Repair of Advertent and Inadvertent Cystotomy
Opening and Closing the Bladder
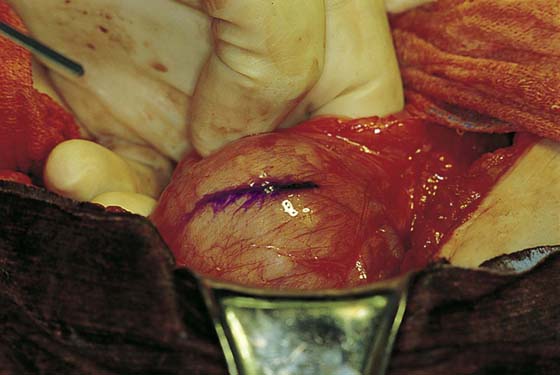
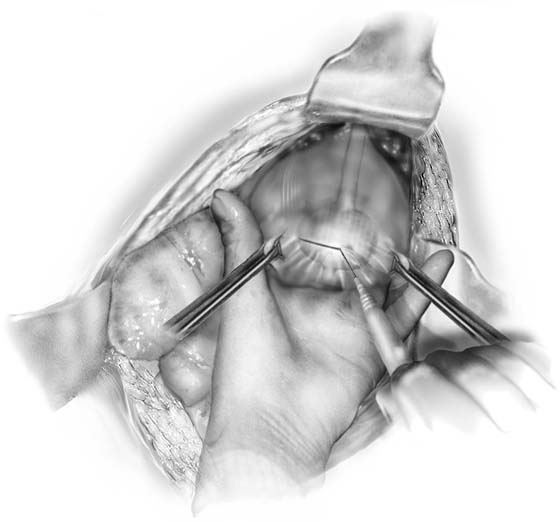
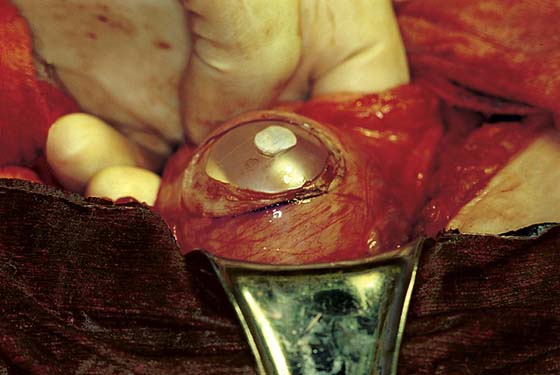
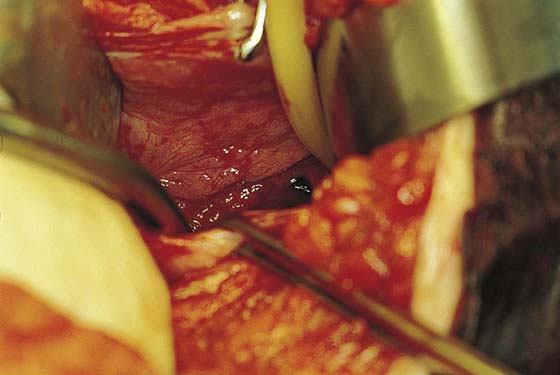
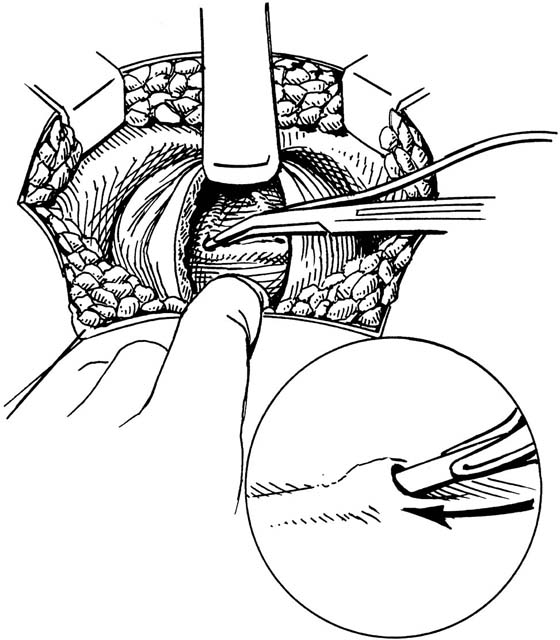
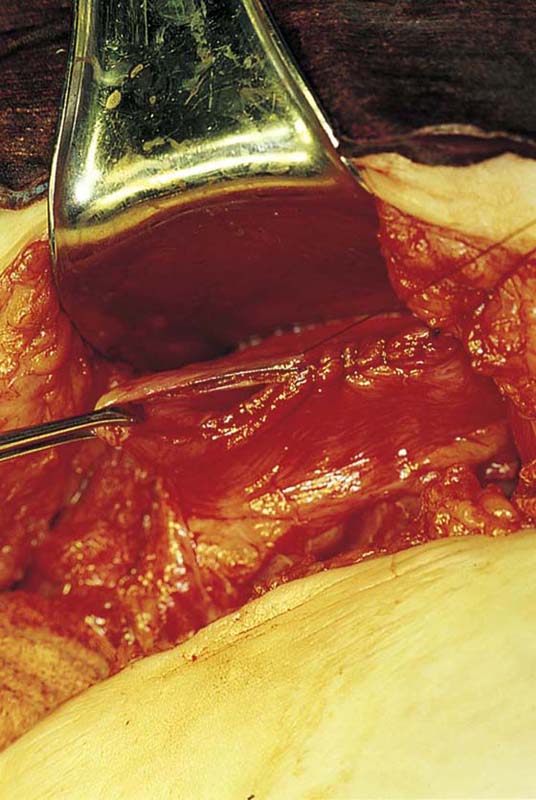
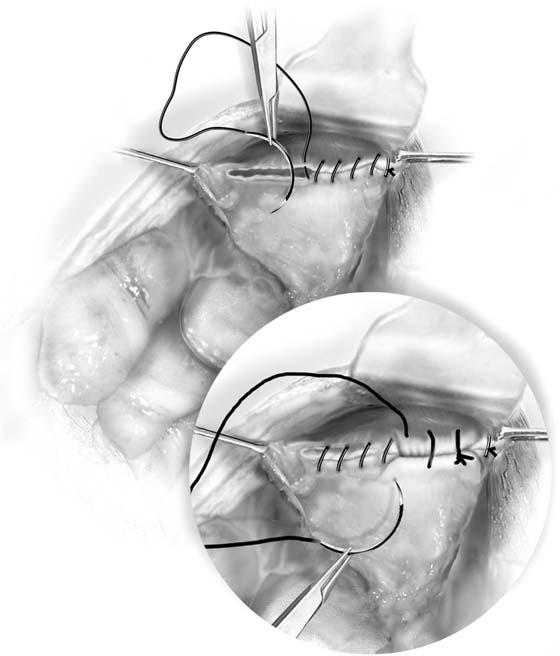
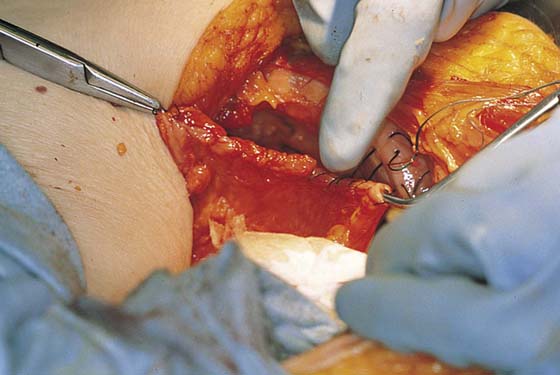
When performing abdominal surgery, the surgeon may encounter pelvic pathology that involves the lower urinary tract. The gynecologist should be comfortable with performing a cystotomy to assist in dissection of the bladder off pelvic organs such as the uterus or possibly off the back of the symphysis pubis in cases of retropubic urethropexy. Also, when ureteral injury has potentially occurred, it is reasonable to make a high cystotomy to assess ureteral patency. Making an incision into the urinary bladder is best done high up in the extraperitoneal portion of the dome of the bladder. An easy way of doing this is to mobilize the balloon of the Foley catheter up into the dome of the bladder (Fig. 88–1), go to the extraperitoneal portion of the dome of the bladder, and using cautery or a knife incise down onto the balloon until the bladder is penetrated (Figs. 88–2 and 88–3). Through a 4- to 5-cm incision in the dome of the bladder, one can assess the inside of the bladder for any potential suture penetration or injury and can visualize the ureteral orifices to ensure ureteral patency (Fig. 88–4). Also, if indicated, a ureteral stent or pediatric feeding tube can be passed in a retrograde fashion (Fig. 88–5). Ureteral stent placement may be very helpful when pelvic pathology such as endometriosis, pelvic inflammatory disease, or a pelvic mass distorts or involves the pelvic ureter. To close the bladder, delayed absorbable 3-0 sutures are utilized. The author prefers to use chromic catgut suture as it does not tear through the tissue and its short time of absorption will never allow stone formation. The first layer is a continuous suture that approximates the vesical mucosa (Figs. 88–6 and 88–7). A second layer is then placed to imbricate the muscular portion of the wall of the bladder over the mucosal closure (see Figs. 88–7 and 88–8). This is usually performed with a 3-0 absorbable suture in a continuous or an interrupted fashion.
Repair of Bladder Lacerations
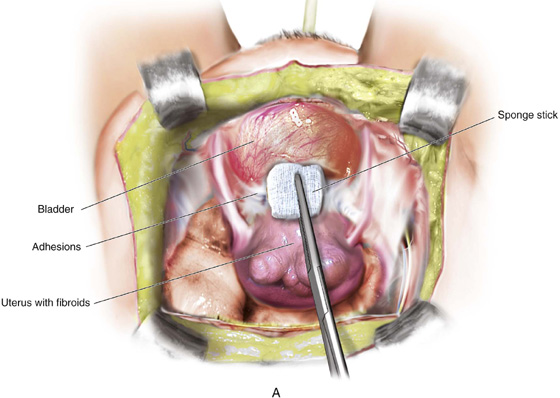
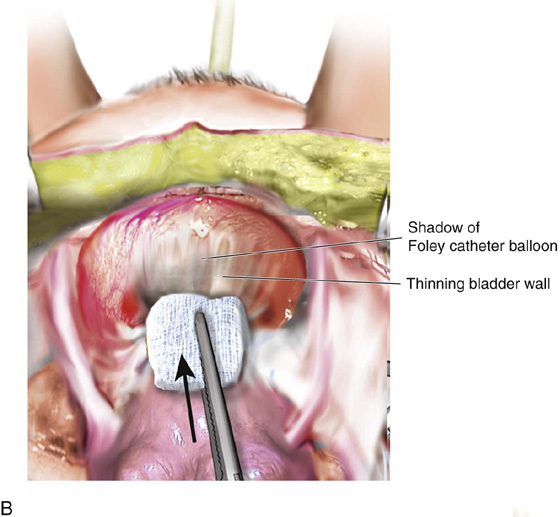
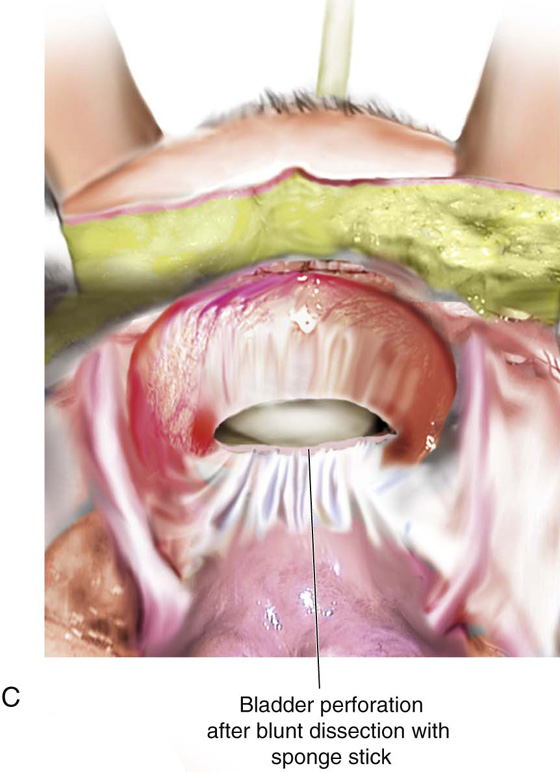
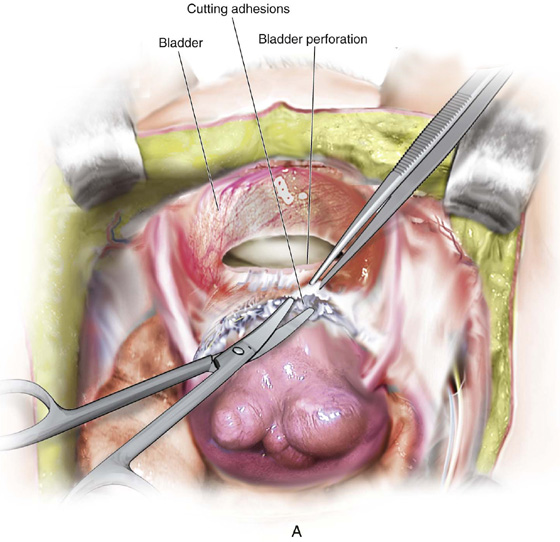
Even with extensive surgical expertise, injury to the urinary tract does occur. Most injuries to the bladder occur during abdominal hysterectomy, cesarean section, or retropubic urethropexy. When injury occurs, it is important to differentiate low intraperitoneal injury from high extraperitoneal injury. When a low intraperitoneal injury occurs, the injured bladder needs to be completely mobilized from surrounding tissue and closed in layers under no tension. On the other hand, a high extraperitoneal cystotomy utilizes the technique discussed in the previous section on opening and closing the bladder. With an increasing number of women undergoing cesarean section, it is relatively common to encounter some adhesions between the lower uterine segment and the bladder when performing a hysterectomy. For this reason, it is important to utilize sharp dissection when mobilizing the bladder off the lower uterine segment. Fig. 88–9 demonstrates how utilizing blunt dissection with a sponge stick in a patient with dense adhesions can at times result in an inadvertent tear into the bladder. Figure 88–10 demonstrates how sharp dissection allows appropriate mobilization of the base of the bladder off the lower uterine segment. This then allows a tension-free closure of inadvertent cystotomy. Figure 88–11 demonstrates how blunt finger dissection at the time of vaginal hysterectomy can result in an inadvertent cystotomy.
The duration of bladder drainage after cystotomy depends on the position and extent of the cystotomy. In general, high extraperitoneal cystotomies in a nondependent portion of the bladder require very little drainage time, whereas low intraperitoneal cystotomies in a dependent portion of the bladder usually require 7 to 10 days of bladder drainage. This can be performed via a suprapubic catheter or a transurethral catheter.
FIGURE 88–1 The balloon of the Foley catheter is mobilized into the extraperitoneal portion of the dome of the bladder in preparation for cystotomy. A line has been drawn to indicate the location and size of the cystotomy.
FIGURE 88–2 Drawing showing the use of electrocautery to perform cystotomy.
FIGURE 88–3 Cystotomy has been made over the elevated Foley balloon in the extraperitoneal portion of the dome of the bladder.
FIGURE 88–4 The inside of the bladder is being assessed through the cystotomy. Note that the Foley catheter has been pulled up through the cystotomy, and intravesical placement of a small Deaver or malleable retractor aids in visualization of the lower portion of the bladder, trigone, and ureteral orifices. Dye-colored urine is seen effluxing from the left ureteral orifice.
FIGURE 88–5 Technique of retrograde passage of a ureteral stent or pediatric feeding tube through a high cystotomy. (From Walters MD, Karram MM: In Urogynecology and Reconstructive Pelvic Surgery, 2nd ed. St Louis, Mosby, 1999, with permission.)
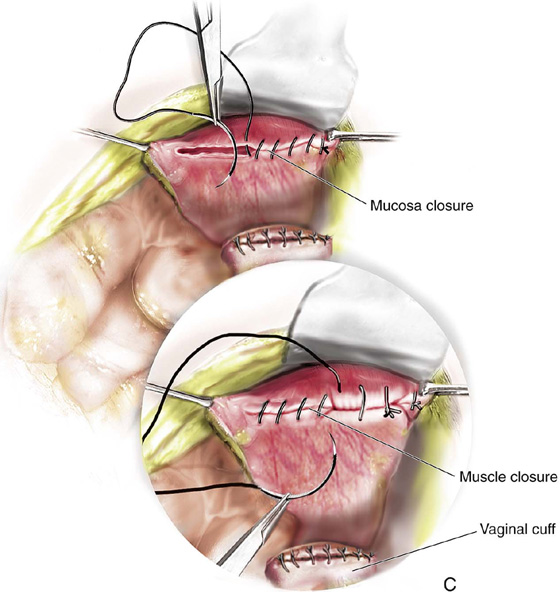
FIGURE 88–6 Closure of a high cystotomy. Continuous 3-0 absorbable through-and-through suture in the bladder mucosa is being placed as the first layer of closure of a high cystotomy.
FIGURE 88–7 Technique of two-layer closure of a high cystotomy. Note that the first layer is a running through-and-through suture that approximates the mucosa, and the second layer is a running suture that imbricates the bladder muscularis.
FIGURE 88–8 The second layer of bladder closure demonstrating imbricating of the muscularis.
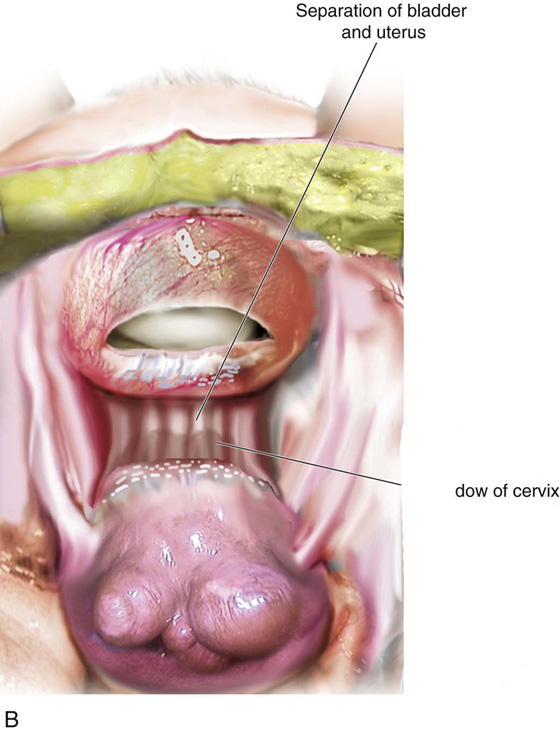
FIGURE 88–9 A. Blunt dissection using a sponge stick is being performed at the time of an abdominal hysterectomy in a patient with dense adhesions between the base of the bladder and the lower uterine segment. B. As the sponge stick is aggressively advanced, it thins the wall of the bladder because this is the area of least resistance. C. The end result of inadvertent cystotomy due to aggressive blunt dissection with a sponge stick.
FIGURE 88–10 A. Sharp dissection is used to appropriately mobilize the base of the bladder off the lower uterine segments. B. Once the bladder is completely mobilized, a tension-free layered closure of the inadvertent cystotomy is performed (C).
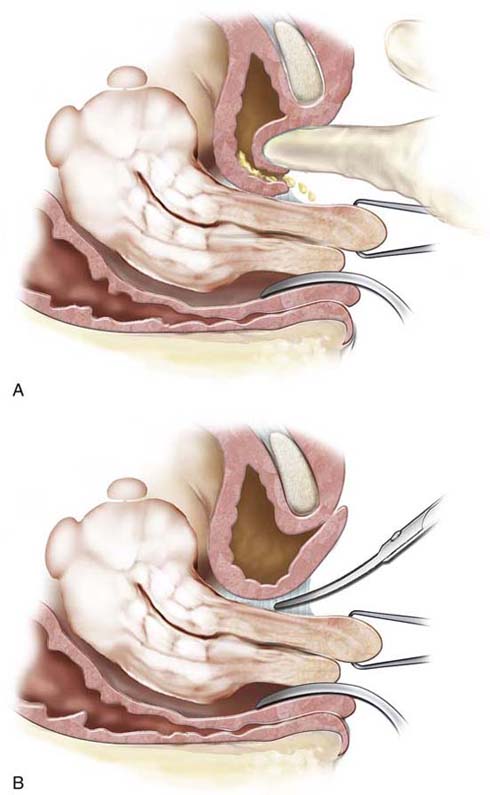
FIGURE 88–11 A. Blunt finger dissection utilized at the time of vaginal hysterectomy can result in an inadvertent cystotomy. B. Sharp dissection with scissors should be utilized to initially mobilize the base of the bladder off the lower uterine segment, allowing entrance into the vesicouterine space.