CHAPTER 43 Rehabilitation after Shoulder Arthroplasty
The goal of rehabilitation after shoulder arthroplasty is restoration of functional shoulder mobility in timely fashion. Biologic factors impose limitations in achieving mobility after shoulder arthroplasty. Histologically, collagenous connective tissues in the shoulder (tendons, ligaments, capsule) contract after shoulder arthroplasty. These connective tissues are subject to the biomechanical properties and limitations of collagen, including plasticity, stretching, and temperature sensitivity. The plasticity of collagen allows connective tissues to adapt to physiologic and pathologic conditions. Rehabilitation is designed to maximize these adaptations and provide functional recovery of mobility after shoulder arthroplasty. We use a hydrotherapy-based rehabilitation regimen after shoulder arthroplasty to regain shoulder mobility.1
REHABILITATION PROTOCOL
Rehabilitation starts with choosing the type of postoperative orthosis and its duration of use. This is based largely on the type of arthroplasty performed (unconstrained, fracture, reverse) and the performance of any associated procedures (posterior capsulorrhaphy). Table 43-1 summarizes the types of orthoses used and the duration of their use based on the procedure performed. All patients are instructed in hand, wrist, and elbow mobility exercises on postoperative day 1. Patients undergoing unconstrained shoulder arthroplasty for chronic conditions without performance of an associated posterior capsulorrhaphy are also instructed in pendulum exercises on postoperative day 1. These exercises are performed three to five times per day for approximately 15 minutes each time and are continued throughout the rehabilitative program. The time of initiation of hydrotherapy depends on the type of arthroplasty performed. Table 43-2 summarizes the time that hydrotherapy is instituted based on the procedure performed.
Table 43-1 TYPE OF POSTOPERATIVE ORTHOSIS USED AND DURATION OF USE
| Procedure | Type | Duration (wk) |
|---|---|---|
| Unconstrained arthroplasty | Simple sling | 2 to 4 |
| Unconstrained arthroplasty + posterior capsulorrhaphy | Neutral rotation sling | 4 |
| Fracture prosthesis | Neutral rotation sling | 4 to 6 |
| Reverse prosthesis | Neutral rotation sling | 3 to 4 |
Table 43-2 TIME FOR INITIATION OF HYDROTHERAPY
| Procedure | Hydrotherapy Initiated (Postoperative Week) |
|---|---|
| Unconstrained arthroplasty | 1 |
| Unconstrained arthroplasty + posterior capsulorrhaphy | 1 |
| Fracture prosthesis | 4 to 6 |
| Reverse prosthesis | 3 to 4 |
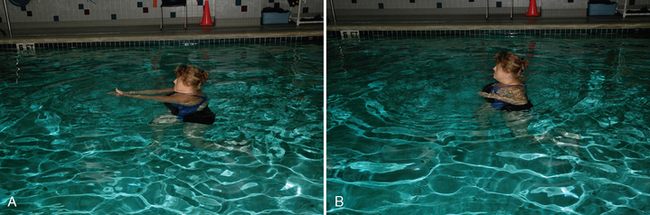
Hydrotherapy takes place daily (5 to 7 days per week, depending on availability) in a single 30- to 45-minute session. An abbreviated land-based verification session follows to affirm gains in mobility achieved in the pool. Various exercises designed to gain elevation, extension, horizontal adduction, internal rotation, and external rotation are performed in sets of 10 repetitions (Figs. 43-1 through 43-4). The unaffected extremity is used to help power the movement. Active mobility of the operated extremity is allowed in the form of a slow, gentle breaststroke motion with the palms placed horizontally (to not invoke resistance from the water), which is performed with the patient supported by a harness and the shoulders submerged (Fig. 43-5). In patients who have undergone unconstrained shoulder arthroplasty, external rotation beyond neutral is not allowed until 4 weeks postoperatively in patients with primary osteoarthritis or osteonecrosis and 6 weeks in patients with compromised soft tissues (inflammatory arthropathies, revision surgery) to protect the subscapularis repair. In patients who have undergone an associated posterior capsulorrhaphy, internal rotation and horizontal adduction are avoided until 4 weeks postoperatively. With the exception of these cases, no limitations on mobility are imposed.
Mobility exercises with total body immersion are advised for all patients; however, it is not forced on anyone. Patients who wish to try such exercises are fitted with a weighted belt and instructed to hold their breath as they kneel or recline supine on the bottom of the pool (Fig. 43-6). The same mobility exercises are then performed in the more insulated underwater environment. This technique is very helpful in accelerating gains in mobility.
As soon as the patient has achieved 140 degrees of elevation, the hands can be clasped behind the head in the “siesta” position (Fig. 43-7). Additional stretching exercises for the anterior capsule (Fig. 43-8) and posterior capsule (Fig. 43-9) can be performed in this position. From this position, motion is advanced until the “triple-locking” position is achieved, which stretches the inferior capsule (Fig. 43-10). Both the siesta and triple-locking positions are used extensively in a self-rehabilitation program implemented after the patient has been discharged from formal physical therapy.
An abbreviated session of land-based rehabilitation is used after the hydrotherapy session. The land-based session is performed principally to affirm the gains that the patient has made during the hydrotherapy sessions. The same exercises are used, but with fewer repetitions. Modality treatment (i.e., cryotherapy) is used on an as-needed basis. Analgesic pain medication is provided to patients for the first 6 postoperative weeks to alleviate the discomfort associated with surgery and subsequent rehabilitation.
RETURN TO ACTIVITY
We allow our patients to pursue most activities and sports after shoulder arthroplasty. We do limit patients to noncontact sports. The majority of our arthroplasty patients with athletic interests participate in golf and tennis. Restrictions placed on golfers and tennis players are designed to protect the subscapularis repair. Putting is allowed as soon as the patient can tolerate it postoperatively, usually within 6 weeks. At 3 months, half swings with a seven iron off a tee are allowed. This is advanced until the patient is allowed to hit a full swing with all clubs off a tee 4 to 5 months postoperatively. At 6 months after surgery, unrestricted golf is allowed. Tennis players are permitted to begin gentle ground strokes 3 months postoperatively. The intensity of the ground strokes is increased 4 to 5 months after surgery. Unrestricted tennis, including serves and overhead shots, is allowed 6 months postoperatively.