Renal Anatomy and Physiology
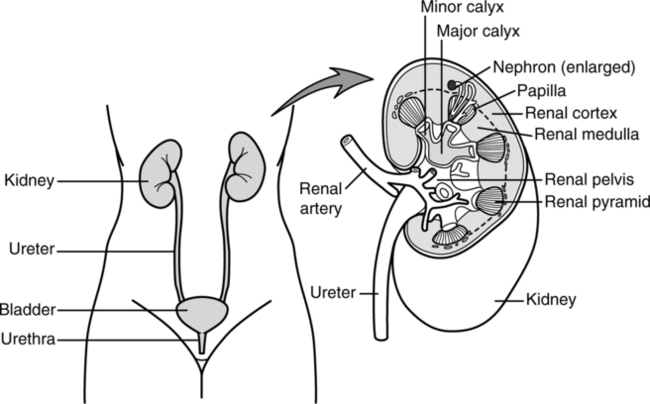
A The kidneys are located outside the peritoneal cavity on each side of the spinal column within the posterior abdominal wall.
B Renal vessels and nerves enter on the medial border.
C A single ureter that conducts urine to the bladder exits each kidney from the medial border.
D A single urethra leaves the bladder.
E The renal pelvis is a continuation of the ureter and forms the urine-collecting area of each kidney.
1. The outer border of the renal pelvis is divided into major calices.
2. Each major calyx is further subdivided into minor calices.
3. Each minor calyx is formed about a renal pyramid.
4. Nephrons, the functional aspect of the kidney, are located within each renal pyramid (Figure 13-2).
F A dissection of the kidney from top to bottom demonstrates two major regions:
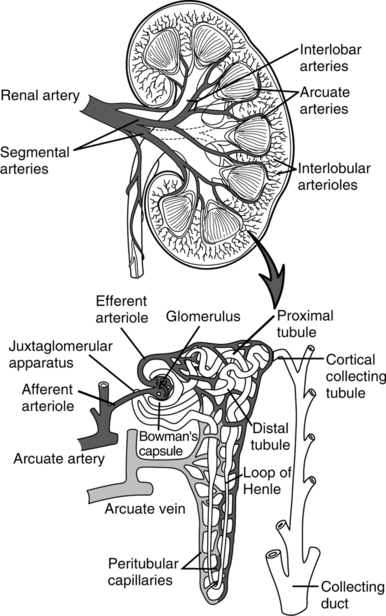
A The nephron is the functional unit of the kidney.
B Each kidney is composed of approximately 1.3 million nephrons.
C Each nephron is composed of a kidney tubule and its corresponding blood supply.
D The site of initial formation of urine is the glomerulus. The glomerulus filters blood into Bowman’s capsule, forming the glomerular filtrate.
E The kidney tubule itself begins with Bowman’s capsule and continues sequentially with the following structures:
F The arcuate artery provides the circulatory supply of the nephron.
1. This artery becomes the interlobular artery, which leads to an afferent arteriole leading to the glomerulus.
2. Blood exits the glomerulus via an efferent arteriole.
3. The efferent arteriole forms the peritubular capillaries, which intertwine about the distal and proximal convoluted tubules.
4. The efferent arterioles also form the vasa recta, a long looping capillary that forms about the loop of Henle.
5. Blood leaves the peritubular capillaries and the vasa recta via the interlobular veins and then the arcuate veins.
III Major Functions of the Kidney
A The primary function of the kidney is twofold:
1. Excretion of end products of bodily metabolism
2. Control of the concentration of constituents of the body fluids
B These primary functions are performed by a number of interrelated processes.
1. Filtration: Formation of the glomerular filtrate (see Section IV, Glomerular Filtration)
2. Tubular reabsorption (see Section V, Tubular Reabsorption)
3. Tubular secretion (see Section VI, Tubular Secretion)
4. Renin secretion (see Section XI, Renin-Angiotensin)
5. Erythropoietic factor secretion: In the presence of hypoxemia, the kidney secretes erythropoietic factor, which stimulates red blood cell production.
6. Activation of vitamin D: Vitamin D is necessary for appropriate absorption of calcium via the gastrointestinal tract.
7. Gluconeogenesis: The formation of glucose from fats and protein during periods of significant physiologic stress.
A Filtration of fluid and electrolytes at the glomerulus follows Starling’s law of fluid exchange (see Chapter 14).
B However, because protein is poorly filterable across the glomerulus, except under pathologic conditions, only three forces normally control fluid exchange.
| 1. | Forces moving fluid out of the glomerulus | |
| Glomerular hydrostatic pressure | 60 mm Hg | |
| Total outward force | 60 mm Hg | |
| 2. | Forces maintaining fluid in the glomerulus | |
| Glomerular colloid osmotic pressure | 32 mm Hg | |
| Bowman’s capsule hydrostatic pressure | +18 mm Hg | |
| Total inward force | 50 mm Hg | |
| 3. | Net filtration pressure | |
| Total outward force | 60 mm Hg | |
| Total inward force | −50 mm Hg | |
| Filtration pressure | 10 mm Hg |
C In the average adult approximately 125 ml/min of fluid is filtered across the glomerulus.
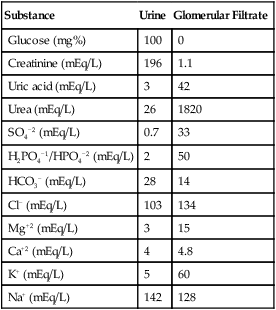
D This filtrate is essentially protein free and has concentrations of dissolved crystalloids similar to that of plasma (Table 13-1).
TABLE 13-1
Approximate Concentrations of Substances in the Glomerular Filtrate and in the Urine
| Substance | Urine | Glomerular Filtrate |
| Glucose (mg%) | 100 | 0 |
| Creatinine (mEq/L) | 196 | 1.1 |
| Uric acid (mEq/L) | 3 | 42 |
| Urea (mEq/L) | 26 | 1820 |
| SO4−2 (mEq/L) | 0.7 | 33 |
| H2PO4−1/HPO4−2 (mEq/L) | 2 | 50 |
| HCO3− (mEq/L) | 28 | 14 |
| Cl− (mEq/L) | 103 | 134 |
| Mg+2 (mEq/L) | 3 | 15 |
| Ca+2 (mEq/L) | 4 | 4.8 |
| K+ (mEq/L) | 5 | 60 |
| Na+ (mEq/L) | 142 | 128 |
E The kidney receives approximately 20% of the cardiac output, of which approximately 55% is fluid.
1. If cardiac output is 5.5 L, 1.1 L perfuses the kidney each minute.
2. Fifty-five percent of 1.1 L is 605 ml/min of fluid.
3. From this fluid volume, 125 ml/min of glomerular filtrate is formed.
4. The glomerular filtration fraction is the percent of the plasma volume filtered:
< ?xml:namespace prefix = "mml" />

5. Normally 20% of the fluid presented to the kidney is filtered.
F Alterations in the tone of the afferent arteriole and the efferent arteriole affect the volume of glomerular filtrate formed.
V Tubular Reabsorption: The movement of filtered substances back into the bloodstream
A Of the 125 ml/min of glomerular filtrate formed, only 1 ml/min of urine is formed; the remainder is reabsorbed. Normally urinary output is approximately 40 to 60 ml/hr.
B Reabsorption occurs via simple diffusion, facilitated diffusion, and active transport mechanisms (see Chapter 14).
C The vast majority of the electrolytes in the glomerular filtrate are reabsorbed (see Table 13-1).
D All filtered glucose is reabsorbed unless the blood glucose level is >375 mg/dl (mg%), the threshold for the spillage of glucose in the urine.
E Approximately 50% of the urea filtered is reabsorbed.
F Little of the creatinine and creatine filtered is reabsorbed.
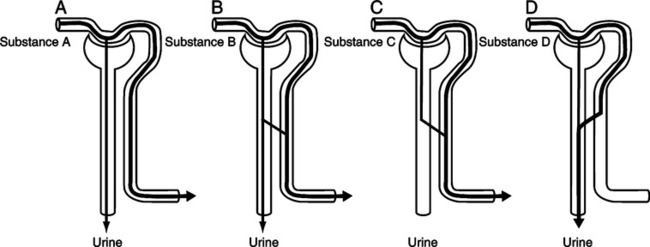
A Tubular secretion is the movement of substances from the blood into the kidney tubule.
B The following substances are secreted into the kidney tubule:
C The urinary excretion rate of a substance is equal to its filtration rate: its reabsorption rate + its secretion rate.
D Figure 13-4 depicts the potential outcome of all substances in the blood as they pass through the kidney.
A Clearance of a substance refers to the volume of plasma cleared of the substance per unit time.
B Every substance in the blood has its own clearance rate.
C Renal clearance of a substance is equal to the glomerular filtration rate (GFR) if the substance is:
D Renal clearance is equal to:
 (1)
(1)E Normally renal clearance is determined from a 24-hour urine sample.
F Inulin, an inert polysaccharide, is the standard to determine the GFR because its renal clearance is equal to the GFR.
G Clinically plasma creatinine and urea levels are used as indicators of GFR changes.
1. Creatinine results from the breakdown of voluntary muscle. As muscle breaks down, creatine is produced, which is converted to creatinine in the blood.
2. Urea is produced from the metabolism of amino acids.
3. Plasma creatinine levels are indirectly affected by the GFR.
4. All creatinine filtered is excreted.
5. A small quantity of creatinine also is secreted.
6. Plasma concentration of creatinine is usually approximately 1.3 mEq/L but can increase 10-fold during renal failure.
7. Plasma concentration of urea is 26 mEq/L and may increase to 200 mEq/L during renal failure.
8. Thus as the GFR decreases, the plasma creatinine and urea levels increase.
9. Plasma concentrations of creatinine are affected by the following:
10. Plasma concentrations of urea are affected by the following:
VIII Counter Current Multiplier
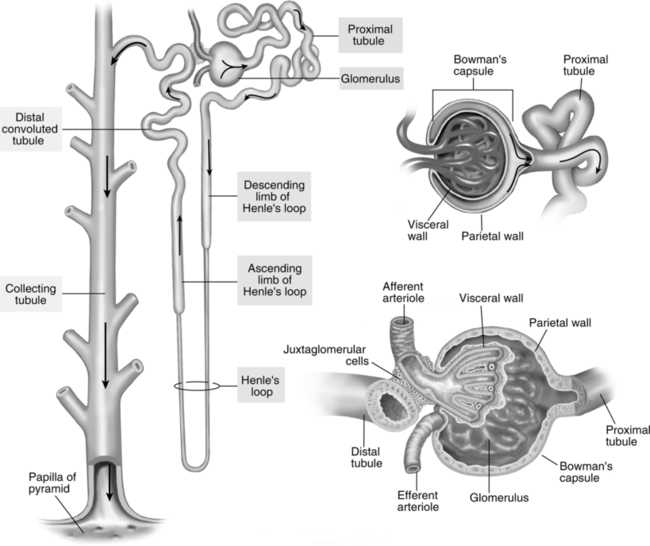
A The configuration of the nephron allows for the concentrating of urine.
B In the descending limb of the loop of Henle, water is reabsorbed. However, Na+ and Cl− are not reabsorbed. Thus the concentration of the filtrate increases toward the tip of the nephron.
C In the ascending limb of the loop of Henle, Na+ and Cl− are reabsorbed. However, water is not reabsorbed. Thus the concentration of the filtrate decreases toward the top of the loop of Henle.
D This arrangement causes a variation in the osmolarity of the interstitium from the top to the bottom of the loop of Henle. This variation is maintained by the arrangement of the circulatory system.
E The collecting duct passes through the interstitium parallel to the loop of Henle. As a result, fluid moving through the collecting duct can be concentrated if the permeability of the collecting duct to water and Na+ reabsorption are increased.
A ADH affects the reabsorption of water in the distal convoluted tubule and the collecting duct.
B Increased ADH increases the reabsorption of water.
C Decreased ADH decreases the reabsorption of water.
D ADH levels are controlled by the hypothalamus.
E ADH is released by the posterior pituitary via stimulation from the hypothalamus.
a. The body views increased atrial pressure as an increased extracellular fluid volume; therefore, ADH levels are decreased.
b. The body views decreased atrial pressure as a decreased extracellular fluid volume; therefore, ADH levels are increased. (Positive pressure ventilation and positive end-expiratory pressure [PEEP] normally decrease atrial pressure.)
2. Osmolarity of the extracellular fluid
a. The body views decreased osmolarity as an increase in extracellular fluid volume; therefore, ADH levels are decreased.
b. The body views increased osmolarity as a decrease in extracellular fluid volume; therefore, ADH levels are increased.
3. Urine specific gravity provides an index of how concentrated the urine is.
a. Normally the specific gravity is approximately 1.020, but it may range between 1.002 and 1.045.
b. Decreased specific gravity is associated with decreased ADH production and increased vascular volume.
c. Increased specific gravity is associated with increased ADH production and decreased vascular volume.
A Aldosterone controls the reabsorption of Na+ and the secretion of K+.
B Increased aldosterone increases the reabsorption of Na+ and the secretion of K+.
C Decreased aldosterone decreases the reabsorption of Na+ and the secretion of K+.
D Aldosterone affects Na+ and K+ movement at the distal convoluted tubule and the collecting duct.
E Aldosterone is secreted by the adrenal cortex. Its levels are increased by:
A Renin is secreted by the kidney in response to a decrease in the delivery of sodium chloride to a group of cells located between the afferent and efferent arterioles, the macula densa cells.
B Primarily a decrease in perfusion of the kidney increases the release of renin.
C Renin converts angiotensinogen formed by the liver to angiotensin I.
D Angiotensin I is converted to angiotensin II by the pulmonary endothelium.
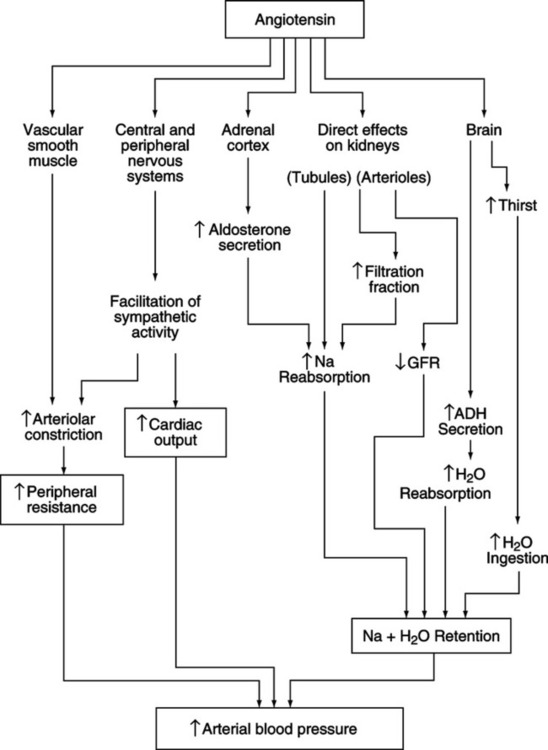
E Figure 13-5 summarizes the effects of angiotensin II.
F Angiotensin II is converted to angiotensin III. Most of the effects in Figure 13-5 can also be attributed to angiotensin III.
G Angiotensin levels facilitate Na+ and H2O retention and elevate arterial blood pressure. Angiotensin is the strongest vasopressor produced by the body.
H Angiotensin levels increase in response to physiologic stress.
XII Secretion of H+ and Reabsorption of HCO3−.
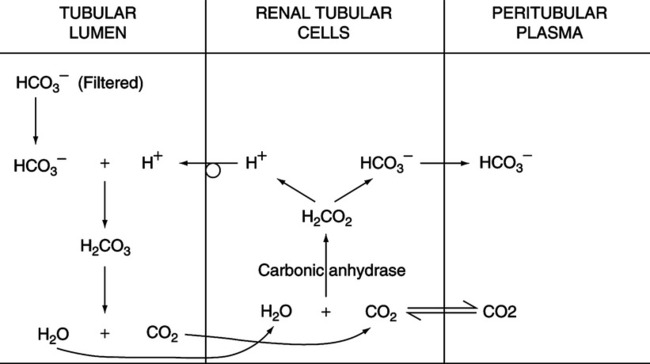
A Figure 13-6 illustrates the sequence of reactions maintaining normal H+ secretion and HCO3− reabsorption.
B Carbonic anhydrase is present in kidney tubule cells, increasing the hydration of CO2, which dissociates into H+ and HCO3−.
C As CO2 enters the kidney cell, H+ and HCO3− are formed. The HCO3− formed moves into the blood, and the H+ moves into the glomerular filtrate. As each H+ moves into the glomerular filtrate, a Na+ is reabsorbed into the bloodstream.
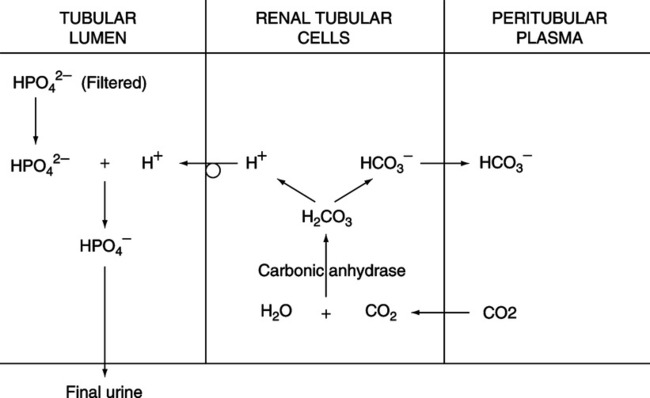
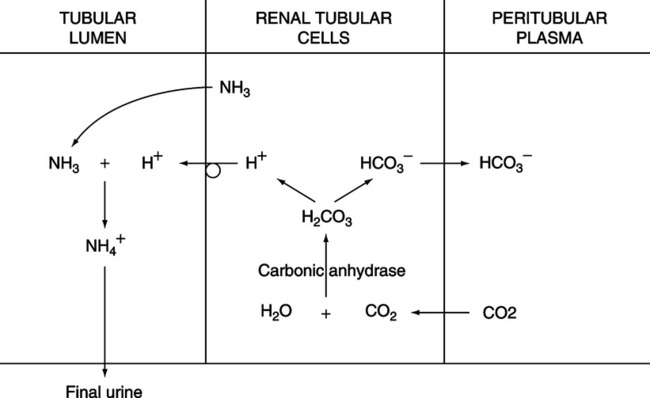
D In the glomerular filtrate, the H+ is buffered by:
E Note that for every HCO3− reabsorbed, one H+ is secreted.
F This series of reactions (see Figure 13-6) continues in the presence of normal acid-base balance.
G If a decrease in plasma Paco2 occurs, there is a decrease in the amount of HCO3− reabsorbed and H+ excreted.
H If Paco2 levels are increased, there is an increase in the amount of HCO3− reabsorbed and H+ excreted.
I When this occurs, the HCO3− in the tubular lumen is rapidly depleted; HPO4−2 and NH3 are used to buffer the excess H+ excreted (Figures 13-7 and 13-8).
J The kidney can continue to buffer acid until the pH of the urine decreases to approximately 4.0.
K Normal pH of the urine is approximately 7.33 to 7.37.
L The quantity of HCO3− reabsorbed over normal is equal to the amount of acid excreted in the form of H2PO4−1 and NH4+.
M Renal compensation for respiratory acid-base imbalances:
1. If Pco2 level increases, more HCO3− is formed and moved into the blood. This normalizes the acidic pH caused by the increased Pco2 level.
2. If Pco2 level decreases, less HCO3− is formed and moved into the blood. This normalizes the alkalotic pH caused by the decreased Pco2 level.
3. Compensation by the kidney is relatively complete, but the mechanism may take a long time to normalize the pH (24 to 48 hours or longer).