Repair of Rectovaginal Fistulas
Most rectovaginal fistulas seen by the obstetrician/gynecologist are secondary to obstetric injury. These fistulas are usually in the distal third of the vagina. The key to successful repair of a rectovaginal fistula is excision of the fistulous tract with tension-free approximation of the edges of the defect. There should be excellent hemostasis, and perioperative antibiotics should be administered to decrease any potential for infection.
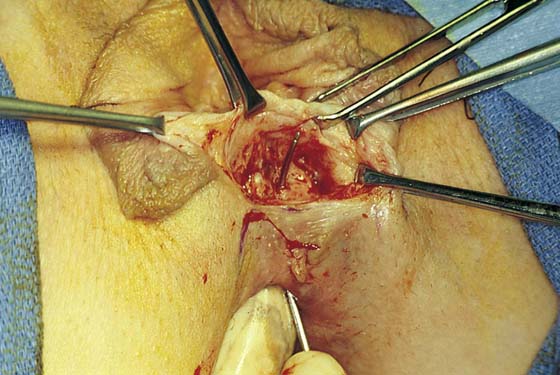
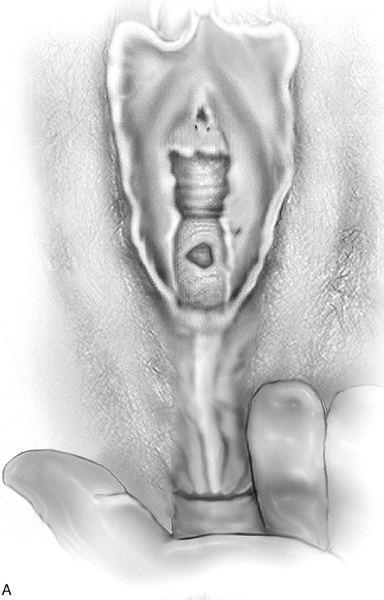
Most fistulas are easily visualized and can be palpated on rectovaginal examination. At times, the passage of a probe helps delineate the fistula and its tract (Fig. 99–1).
Following is a description of a repair of a primary nonirradiated rectovaginal fistula:
1. The surgeon’s nondominant index finger is placed in the rectum to aid in identification of the fistula and to assess the extent of scarification. A rectal finger will also facilitate dissection in the appropriate plane.
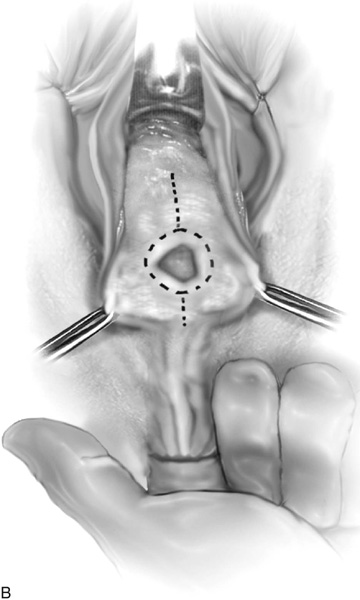
2. The initial incision depends on the anatomic location of the fistula. Many fistulas are best approached with an inverted-U perineal incision (Fig. 99–2). This allows easy mobilization of the posterior vaginal wall from the anterior rectal wall, as well as rebuilding of the perineal body. If the external anal sphincter is intact, there is no reason to disrupt it. If the fistula is higher in the vagina and the perineum is intact, an incision can be made directly into the posterior vaginal wall over and around the fistula.
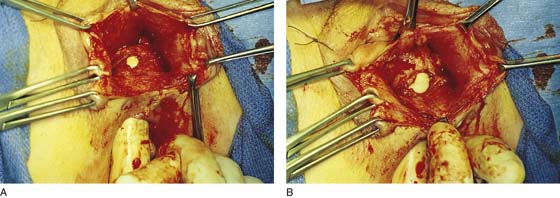
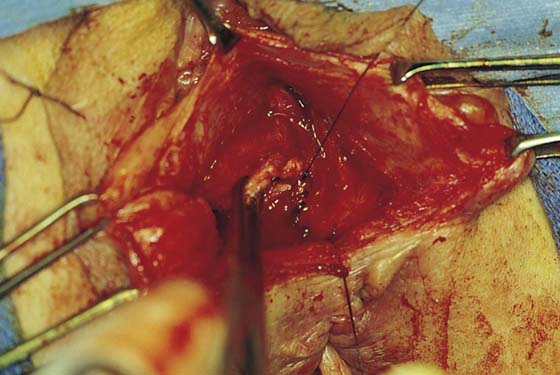
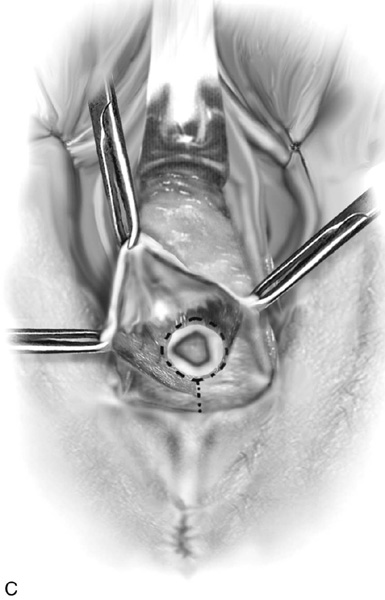
3. With traction of the vaginal wall and a finger in the rectum to provide support of the rectal wall, sharp dissection is used to widely mobilize the posterior vaginal wall from the anterior rectal wall (Figs. 99–3 and 99–4).
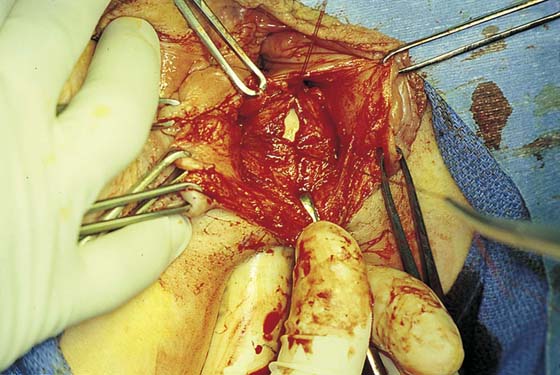
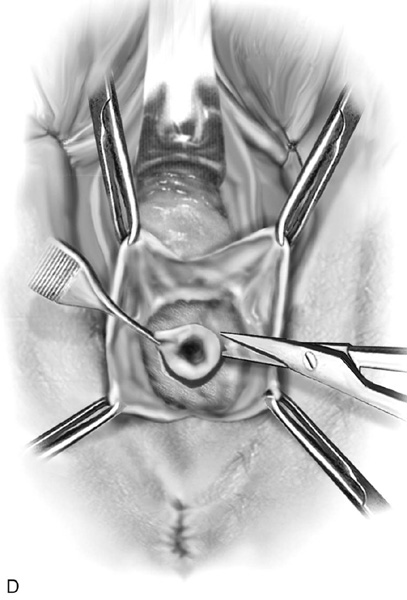
4. Once the vaginal walls are widely mobilized from the underlying rectum, the entire fistulous tract is excised. After the scar tissue is removed, the defect in the anterior rectal wall will enlarge. The rectal wall is cut back until fresh edges are encountered (see Fig. 99–4).
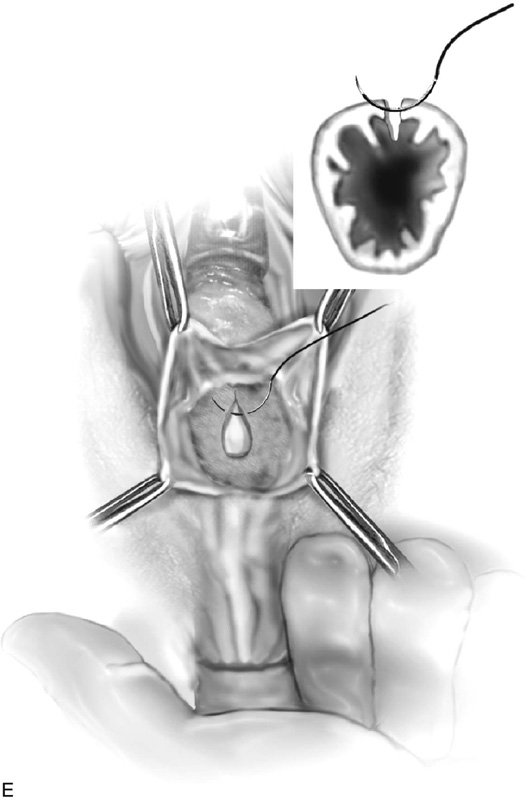
5. With the surgeon’s index finger elevating the anterior rectal wall, an initial row of 3-0 or 4-0 absorbable sutures is placed (Fig. 99–5). These sutures are best placed extramucosally and should include a portion of the muscularis and submucosa.
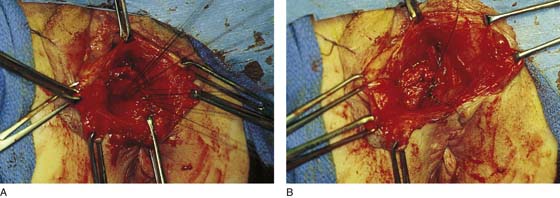
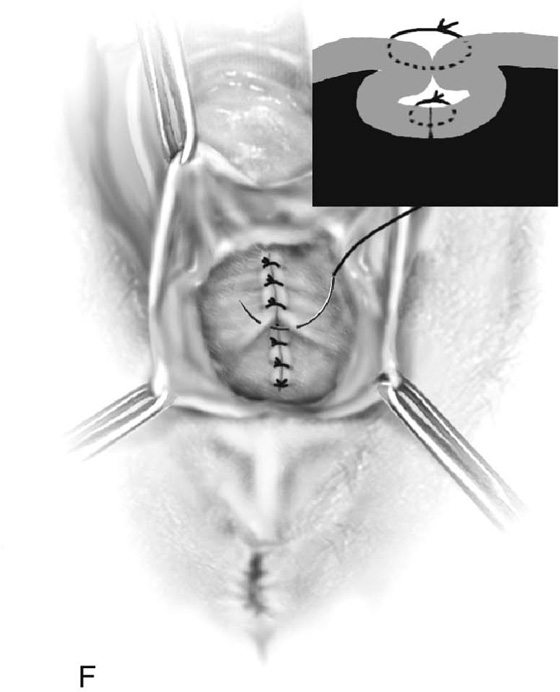
6. A second layer of inverted sutures is then placed (Fig. 99–6). This inverts the first suture line into the rectum; ideally, no suture penetrates the rectal lumen.
7. If possible, a third layer of sutures is placed by plicating the fascia of the posterior vaginal wall over the rectal closure (Fig. 99–7).
8. The vaginal skin is closed, and the perineum is reconstructed if necessary (Fig. 99–8).
Fig. 99–9 reviews the steps for rectovaginal fistula repair with an intact perineum.
FIGURE 99–1 Example of a rectovaginal fistula in which a probe helps delineate the fistula and its tract, which notes a very distal fistula opening at the posterior fourchette.
FIGURE 99–2 Usually an inverted-U incision is made on the perineum for distal fistulas. If the external anal sphincter is intact, there is no reason to disrupt it.
FIGURE 99–3 Sharp dissection with a finger in the rectum exposes the fistulous tract and begins development of the rectovaginal space.
FIGURE 99–4 A. Sharp dissection completely mobilizes the posterior vaginal wall from the anterior rectal wall. The dissection must be extended well beyond the edges of the fistula to provide tension-free closure. B. Note that the fistula will enlarge as more scar tissue is excised.
FIGURE 99–5 Once the dissection is completed and the scarred edges of the fistulous tract have been excised, closure of the anterior rectal wall is initiated with a fine absorbable suture. The author prefers a 4-0 chromic catgut suture. The distal and proximal edges of the fistula have been tagged. Sutures should be passed extramucosally if at all possible.
FIGURE 99–6 A. The initial layer of interrupted extramucosal sutures has been passed, approximating the anterior rectal wall. B. This layer is followed by a second layer of imbricating sutures.
FIGURE 99–7 The rectovaginal fascia is identified and grasped with an Allis clamp. If possible, this tissue is then approximated over the initial closure of the fistula.
FIGURE 99–8 The posterior vaginal wall is closed and the perineum is reconstructed if necessary.
FIGURE 99–9 Rectovaginal fistula repair in a patient with an intact perineum. A. A rectovaginal fistula present in the midportion of the posterior vaginal wall. B. The dashed line demonstrates the site of the posterior vaginal wall incision. C. The vaginal wall is mobilized off the anterior rectal wall. D. The fistulous tract is excised. The rectal wall is cut back until fresh edges are encountered. E. Extramucosal closure of the anterior rectal wall with interrupted fine delayed absorbable sutures. F. The second layer imbricates the muscular portion of the wall of the rectum over the initial layer. The repair is completed by plicating the rectovaginal fascia and closing the posterior vaginal wall.