Removal of Uterine Septum
The uterus develops during intrauterine life as a result of fusion of the right and left müllerian ducts. When the fusion process fails to happen or occurs incompletely, a uterine septum results. The septum divides the usually capacious corporeal cavity into two smaller spaces. A complete septum extends to the level of the cervicocorporeal junction. An incomplete septum extends variable distances downward from the fundus toward the cervix. Total nonfusion results in a didelphic uterus, that is, completely separate bodies and cervices.
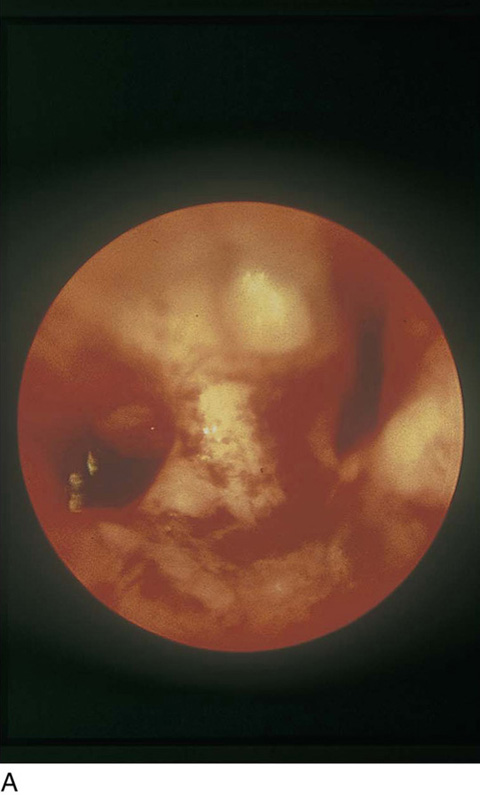
The diagnosis of a septate uterus is suspected unexplained preterm labor occurs. The condition does not lead to infertility. The diagnosis can be objectively made by a variety of techniques, including hysteroscopy. The hysteroscopic examination is conclusive. The cavity is divided by a vertical pillar of tissue extending from anterior to posterior walls (Fig. 108–1). The finding is analogous to viewing the end of a double-barreled shotgun head-on.
A diagnostic laparoscopic examination must always precede hysteroscopic takedown of the septum. The intra-abdominal aspect of the uterus is viewed to exclude the diagnosis of a bicornuate uterus. Finding the latter contraindicates hysteroscopic septum resection. The surgical procedure required to correct a bicornuate uterus is described in Unit II (Chapter 16). Similarly, laparoscopy is simultaneously performed during the septal surgery.
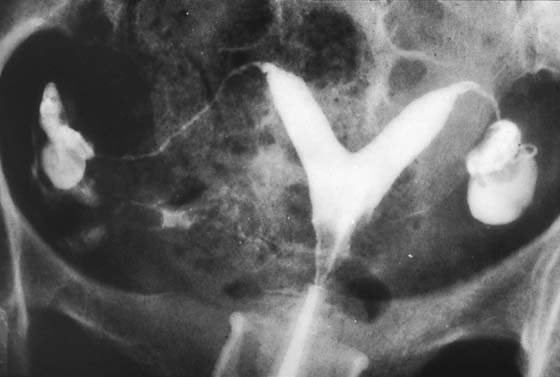
Hysterosalpingography will memorialize the septum’s structural presence and will document tubal patency (Fig. 108–2). Postoperative imaging will similarly document the adequacy of the surgery.
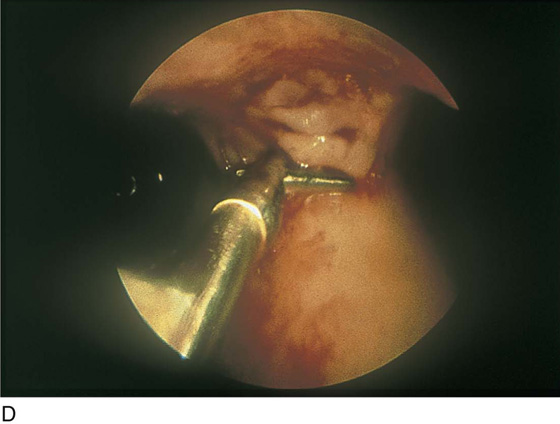
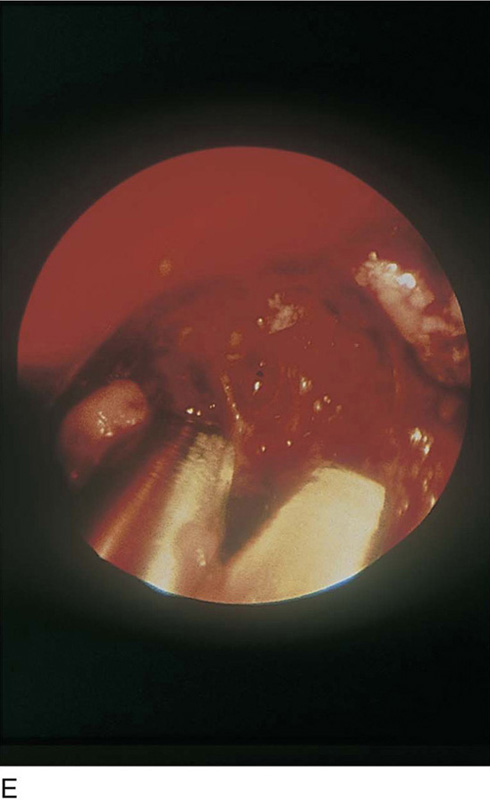
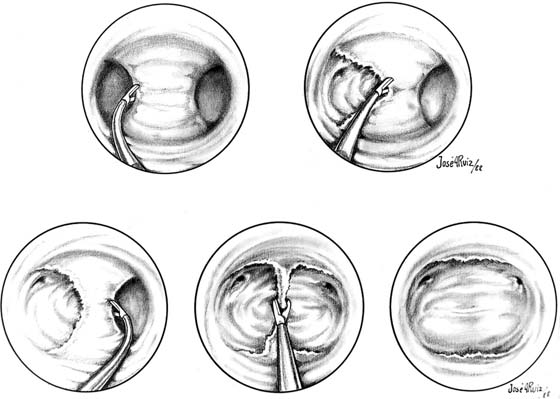
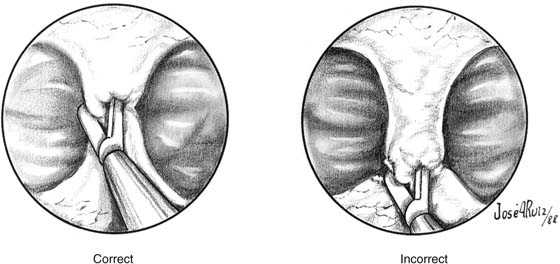
When the investigation has been completed, the septum is cut. The preferred tool to accomplish this is hysteroscopic scissors (Fig. 108–3). Thermal devices, such as resectoscope electrode, needle electrode, or laser, may be utilized; however, these devices all produce tissue necrosis and result in a greater potential for scar formation. The greatest risk for use of scissors is bleeding. This can be avoided by maintaining the incision through the septum at midpoint and avoiding cutting into the myometrium at the level of the fundus (Fig. 108–4). As the septum is incised, the hysteroscopist should regularly reorient to ensure that he or she is not drifting anteriorly or posteriorly (Fig. 108–5). Pulsatile bleeding indicates intrusion into the myometrium and should signal the operator to cease cutting. The assistant observing through the laparoscope can and should signal the operator as the intensity of the light on the hysteroscope increases (Fig. 108–6). The cold fiberoptic light of the hysteroscope transluminates through the uterine wall.
Upon completion of the procedure, the inflow and outflow ports of the operative sheath should be closed to decrease intrauterine pressure. This maneuver permits the surgeon to assess for any gross bleeding.

FIGURE 108–1 A. View of a subseptate uterus from a point just above the internal os of the cervix. B. View of a bicornuate uterus from the upper portion of the cervix. Note: Without a laparoscopic exam, the bicornuate and subseptate uterus would be difficult to segregate.
FIGURE 108–2 Hysterosalpingogram showing a fusion defect and a rather broad septum.
FIGURE 108–3 A. Subseptate uterus just before resection. B. The hysteroscopic scissors are seen at 12 o’clock approaching a midpoint of the septum between the anterior and posterior walls of the uterus. C. The scissors cut the septum, which rarely bleeds because it is largely avascular. D. Panoramic view showing the scissors cutting in the midplane, that is, at the correct location. E. The septum has been completely incised. As the top of the septum is reached, bleeding is encountered because of a better blood supply.
FIGURE 108–4 Technique for incising a broad septum. The peripheral edges are cut, causing the thick septum to be whittled down.
FIGURE 108–5 Schematic illustrating the correct location (left) versus the wrong location (right) at which to cut a septum. Drifting too low will invariably lead to bleeding.
FIGURE 108–6 An assistant observing via a laparoscope can alert the hysteroscopist that the septum incision should cease based on observing the relative brightness of the light on the hysteroscope, which transluminates through the uterine wall.