Chapter 33 Rehabilitation after Tibial and Femoral Osteotomy
CLINICAL CONCEPTS
The protocol described in this chapter was designed for opening wedge high tibial osteotomy (HTO) and distal femoral osteotomy (DFO) in which an autogenous iliac crest bone graft is used along with internal fixation with a locking plate and screw. The operative techniques, detailed in Chapter 31, Primary, Double, and Triple Varus Knee Syndromes: Diagnosis, Osteotomy Techniques, and Clinical Outcomes, prevent delayed union or nonunion and collapse at the osteotomy site and allow a rehabilitation program of immediate knee motion and early weight-bearing, preventing the complications of arthrofibrosis and patella infera.1–5 As discussed in Chapter 31, allograft instead of an iliac crest autograft is frequently used for open wedge osteotomy. In these knees, a more cautious approach is required for resuming weight-bearing because healing is delayed approximately twofold. Full weight-bearing is not allowed until the surgeon advises based on radiographic evidence of healing. In addition, the physical therapist is informed whether a locking plate and screw fixation was used because this provides more rigid fixation. If a smaller non–locking plate and screw was used, protection from weight-bearing is required until osteotomy healing is advanced. In rare cases in which the opening wedge has been compromised at the lateral tibial cortex, inducing a fracture, no weight-bearing is allowed until complete healing of the osteotomy is verified.
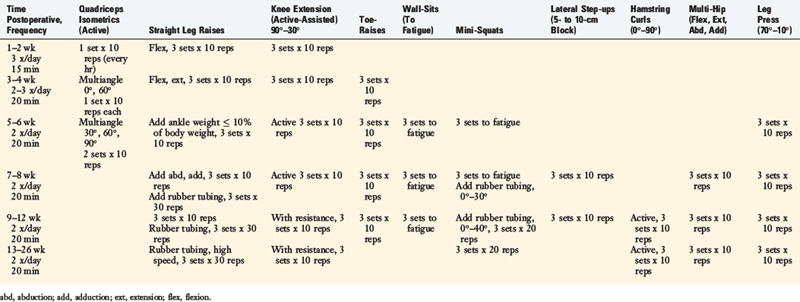
Important postoperative signs to monitor include (Table 33-1):
TABLE 33-1 Postoperative Signs and Symptoms Requiring Prompt Treatment
| Postoperative Sign, Symptom | Treatment Recommendations |
|---|---|
| Failure to meet knee extension and flexion goals (see text) | Overpressure program, early gentle manipulation under anesthesia if 0°–135° not met by 6 wk postoperatively. |
| Decreased patellar mobility (indicative of early arthrofibrosis) | Aggressive knee flexion, extension overpressure program, or gentle manipulation under anesthesia to regain full knee ROM and normal patellar mobility. |
| Decrease in voluntary quadriceps contraction and muscle tone, advancing muscle atrophy | Aggressive quadriceps muscle–strengthening program, EMS. |
| Persistent joint effusion, joint inflammation | Aspiration, rule out infection, close physician observation. |
| Loss of angular correction | Immediate referral to physician for revision. |
| DVT: abnormal calf tenderness, a positive Homans sign, or increased edema | Immediate ultrasound evaluation. |
DVT, deep venous thrombosis; EMS, electrical muscle stimulation; ROM, range of motion.
POSTOPERATIVE REHABILITATION PROTOCOL
Modalities
The postoperative rehabilitation protocol after tibial and femoral osteotomy is summarized in Table 33-2. In the immediate postoperative period, knee pain and effusion must be controlled to avoid quadriceps muscle inhibition or shutdown. Electrogalvanic stimulation or high-voltage electrical muscle stimulation (EMS) may be used to augment ice, compression, and elevation to control swelling. The treatment duration is approximately 30 minutes and the intensity is set to patient tolerance.
Critical Points POSTOPERATIVE REHABILITATION PROTOCOL
Patellar Mobilization
Postoperative Bracing and Weight-Bearing
A long-leg postoperative brace is worn for the first 8 to 12 weeks postoperatively. Patients then discontinue use of the brace, but if they continue to experience pain, Visco heel pads are used to unload the affected compartment. A lateral wedge is used for patients who underwent HTO, whereas a medial wedge is used for those who had a DFO. If pain remains, an unloading brace, used initially in a neutral position and then adjusted based on patient response, is recommended (Fig. 33-1).
Initially, patients are allowed only toe-touch weight-bearing. They are encouraged during this time period to lightly touch the ground with the toes of the operated limb while standing, with the visual image of stepping on a sponge, as frequently as possible during the day. At 4 weeks postoperative, double-stance, full-length anteroposterior radiographs are taken to determine osteotomy healing. Patients are then allowed to bear 25% of their body weight if the radiographs demonstrate adequate healing and maintenance of the osteotomy position and fixation implant (Fig. 33-2). A normal gait pattern is advocated that encourages normal knee flexion throughout the gait cycle. This technique allows for normal patterning of heel-to-toe ambulation, quadriceps contraction during midstance, and hip and knee flexion during the gait cycle. Average healing of the fracture site occurs at approximately 8 to 10 weeks postoperatively. In patients in whom allograft bone is used to fill the osteotomy gap, an additional delay in full weight-bearing may be required for up to 12 weeks postoperatively to allow for bony consolidation.
Range of Knee Motion
The postoperative goals for knee flexion and extension are shown in Table 33-3. Patients are encouraged to regain 0° to 90° within the first 2 weeks. Patients perform passive and active range of motion exercises in a seated position for 10 minutes a session, approximately three to four times per day.
Patients that have difficulty regaining at least 0° by the 2nd week are placed into an overpressure program using a propped foot/ankle position (Fig. 33-3). This position is maintained for 10 minutes and repeated four to six times per day. A 10-pound weight may be added to the distal thigh and knee to provide overpressure to stretch the posterior capsule. If this method is not successful in achieving full extension, or if the clinician notes a firm end feel, an extension board or additional weight of 15 to 20 pounds may be used up to six times a day.
Knee flexion is gradually increased to 110° by the 3rd to 4th postoperative week, 130° by the 5th to 6th week, and 135° by the 7th to 8th week. Methods to assist in achieving flexion greater than 90° include chair-rolling, wall-slides, knee flexion devices, and passive quadriceps stretching exercises (Fig. 33-4).
Patellar Mobilization
The resumption of normal patellar mobility is critical to regain a normal range of knee motion. The loss of patellar mobility is often associated with arthrofibrosis and, in extreme cases, the development of patella infera. Patellar glides are performed in all four planes (superior, inferior, medial, and lateral) beginning the 1st postoperative day with sustained pressure applied to the appropriate patellar border for at least 10 seconds (Fig. 33-5). This exercise is done for 5 minutes before range of motion exercises. Caution is warranted if an extensor lag is detected because this may be associated with poor superior migration of the patella, indicating the need for additional emphasis on this exercise. Patellar mobilization is performed for approximately 8 weeks postoperatively.
Strengthening
The strengthening program is begun on the 1st postoperative day (Table 33-4). Isometric quadriceps contractions are done hourly using the repetition rules of 10-second holds, 10 repetitions, 10 times per day. The patient is taught to monitor the contractions by visual or manual means, comparing the quality with those achieved by the contralateral limb. The superior migration of the patella is observed and should be approximately 1 cm during contractions, with inferior migration also seen during the initial relaxation of the contraction. The knee is held in a slightly flexed position during isometric contractions. Biofeedback may be used to reinforce an adequate quadriceps contraction.
Another common exercise effective in helping with quadriceps reeducation is the straight leg plus raise (Fig. 33-6). The quadriceps is contracted, the leg is lifted approximately 6 inches off the table or chair, held in the lifted position for 15 seconds, and then lowered and relaxed for 45 seconds. This 1-minute cycle is maintained and progressed in ratios (1:3, 1:2, and eventually, 1:1), and then progressed from 5 to 10 repetitions, with additional ankle weight added to increase the difficulty of the exercise.
Toe-raises are begun during the 3rd to 4th week as tolerated. Closed kinetic chain exercises may be initiated during the 5th to 6th week. Mini-squats from 0° to 45° are begun when tolerated by the patient. Initially, the patient’s body weight is used as resistance, and gradually, TheraBand or surgical tubing is added for resistance (Fig. 33-7). Quick, smooth, rhythmic squats are performed to a high-set/high-repetition cadence to promote muscle fatigue. Wall-sitting exercises are also begun during this time period. The goal of wall-sitting is to improve quadriceps contraction by performing the exercise to muscle exhaustion. If anterior knee pain is experienced, either the knee flexion angle of the sit or the toe-out/toe-in angle is altered. The exercise may also be modified by the patient squeezing a ball between the distal thighs, holding dumbbell weights, or shifting the body weight over the involved side to stimulate a single-leg contraction. This exercise is promoted as an excellent one to perform at home four to six times a day to achieve quadriceps fatigue in a knee flexion angle that does not induce anterior knee pain. Leg press exercises in the range of 70° to 10° are begun during this time period as well.
Balance, Proprioceptive, and Perturbation Training
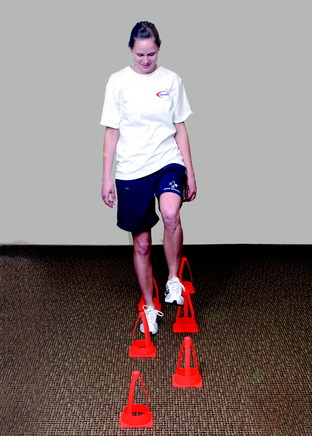
Cup-walking is an exercise that promotes symmetry between the surgical and the uninvolved limbs. This exercise helps develop hip and knee flexion and quadriceps control during midstance of gait to prevent knee hyperextension (see Chapter 34, Correction of Hyperextension Gait Abnormalities: Preoperative and Postoperative Techniques). In addition, cup-walking controls hip and pelvic motion during midstance, gastrocnemius-soleus activity during push-off, and excessive hip hiking (Fig. 33-8). This exercise may be initiated during the partial weight-bearing phase.
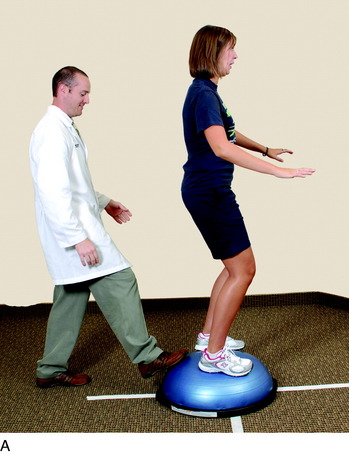
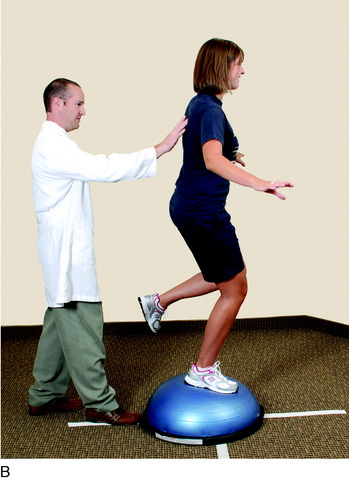
Perturbation-training techniques are also performed during balance exercises. The therapist stands behind the patient and disrupts her or his body posture and position periodically to enhance dynamic knee stability (Fig. 33-9). The techniques involve either direct contact with the patient or disruption of the platform the patient is standing on, and the patient is then instructed to correct the unbalanced position.
Half foam rolls are also used in this time period as part of the gait-retraining and balance program (Fig. 33-10A). This technique helps the patient develop balance and dynamic muscular control required to maintain an upright position and be able to walk from one end of the roll to the other. Use of a balance board or other unstable platform in double-leg and single-leg stance is another effective measure (see Fig. 33-10B). Developing a center of balance, limb symmetry, quadriceps control in midstance, and postural positioning are benefits obtained from this type of training.
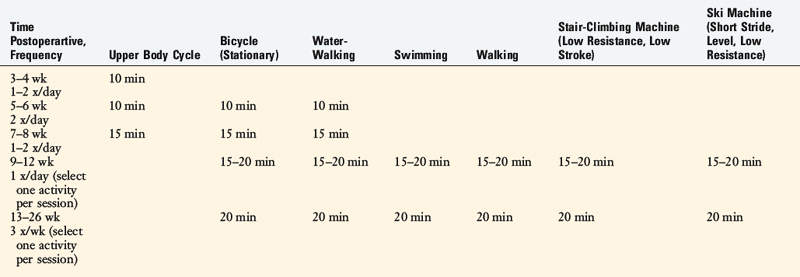
Conditioning and Return to Activities
Depending on accessibility, a cardiovascular program with an upper body cycle may be initiated as soon as tolerated by the patient (Table 33-5). The surgical limb should be elevated to minimize lower extremity swelling. Stationary bicycling is begun during the 5th to 6th postoperative weeks. Water-walking is also begun during this time period.
1 Noyes F.R., Mayfield W., Barber-Westin S.D., et al. Opening wedge high tibial osteotomy: an operative technique and rehabilitation program to decrease complications and promote early union and function. Am J Sports Med. 2006;34:1262-1273.
2 Noyes F.R., Wojtys E.M., Marshall M.T. The early diagnosis and treatment of developmental patella infera syndrome. Clin Orthop. 1991;265:241-252.
3 Noyes F.R., Barber S.D., Simon R. High tibial osteotomy and ligament reconstruction in varus angulated, anterior cruciate ligament-deficient knees. A two to seven year follow-up study. Am J Sports Med. 1993;21:2-12.
4 Noyes F.R., Barber-Westin S.D., Hewett T.E. High tibial osteotomy and ligament reconstruction for varus angulated anterior cruciate ligament deficient knees. Am J Sports Med. 2000;28:282-296.
5 Noyes F.R., Berrios-Torres S., Barber-Westin S.D., Heckmann T.P. Prevention of permanent arthrofibrosis after anterior cruciate ligament reconstruction alone or combined with associated procedures: A prospective study in 443 knees. Knee Surg Sports Traumat Arthrosc. 2000;8:196-206.