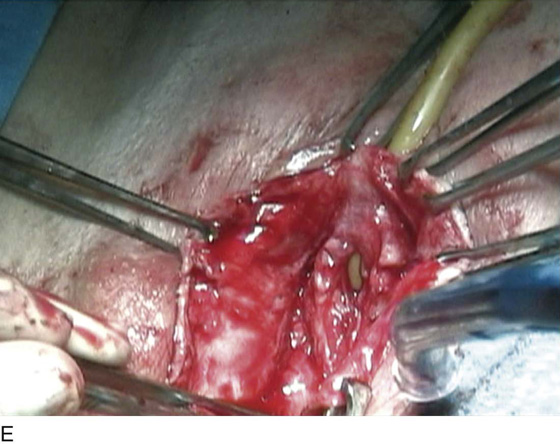
FIGURE 83–4 Repair of a recurrent urethrovaginal fistula. A. A probe has been placed in the fistulous tract. B. A Foley catheter has been placed in the fistulous tract to facilitate the dissection. Note that excessive scarification is being sharply excised from the fistulous tract. C. A bridge of devascularized tissue is noted and will be excised. D. The fistulous tract is seen after excision of all of the devascularized, scarred tissue from the previous repair. E. The healthy edges of the fistulous tract are noted and will be closed in two layers as previously mentioned.
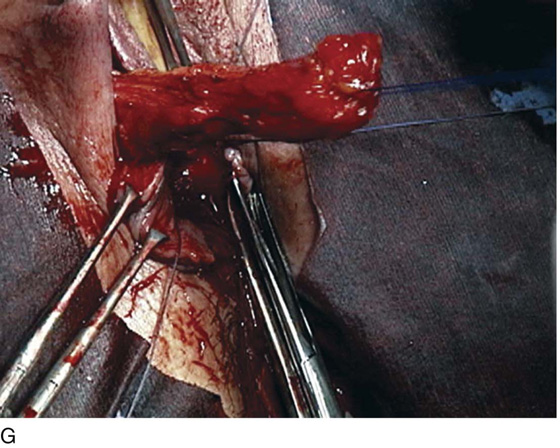
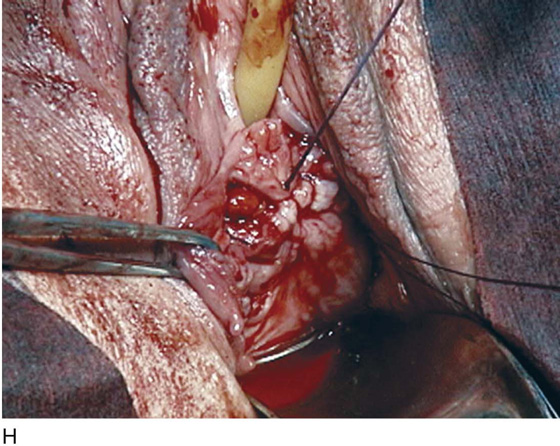
FIGURE 83–5 Recurrent, multiple urethrovaginal fistulas are noted in a 27-year-old female. A. Probes are passed through two fistulous tracts. B. The anterior vaginal wall is injected with a hemostatic solution to be used for hydrodistention. C. An inverted-U incision has been made on the anterior vaginal wall, and the dissection is being extended laterally to the inferior pubic ramus. Because this is a recurrent case, the urethra must be completely mobilized, and thus the retropubic space will be entered on each side of the urethra. D. The retropubic space has been entered on the left side. Note the retropubic fat is seen. E. The scarred bridge of tissue between the fistulous tracts is being excised. F. The scar tissue has been excised, and the defect in the urethra is noted with fresh vascular edges of urethral tissue present. G. The fistulous tract has been closed in two layers as previously mentioned. Because this is a recurrent case, a Martius fat pad has been transposed and brought into the field to be placed between the repaired urethra and the anterior vaginal wall. H. The anterior vaginal wall has been mobilized and is being closed with 3-0 delayed absorbable sutures, thus completing the repair.