Chapter 23 Rehabilitation of Posterior Cruciate Ligament and Posterolateral Reconstructive Procedures
Clinical Concepts
The rehabilitation protocols described in this chapter consist of a careful incorporation of exercise concepts supported by scientific data and clinical experience.3,14,15,17 The goal is to progress a patient on a rate that takes into account athletic and occupational goals, condition of the articular surfaces and menisci, return of muscle function and lower limb control, postoperative graft healing, and graft remodeling. Modifications to the postoperative exercise program may be required if noteworthy articular cartilage deterioration is found during surgery.
The protocol for PCL reconstruction was developed for a high-strength two-strand graft (quadriceps tendon–bone, bone–patellar tendon–bone). The protocol for posterolateral reconstruction may be used after the various operative options described in detail in Chapter 22, including anatomic and proximal advancement techniques of the posterolateral structures and nonanatomic femoral-fibular reconstruction.
Critical Points CLINICAL CONCEPTS
Patients with posterolateral reconstruction are warned specifically at the 4th to 8th postoperative weeks that, with resumption of weight-bearing and weaning of crutches, to avoid a varus or internal tibial rotation position that could place high tensile forces on the posterolateral structures.13,16 It is important that the patient demonstrates good lower extremity control with suitable muscle strength to maintain tibiofemoral compensation and avoid a lift-off of the lateral tibiofemoral joint, which may disrupt the posterolateral reconstruction.
PCL Clinical Biomechanics
Kaufman and coworkers8 used a three-dimensional biomechanical model to predict dynamic patellofemoral and tibiofemoral forces generated during isokinetic exercises at 60°/sec and 180°/sec. During isokinetic extension, posterior shear forces were detected at knee flexion angles of 40° and greater. The maximum posterior shear force occurred at 70° to 80° of knee flexion and measured 0.5 ± 0.1 body weight at 60°/sec and 0.6 ± 0.1 body weight at 180°/sec
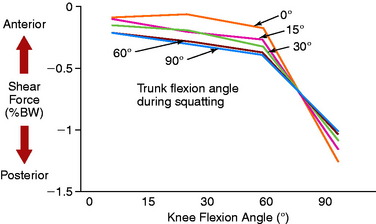
Ohkoshi and associates19 used a two-dimensional model to calculate shear force exerted on the tibia during standing at various knee flexion angles in 21 healthy subjects. Posterior shear forces were found in the upright position of the trunk and at knee flexion angles of 15° to 90° (Fig. 23-1). At 30° and 60°, the posterior drawer force was significantly increased by anterior flexion of the trunk.
Castle and colleagues4 measured posterior tibial subluxation during a static double-legged squat in patients with PCL-deficient knees. The results revealed a statistically significant mean increase of 5.9 mm in posterior tibial translation (P < .05) of the injured knee compared with the contralateral knee at high knee flexion angles. At low flexion angles, the magnitude of increase in mean posterior tibial translation was only 2.1 mm. Tibiofemoral shear forces were small compared with tibiofemoral joint compression forces.
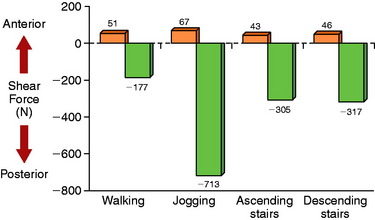
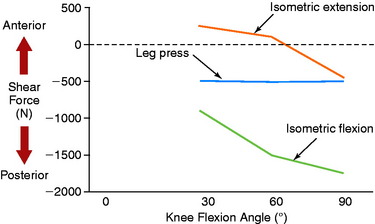
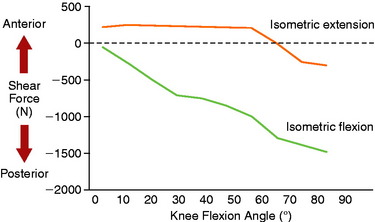
Berchuck and coworkers2 calculated large posterior shear forces during gait analysis for the activities of jogging, ascending stairs, and descending stairs (Fig. 23-2) in five normal subjects. Lutz and associates9 evaluated tibiofemoral joint shear and compressive shear forces using a two-dimensional biomechanical model and electromyographic (EMG) activity of hamstrings and quadriceps muscle activity during a closed kinetic chain (CKC) leg press exercise, an isometric open kinetic chain (OKC) exercise, and an OKC flexion exercise. Measurements of maximum muscle contractions were obtained at 30°, 60°, and 90° of knee flexion. The OKC isometric flexion exercise produced posterior shear forces at all knee flexion angles (Fig. 23-3), ranging from –939 ± 174 N at 30° of knee flexion to a maximum of –1780 ± 699 N at 90° of knee flexion. The CKC exercises produced significantly less posterior shear forces at 60° and 90° of flexion (–538 N; P < .05). These findings were similar to those reported by Smidt21 during isometric knee extension and flexion exercises (Fig. 23-4). Maximum hamstrings EMG activity was detected during the OKC exercise at 90° of flexion (82 ± 15% of maximum contraction). The antagonistic muscle activity was minimal during this exercise at all knee flexion angles. In contrast, co-contraction of the quadriceps and hamstrings was observed during the CKC exercise, which was greatest at 30° and 60° of flexion. The authors concluded that CKC exercise produced significantly less tibiofemoral shear forces compared with OKC exercise (P < .05).
Critical Points POSTERIOR CRUCIATE LIGAMENT CLINICAL BIOMECHANICS
CKC, closed kinetic chain; OKC, open kinetic chain; PCL, posterior cruciate ligament.
Wilk and colleagues23 evaluated tibiofemoral shear forces and EMG activity of the quadriceps, hamstrings, and gastrocnemius muscles during OKC extension and CKC leg press and squat exercises. Both CKC exercises produced posterior shear forces. However, during the squat, these forces were relatively low (245–565 N) from 0° to 45° of knee flexion. A rapid increase in posterior shear forces was detected from 45° to 72° of flexion. In addition, co-contraction of the quadriceps and hamstrings occurred from 0° to 30° of flexion. The authors concluded that vertical squats from 0° to 45° of flexion should not be performed in knees in the early stages of PCL reconstruction rehabilitation.
Wilk and colleagues23 also found that the knee extension exercise produced posterior shear forces from 60° to 100° of knee flexion; however, these forces were lower than those measured during both CKC exercises. The leg press induced minimal hamstring muscle activity.
Hoher and coworkers7 reported that the in situ forces in the PCL significantly increased with knee flexion in response to an isolated hamstrings load, reaching a maximum at 90° of flexion. These findings were in agreement with other authors5,24 who also reported increased strain in the PCL with knee flexion. The addition of a 200-N quadriceps load (simulating co-contraction of the quadriceps and hamstrings) reduced the in situ forces in the PCL.
Toutoungi and associates22 combined noninvasive experimental measurements with geometrical modeling of the lower extremity to calculate ligament forces during isometric, isokinetic, and squat exercises. The data indicated that isokinetic extension at knee flexion angles less than 70° should be safe in the early postoperative period after PCL reconstruction. However, isokinetic flexion and deep squats should be avoided. During isokinetic flexion, only the PCL is loaded and peak forces may reach over 4 times the patient’s body weight at 90° of knee flexion. During squatting, PCL forces may reach 3.5 times body weight at high knee flexion angles. Shallow squats with knee flexion angles kept below 50° may be considered.
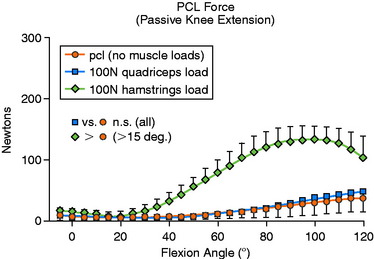
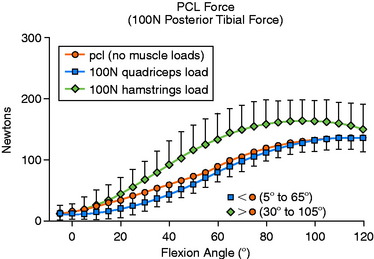
Markolf and colleagues10 studied the effects of muscle loads on cruciate force levels when the knee was subjected to external forces and moments. Load cells were installed into cadaveric knees to record forces in the ACL and PCL under five loading conditions. These force measurements were repeated with a 100-N load applied to the quadriceps tendon and with a combined 50-N load applied to both the biceps and the semimembranosus-semitendinosus tendons.
With no applied tibial force, application of hamstrings load significantly increased mean PCL force from 15° to 120° of knee flexion (Fig. 23-5; P < .05). With the application of a 100-N posterior tibial force, the addition of hamstrings load significantly increased mean PCL force between 30° and 105° of flexion (Fig. 23-6; P < .05). When a 5-Nm external tibial torque was applied, the addition of hamstrings load significantly increased mean PCL force beyond 75° of knee flexion (P < .05). Under a 5-Nm internal tibial torque, application of hamstrings load also significantly increased mean PCL force between 60° and 100° of flexion (P < .05). The authors concluded that, in general, the hamstrings were more effective in producing changes in cruciate force levels. Application of tibial torque in either an anterior or a posterior direction when the knee was flexed greater than 60° increased PCL force, and isolated hamstrings activity (with tibial torque) further increased PCL force.
Protocol for Partial or Acute Isolated PCL Ruptures
The rules to treat partial or acute isolated PCL tears are
PCL Reconstruction Postoperative Protocol
Immediate Postoperative Management
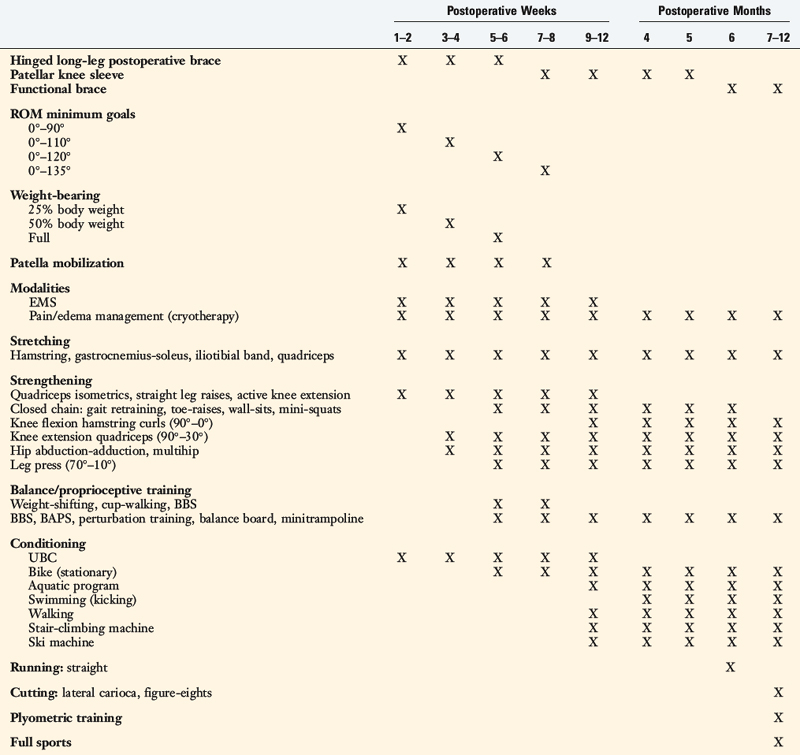
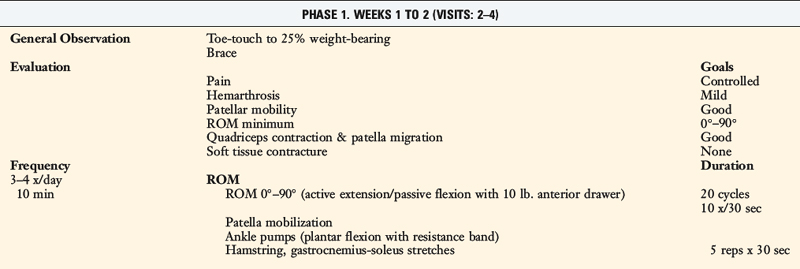
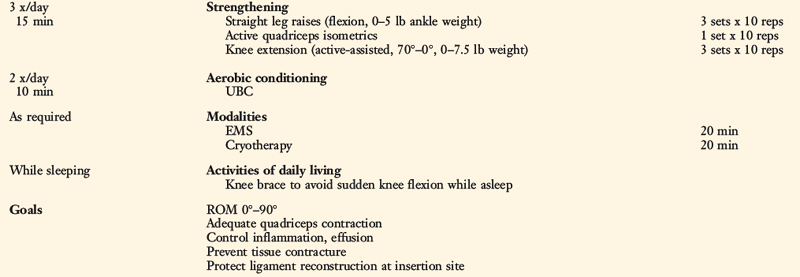
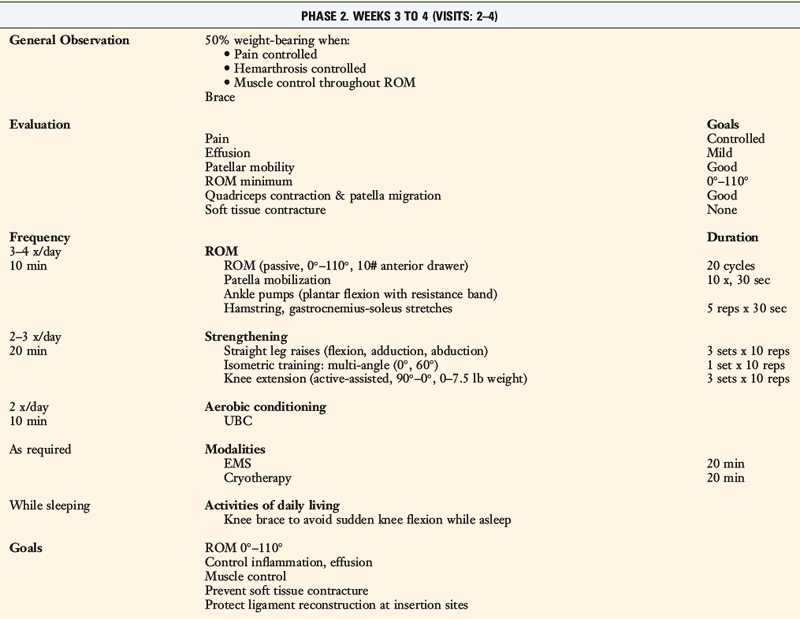
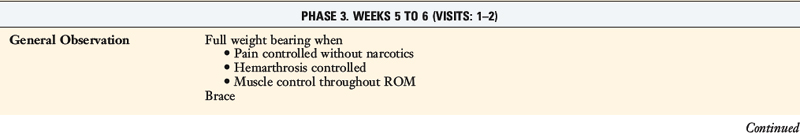
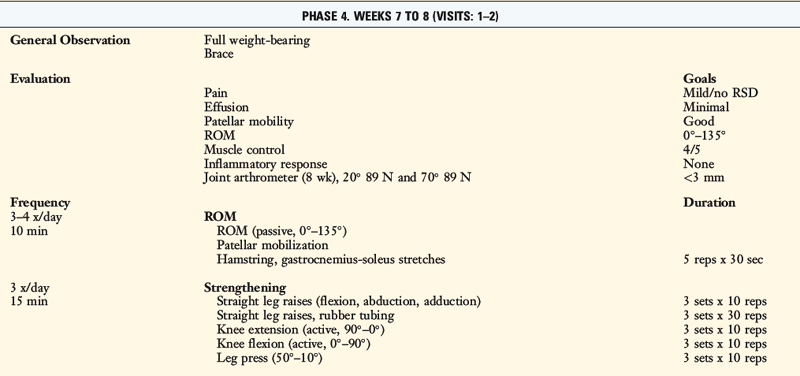
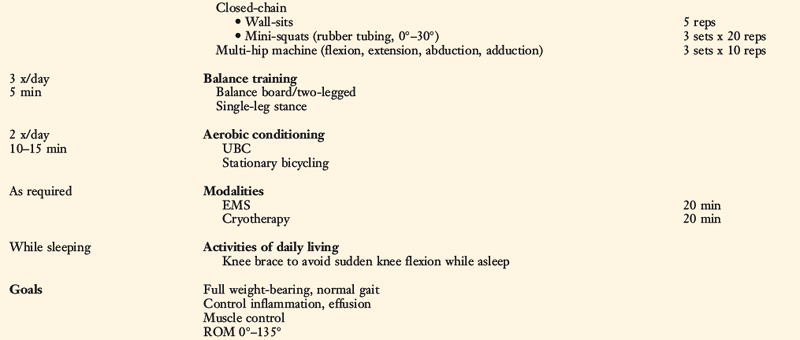
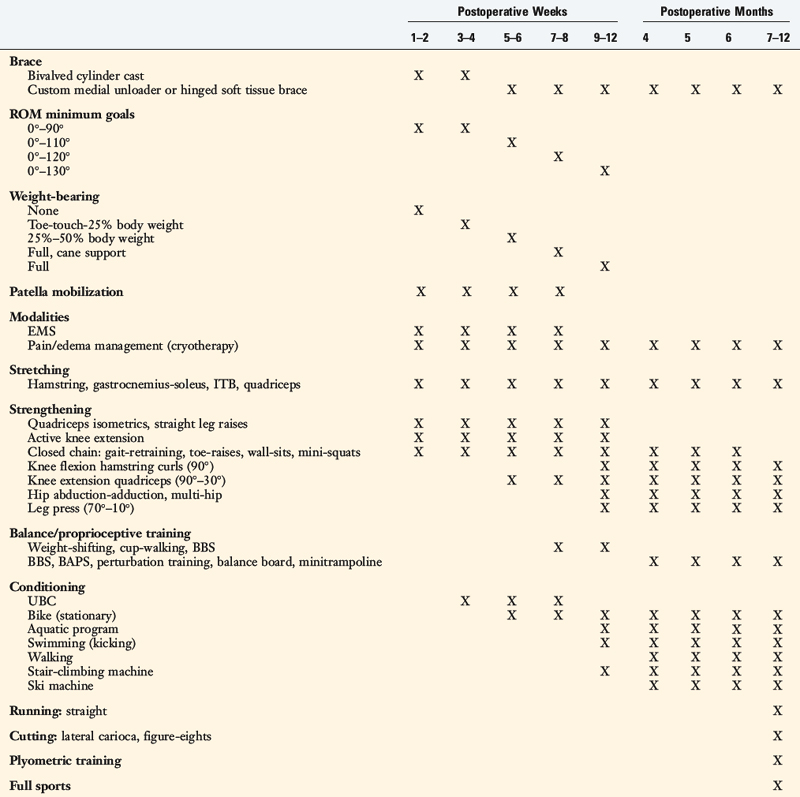
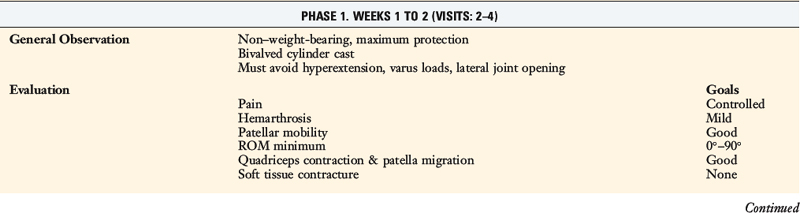
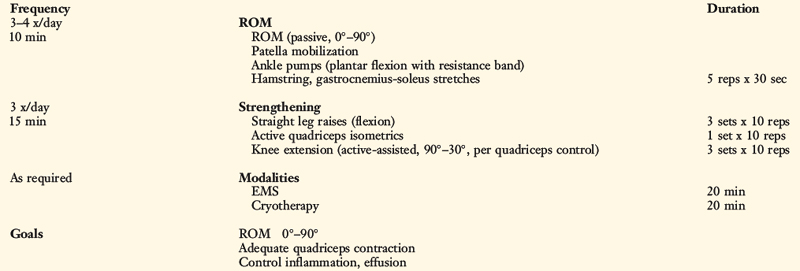
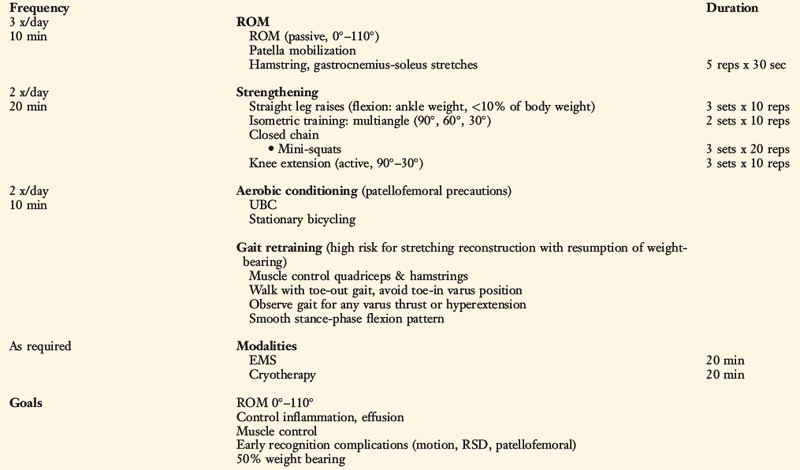
Patients present to physical therapy the 1st day after surgery on bilateral axillary crutches in a postoperative dressing with a long-leg brace locked in full extension (Table 23-1). The postoperative bandage and dressing are changed to allow the application of thigh-high compression stockings and a compression bandage. Early control of postoperative effusion is essential for pain management and early quadriceps reeducation. In addition to compression, cryotherapy is important in this time period.
Range of Knee Motion
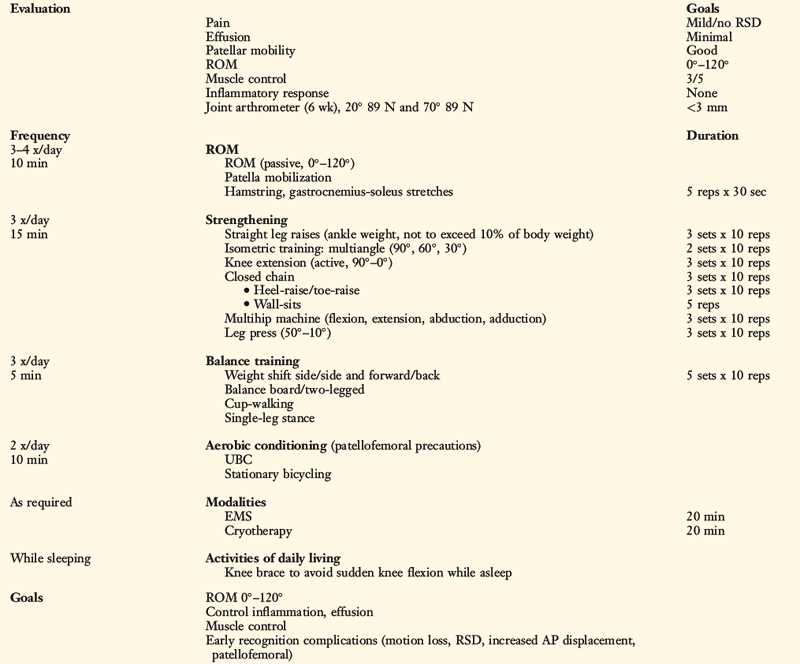
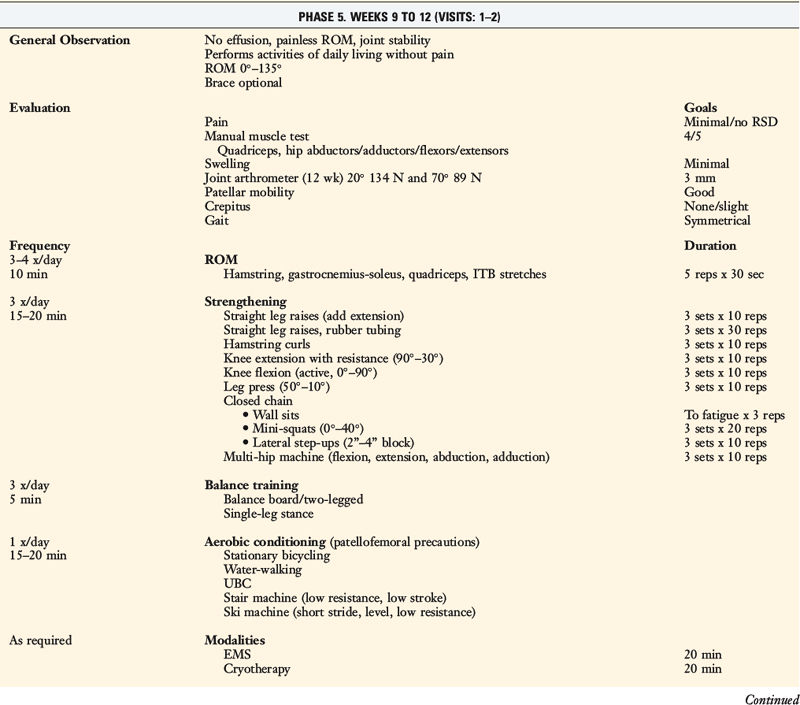
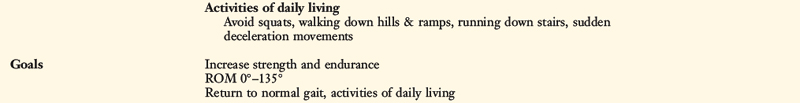
Passive knee motion from 0° to 120° is allowed immediately postoperatively. Although patients are encouraged to regain full extension as soon as possible, knee flexion is limited for the first 7 to 8 postoperative weeks to avoid high posterior shear forces. The total number of daily knee motion cycles is limited to 60 (20 cycles, three times/day) for the first 4 weeks to limit undue abrasion of the graft.12,20
Regaining knee extension as soon as possible is important to avoid excessive scarring in the intercondylar notch or a posterior capsular contracture. Patients who do not achieve this extension goal by the 7th postoperative day are placed into an overpressure program. The foot and ankle are propped on a towel or other device that elevates the hamstrings and gastrocnemius, allowing the knee to drop into full extension. This exercise is performed for 10 minutes and repeated approximately six times per day. A 10-pound weight may added to the distal thigh and knee to stretch the posterior capsule (Fig. 23-8). Care should be taken to keep the hanging weight away from the proximal tibia to avoid posterior shear stresses. Zero degrees of knee extension should be obtained by the 3rd to 6th postoperative weeks. If this is not accomplished, or if the clinician notes a firm end feel, a serial casting program may be required (see Chapter 41, Prevention and Treatment of Knee Arthrofibrosis). Hyperextension is avoided to protect the healing PCL graft.
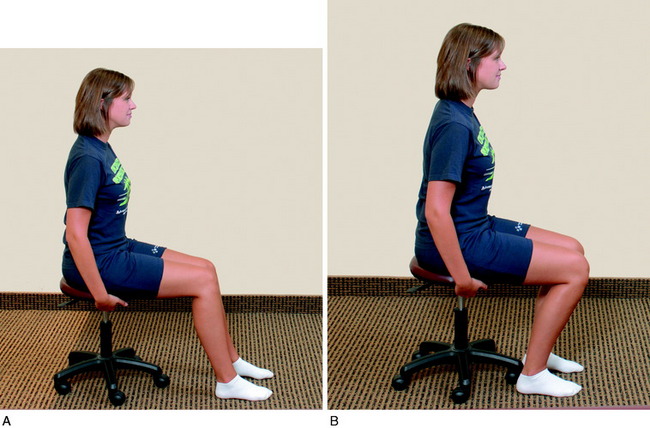
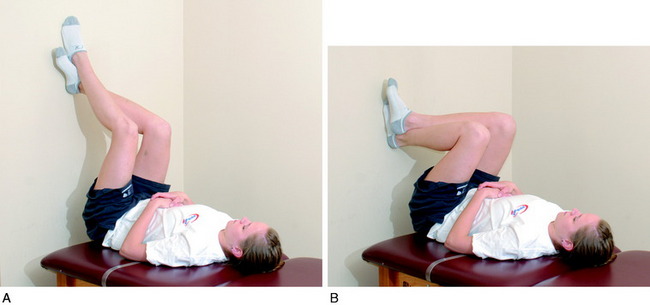
Passive knee flexion exercises are performed in the seated position, using an anterior manual force to provide proximal tibial support to prevent posterior drop-back. A 10-pound anterior drawer is maintained on the proximal tibia during passive knee flexion (Fig. 23-9) because PCL forces significantly increase after 70° of flexion. Knee flexion exercises are primarily passive for the first 6 weeks and are then active for the next 6 weeks. Care must be taken to avoid activating the hamstrings. Other overpressure techniques to assist in gaining flexion include chair-rolling (Fig. 23-10), wall-sliding using the opposite extremity (Fig. 23-11), commercial devices (Fig. 23-12), and passive quadriceps-stretching exercises.
Patellar Mobilization
Patellar mobilization is important in the promotion of a full range of knee motion. The loss of patellar mobility is often associated with knee motion complications and, in extreme cases, the development of patella infera.18 Patellar glides are performed in all four planes (superior, inferior, medial, and lateral) with sustained pressure applied to the appropriate patellar border for at least 10 seconds (Fig. 23-13). This exercise is performed for 5 minutes before ROM exercises are completed. Caution is warranted if an extensor lag is detected, because this may be associated with poor superior migration of the patella, indicating the need for additional emphasis on this exercise.Patellar mobilization is performed for approximately 8 weeks postoperatively.
Strengthening
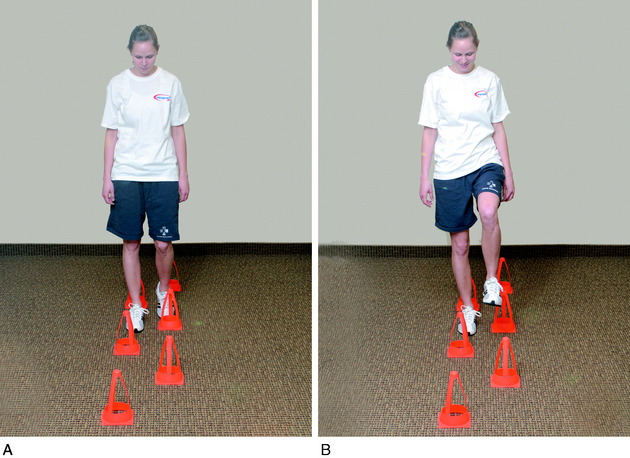
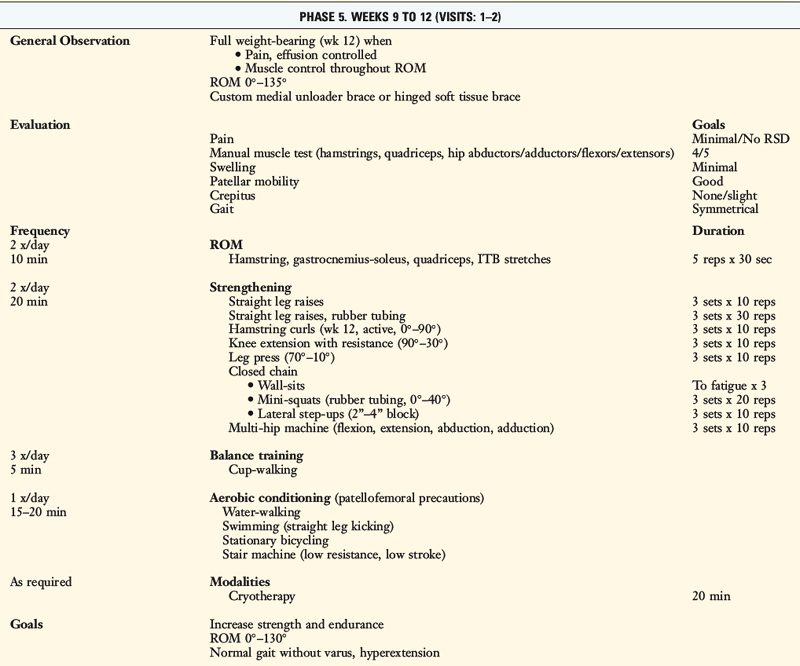
Once partial weight-bearing is initiated, CKC exercises are begun. The first CKC exercise is cup-walking, an activity designed to facilitate adequate quadriceps control during midstance of gait to prevent knee hyperextension from occurring (Fig. 23-14). When the patient progresses to 50% to 75% weight-bearing, toe-raises for gastrocnemius-soleus strengthening, wall-sitting isometrics for quadriceps control, and mini-squats for quadriceps strengthening are begun. The goal of wall-sitting is to improve quadriceps contraction by performing the exercise to muscle exhaustion. This exercise may be modified to decrease patellar pain or place additional stress on the quadriceps muscle. Patellar pain may be decreased by either altering the knee flexion angle of the sit or subtly changing the toe-out/toe-in angle by no more than 10°.
The last CKC exercise is the mini-squat. Initially, the patient’s body weight is used as resistance. Gradually, TheraBand or surgical tubing is employed as a resistance mechanism (Fig. 23-15). The depth of the squat is controlled to protect the patellofemoral joint. Quick, smooth, rhythmic squats are performed to a high-set/high-repetition cadence to promote muscle fatigue. Hip position is important to monitor in order to emphasize the quadriceps. Increased trunk flexion facilitates increased hamstring contractions19 and, therefore, must be carefully monitored to avoid forceful hamstring contractions for a minimum of 3 to 6 months.
The timing of the initiation of extension, hip, leg press, and hamstring curl OKC exercises is shown in Table 23-1. Knee flexion hamstring curls are delayed until the 12th postoperative week to avoid excessive posterior shear forces incurred with this activity. Leg press (range, 50°–0°) and hip abduction-adduction exercises are allowed at the 4th postoperative week. Caution is warranted owing to the potential problems knee extension OKC exercises may create for the healing graft and the patellofemoral joint. Many patients have an unsatisfactory outcome based on persistent anterior or patellofemoral knee pain, which can occur owing to improper training in the terminal phase of extension (0°–30°). Therefore, recommendations for knee extension exercises include emphasis on patellofemoral protection (monitoring for changes in pain, swelling, and crepitus) and a gradual progression of weight to avoid overuse syndromes.
Balance, Proprioceptive, and Perturbation Training
Another helpful activity for balance control is the single-leg balance exercise. The stance position is key to making this exercise beneficial. The patient is instructed to point the foot straight ahead, flex the knee approximately 20° to 30°, extend the arms outward to horizontal, and position the torso upright with the shoulders above the hips and the hips above the ankles. The object of this activity is to stand in position until balance is disturbed. A minitrampoline or unstable surface can be used to make this exercise more challenging. The unstable position created with the soft surface requires greater dynamic limb control than that used to stand on a flat surface (Fig. 23-16).
Critical Points BALANCE/PROPRIOCEPTIVE/PLYOMETRIC TRAINING
Plyometric Training
Perturbation-training techniques are initiated at approximately the 7th to 8th postoperative weeks. The therapist stands behind the patient and disrupts her or his body posture and position periodically to enhance dynamic knee stability. The techniques involve either direct contact with the patient (Fig. 23-17) or disruption of the platform the patient is standing on (Fig. 23-18).
Running and Agility Program
Plyometric Training
During the jumps, the patient is instructed to keep the body weight on the balls of the feet and to jump and land with the knees flexed and a shoulder-width apart to avoid knee hyperextension and an overall valgus lower limb position (Fig. 23-19), as described in detail in Chapter 19, Decreasing the Risk of Anterior Cruciate Ligament Injuries in Female Athletes. The patient should understand that the exercises are reaction and agility drills and, although speed is emphasized, correct body posture must be maintained throughout the drills.
Return to Sports Activities
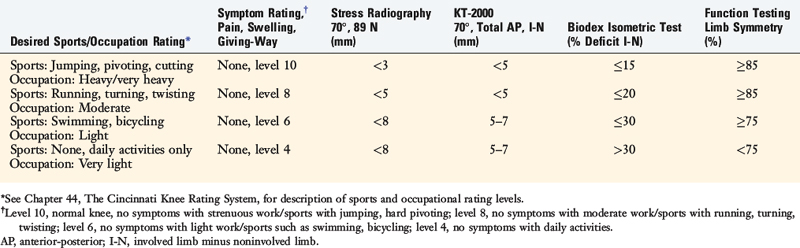
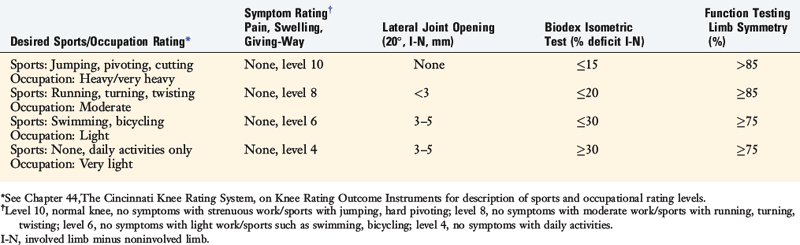
Discharge criteria after PCL reconstruction is based on patient goals for athletics and occupations and the rating of symptoms, stress radiography (90° flexion), KT-2000 testing, muscle strength testing, and function testing (Table 23-2). First, patients complete the Cincinnati Sports Activity Scale and Occupational Rating Scale1 to provide sports and occupational levels that are desired after surgery. Upon completion of the protocol, pain, swelling, and giving-way are rated on the Cincinnati Symptom Rating Scale.1 The patient must not experience these symptoms at the level of activity that he or she wishes to participate in prior to discharge.
Stress radiography is performed as described previously,6 and the difference between knees must be within 5 mm prior to recommendation of return to strenuous activities.
Muscle strength testing is performed with a Biodex isokinetic dynamometer (Biodex Corporation, Shirley, NY) to ensure that adequate strength exists prior to the initiation of the plyometric, running, and cutting programs. At least two function tests are completed and limb symmetry calculated as previously described11 prior to the final discharge.
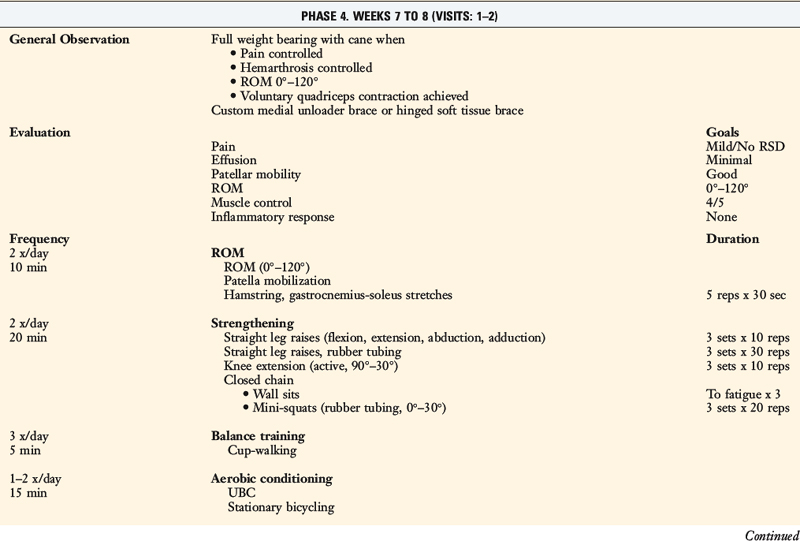
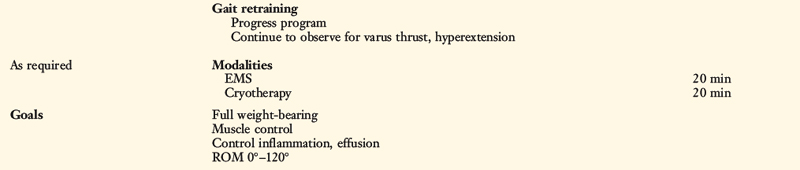
Posterolateral Reconstruction Rehabilitation
Patients who have chronic ruptures to the posterolateral structures may develop over time an alteration in gait in which excessive knee hyperextension occurs during the stance phase, described in detail in Chapter 34, Correction of Hyperextension Gait Abnormalities: Preoperative and Postoperative Techniques. A preoperative gait-retraining program is implemented for these patients, as failure to correct this problem leads to an increased risk of failure of any posterolateral reconstructive procedure.
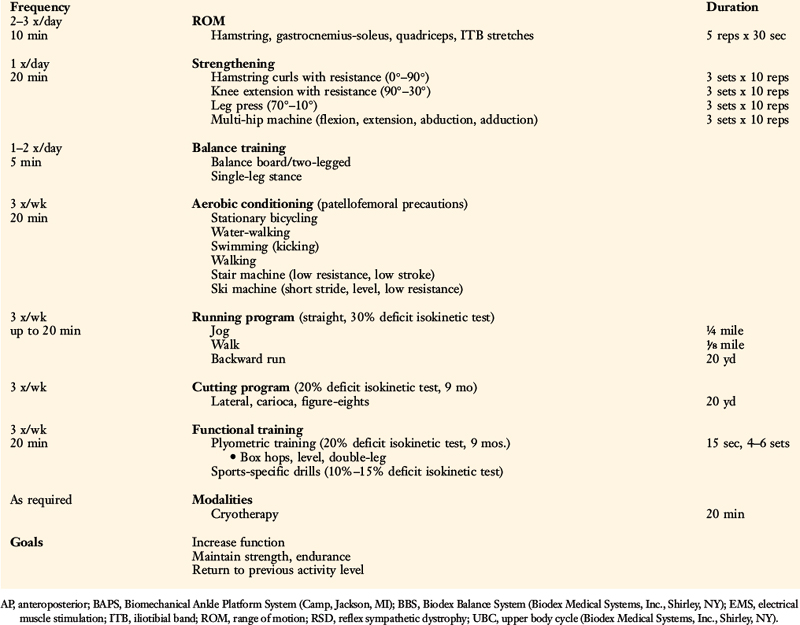
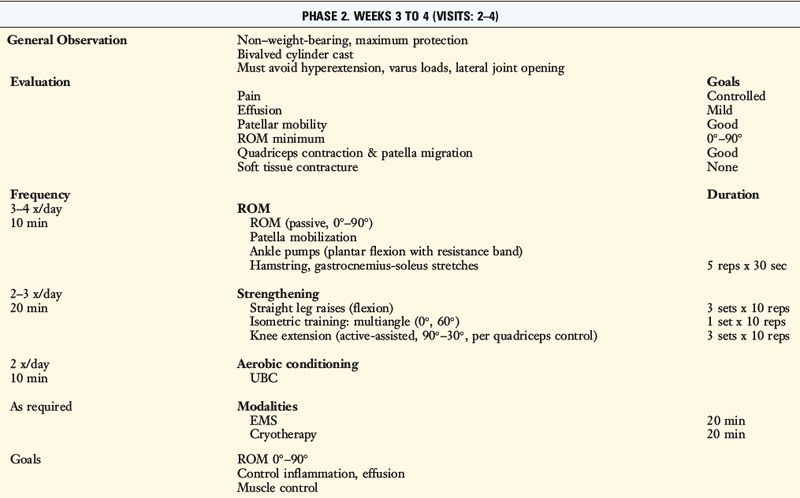
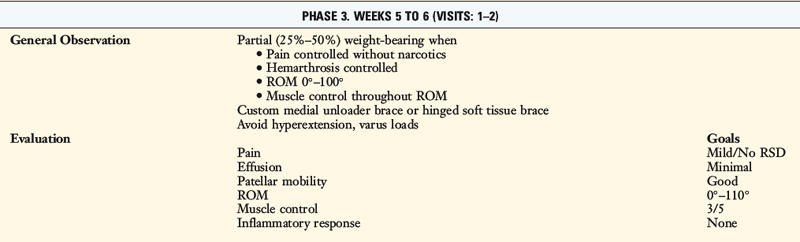
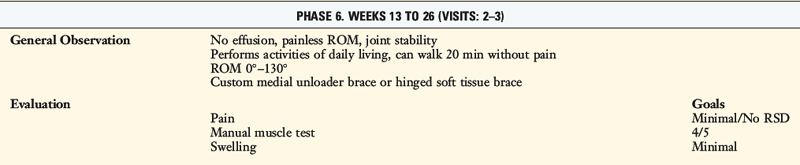
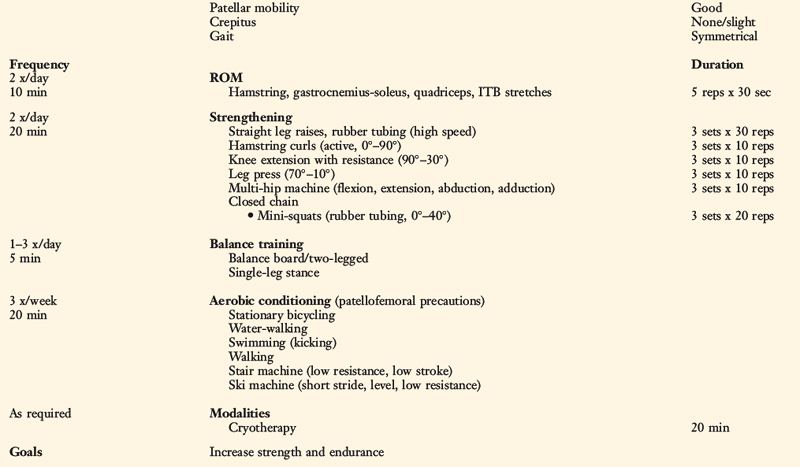
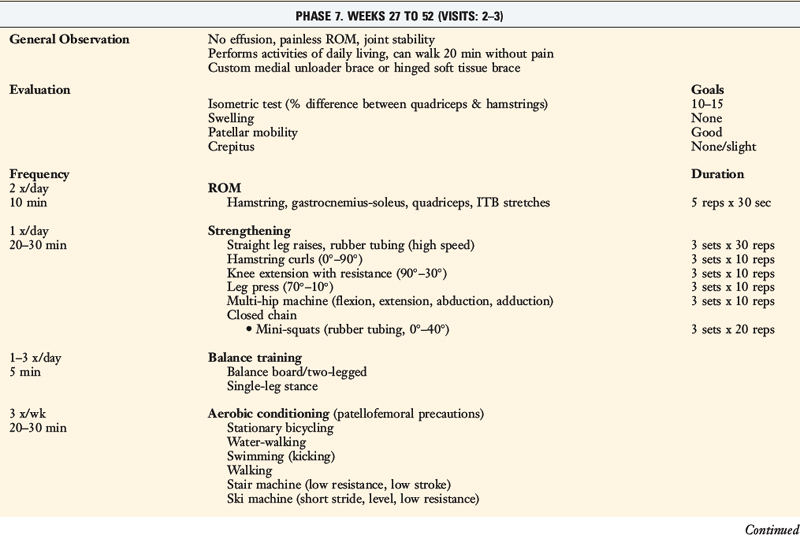
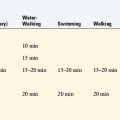
A variety of surgical options are available for ruptures of the posterolateral structures, which are detailed in Chapter 22, Posterolateral Ligament Injuries: Diagnosis, Operative Techniques, and Clinical Outcomes. The rehabilitation protocol incorporates immediate protected knee motion but stresses maximal protection against undue joint loads to prevent stretching and failure of posterolateral grafts or advancement procedures (Table 23-3). Patients are warned to avoid hyperextension and activities that would incur varus loading on the joint. Delays in return of full knee flexion, full weight-bearing, initiation of certain strengthening and conditioning exercises, and running and return to full sports activities are incorporated.
Discharge criteria after lateral and posterolateral graft reconstructions is based on patient goals for athletics and occupations and the rating of symptoms, lateral joint opening, muscle strength testing, and function testing (Table 23-4). Lateral joint opening is assessed by either stress radiography or manual testing at 20° of flexion. The remainder of the assessment is performed as previously described for PCL reconstructions.
1 Barber-Westin S.D., Noyes F.R., McCloskey J.W. Rigorous statistical reliability, validity, and responsiveness testing of the Cincinnati Knee Rating System in 350 subjects with uninjured, injured, or anterior cruciate ligament–reconstructed knees. Am J Sports Med. 1999;27:402-416.
2 Berchuck M., Andriacchi T.P., Bach B.R., Reider B. Gait adaptations by patients who have a deficient anterior cruciate ligament. J Bone Joint Surg Am. 1990;72:871-877.
3 Butler D.L., Noyes F.R., Grood E.S. Ligamentous restraints to anterior-posterior drawer in the human knee. A biomechanical study. J Bone Joint Surg Am. 1980;62:259-270.
4 Castle T.H.Jr., Noyes F.R., Grood E.S. Posterior tibial subluxation of the posterior cruciate–deficient knee. Clin Orthop. 1992;284:193-202.
5 Durselen L., Claes L., Kiefer H. The influence of muscle forces and external loads on cruciate ligament strain. Am J Sports Med. 1995;23:129-136.
6 Hewett T.E., Noyes F.R., Lee M.D. Diagnosis of complete and partial posterior cruciate ligament ruptures. Stress radiography compared with KT-1000 arthrometer and posterior drawer testing. Am J Sports Med. 1997;25:648-655.
7 Hoher J., Vogrin T.M., Woo S.L., et al. In situ forces in the human posterior cruciate ligament in response to muscle loads: a cadaveric study. J Orthop Res. 1999;17:763-768.
8 Kaufman K.R., An K.N., Litchy W.J., et al. Dynamic joint forces during knee isokinetic exercise. Am J Sports Med. 1991;19:305-316.
9 Lutz G.E., Palmitier R.A., An K.N., Chao E.Y. Comparison of tibiofemoral joint forces during open-kinetic-chain and closed-kinetic-chain exercises. J Bone Joint Surg Am. 1993;75:732-739.
10 Markolf K.L., O’Neill G., Jackson S.R., McAllister D.R. Effects of applied quadriceps and hamstrings muscle loads on forces in the anterior and posterior cruciate ligaments. Am J Sports Med. 2004;32:1144-1149.
11 Noyes F.R., Barber S.D., Mangine R.E. Abnormal lower limb symmetry determined by function hop tests after anterior cruciate ligament rupture. Am J Sports Med. 1991;19:513-518.
12 Noyes F.R., Barber-Westin S. Posterior cruciate ligament replacement with a two-strand quadriceps tendon–patellar bone autograft and a tibial inlay technique. J Bone Joint Surg Am. 2005;87:1241-1252.
13 Noyes F.R., Dunworth L.A., Andriacchi T.P., et al. Knee hyperextension gait abnormalities in unstable knees. Recognition and preoperative gait retraining. Am J Sports Med. 1996;24:35-45.
14 Noyes F.R., Grood E.S. Diagnosis of knee ligament injuries: five concepts. In: Feagin J., editor. The Crucial Ligaments. New York: Churchill Livingstone, 1988.
15 Noyes F.R., Heckmann T.P., Barber-Westin S.D. Posterior cruciate ligament and posterolateral reconstruction. In: Ellenbecker T.S., editor. Knee Ligament Rehabilitation. Philadelphia: Churchill Livingstone; 2000:167-185.
16 Noyes F.R., Schipplein O.D., Andriacchi T.P., et al. The anterior cruciate ligament–deficient knee with varus alignment. An analysis of gait adaptations and dynamic joint loadings. Am J Sports Med. 1992;20:707-716.
17 Noyes F.R., Stowers S.F., Grood E.S., et al. Posterior subluxations of the medial and lateral tibiofemoral compartments. An in vitro ligament sectioning study in cadaveric knees. Am J Sports Med. 1993;21:407-414.
18 Noyes F.R., Wojtys E.M., Marshall M.T. The early diagnosis and treatment of developmental patella infera syndrome. Clin Orthop. 1991;265:241-252.
19 Ohkoshi Y., Yasuda K., Kaneda K., et al. Biomechanical analysis of rehabilitation in the standing position. Am J Sports Med. 1991;19:605-611.
20 Shearn J.T., Grood E.S., Noyes F.R., Levy M.S. One- and two-strand posterior cruciate ligament reconstructions: cyclic fatigue testing. J Orthop Res. 2005;23:958-963.
21 Smidt G.L. Biomechanical analysis of knee flexion and extension. J Biomech. 1973;6:79-92.
22 Toutoungi D.E., Lu T.W., Leardini A., et al. Cruciate ligament forces in the human knee during rehabilitation exercises. Clin Biomech (Bristol, Avon). 2000;15:176-187.
23 Wilk K.E., Escamilla R.F., Fleisig G.S., et al. A comparison of tibiofemoral joint forces and electromyographic activity during open and closed kinetic chain exercises. Am J Sports Med. 1996;24:518-527.
24 Zavatsky A.B., Beard D.J., O’Connor J.J. Cruciate ligament loading during isometric muscle contractions. A theoretical basis for rehabilitation. Am J Sports Med. 1994;22:418-423.