Chapter 45 Regional Anesthesia and the Difficult Airway
I Introduction
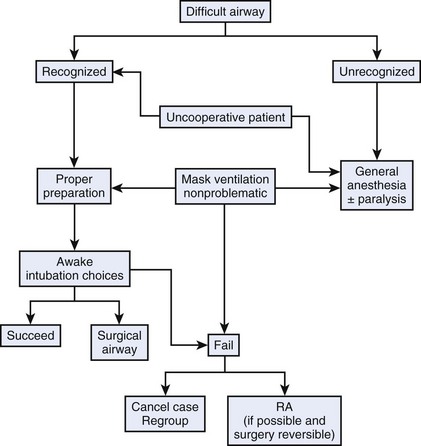
Regional anesthesia is recognized as an effective alternative to general anesthesia and is included in the American Society of Anesthesiologists (ASA) difficult airway algorithm as an alternative to failed intubation (Fig. 45-1).1 The anesthesiologist should carefully balance the risks and benefits of using regional anesthesia compared with those of securing the airway before the administration of anesthesia in a patient with an established difficult airway. The anesthesiologist has a responsibility to provide safe anesthetic care, including maintaining appropriate conditions to manage the airway effectively during the perioperative period. Morbidity and mortality as a consequence of mismanagement or lack of proper management of the airway represent major concerns for anesthesiologists worldwide.
II Practice Guidelines for Management of the Difficult Airway
Irrespective of the final decision, an appropriate assessment of the patient’s airway represents the first step. Although the ability to predict accurately a difficult airway preoperatively would be of great value, it is evident from the literature that no single airway assessment can reliably predict a difficult airway.2 Nevertheless, a preoperative airway history and physical examination should be performed in order to facilitate the choice and management of the difficult airway, as well as reduce the likelihood of adverse outcomes (see Chapter 9).3
Langeron and colleagues have established five factors that are frequently associated with difficult airway management.4 They separated difficult airway into difficult mask ventilation and difficult intubation; the former is the more deleterious of the two. It is well established that airway management may be more difficult in trauma cases and in patients with comorbidities, such as severe rheumatoid arthritis, morbid obesity, metabolic diseases, deformities, or pregnancy. Rocke and colleagues demonstrated that the incidence of difficult airway is 10 times higher during pregnancy than in the general population. They documented the potential risk factors for difficult airway in the obstetric patient.5 The risk factors included short neck, missing protruding incisors, receding mandible, facial edema, and high Mallampati scores. The relative risk of experiencing a difficult intubation compared with an uncomplicated class I airway assessment has been established as follows: class II, 3.23; class III, 7.58; class IV, 11.3; short neck, 5.01; receding mandible, 9.71; and protruding maxillary incisors, 8.0. Using the probability index or a combination of risk factors, or both, showed that for a combination of class III or IV plus protruding incisors, short neck, or receding mandible, the probability of difficult laryngoscopy was more than 90%.
The concept of a difficult airway has different meanings for different physicians. Although most anesthesiologists agree that a patient with very limited mouth opening, Mallampati IV classification, and a very short neck has a difficult airway, there is more controversy about the relative difficulty of managing the airway in a patient with cervical trauma or obesity. This in part reflects the increased expertise in airway management of anesthesiologists and the increased number of airway devices designed to facilitate airway management. For example, Hagberg and colleagues demonstrated that Cormack-Lehane grade 3 airways assessed by laryngoscopy were reduced to grade 2 and even grade 1 when using the video laryngoscope.6,7 The experience of the anesthesiologist with difficult airway management and access to certain airway management devices represent important factors in establishing the relative difficulty of managing the airway of a given patient.
Kheterpal and colleagues followed Langeron’s work by determining the incidence and predictors of difficult mask ventilation and impossible bag-mask ventilation in relation to a difficult intubation.8 Kheterpal later observed in more than 50,000 patients9 that 25% of impossible bag-mask ventilations (n = 19) also had difficult intubations and that 10% (n = 2) required surgical airways. The incidence of impossible bag-mask ventilations was 0.15%. Radiation-induced changes in the neck, male sex, obstructive sleep apnea, Mallampati class III or IV, and presence of a beard were identified as independent predictors. Despite the low incidence, the anesthesiologist must anticipate and recognize differences for difficult mask ventilation and difficult intubation while also exercising sound judgment in conducting regional anesthesia in this patient population.
III Use of Regional Anesthesia Versus Preoperative Management of the Airway
In the past few years, interest has increased in using regional anesthesia as the primary anesthesia technique, especially in patients undergoing gynecologic or obstetric; plastic; ear, nose, and throat; trauma; and orthopedic surgery. The literature supports using various techniques for performing regional anesthesia as the primary anesthetic on patients with difficult airways.10–12 We do not recommend performing these cases unless the anesthesiologist has a level of certainty about performing the block. Because of the more expanded use of regional anesthesia, anesthesiologists have become better accomplished at these techniques (e.g., higher success rate, lower frequency of complications). However, no regional technique provides a 100% success rate or is completely free of complications. Regional anesthesia complications include hematoma, nerve injury, and local anesthetic–associated complications, such as cardiac arrest, seizures, and death. When deciding whether to perform a regional technique in lieu of securing the airway preoperatively, these complications should be considered because they may trigger the need for immediate and urgent control of the airway because of a sudden loss of respiratory function (total spinal) or the development of local anesthesia–related complications (e.g., cardiac arrest, seizures).
Occurrence of these complications may be delayed, even if in most cases they occur within minutes after performance of a block. Anesthesiologists must be prepared to control the airway during the entire perioperative period. Although any regional technique intrinsically carries the risk of complications, the relative risk is different for each regional technique. For example, the use of an ulnar block at the wrist for an open reduction and internal fixation of the fifth finger performed using 5 to 6 mL of 0.5% ropivacaine is associated with a much lower risk of local anesthetic toxicity than the use of a transarterial axillary block performed with 40 mL of 0.5% bupivacaine. The specific type of approach, technique (e.g., transarterial, neurostimulator, paresthesia), volume of local anesthetic, and relative proximity of the injection site to a vessel or the central nervous system are some of the factors associated with the risks of toxicity associated with the use of regional anesthesia. Several considerations are important in making the decision to use regional anesthesia in a patient with an established difficult airway (Box 45-1). Knapik and colleagues demonstrated the ability to perform regional anesthesia for valvular heart surgery using a thoracic epidural on a patient with severe pulmonary disease, precluding the use of general endotracheal anesthesia.13 However, during cardiopulmonary bypass, the patient required ventilatory support with a mask technique, a feat that would have been ill advised if difficult mask ventilation was anticipated.
Box 45-1 Regional Anesthesia Versus Control of the Airway in Patients with Established Difficult Airways
B Anesthetic Environment
1 Anesthesiologist’s Expertise
The use of regional anesthesia as an alternative to the preoperative management of the airway in a patient with a known difficult airway can be considered only if the anesthesiologist has appropriate expertise with regional techniques and difficult airway management. Peripheral nerve blocks can be classified according to the degree of difficulty (Box 45-2).
Box 45-2 Peripheral Nerve Block Classification According to Difficulty
a Regional Anesthesia
The use of neurostimulator and ultrasound techniques is preferred to the use of paresthesia or transarterial techniques, or both, in the performance of regional anesthesia to increase the likelihood of success and minimize the required dose of local anesthetics, thereby minimizing the risk of seizures related to an intravascular injection. The smallest needle possible should be used to avoid intrathecal placement of the needle when performing an interscalene or a lumbar plexus block. Table 45-1 shows the needle sizes related to the practice of the most common peripheral nerve blocks.
TABLE 45-1 Needle Length for Most Common Peripheral Nerve Blocks
| Type of Block | Length (cm) |
|---|---|
| Interscalene and supraclavicular blocks at the elbow and the wrist | 2.5 |
| Axillary, high humeral, posterior popliteal | |
| Infraclavicular (coracoid) and femoral blocks | 5.0 |
| Lumbar plexus, lateral sciatic, gluteal, and infragluteal | 10.0 |
| Posterior sciatic, anterior sciatic, and high lateral sciatic blocks | 15.0 |
Regional Anesthesia Complications
In the case of a patient with an established difficult airway, the likely complications are those that would lead to the immediate need to secure the airway because of total spinal block, cardiac arrest, or seizure. Among regional techniques, neuraxial blocks have a higher rate of complications.14–19 Closed claim studies have demonstrated that young, healthy patients undergoing surgery during spinal anesthesia can experience sudden cardiac arrest.20 In obstetrics, 70% of the regional anesthesia–related deaths occurred among women who had epidural anesthesia, and the remaining 30% were associated with spinal anesthesia. These deaths resulted when the block became too high for adequate ventilation, and the airway could not be secured, leading to hypoxia or aspiration, or both.21,22
The ASA study of closed claims in obstetrics also showed that about 25% of the anesthesia-related maternal deaths were associated with regional anesthesia. Ananthanarayan and associates presented a case of difficult intubation with brainstem anesthesia after retrobulbar block.23 After failed endotracheal intubation, the airway was secured using a laryngeal mask airway.23 Among the peripheral nerve blocks, lumbar plexus block,24–26 interscalene and axillary brachial plexus block,27–34 intercostal block, and retrobulbar block are those most often associated with complications requiring immediate control of the airway.23 This possibility also exists with the performance of any peripheral nerve block, especially when relatively large volumes of local anesthetic are injected rapidly or when there is a vein or artery located near the nerve.
Local Anesthetics
The choice of the local anesthetic mixture, its volume and concentration, and the mode of administration deserve serious consideration. Although the choices are dictated by the technique (e.g., major conduction blockade versus peripheral nerve blocks), selection of the local anesthetic mixture should be based even more on the safety of patients with a difficult airway, with special focus on possible complications requiring immediate airway intervention. Local anesthetics that have the highest safety profile and provide adequate anesthesia covering the entire surgical period are most suitable. The maximum dose of local anesthetics should be determined to decrease the risk of toxicity. Table 45-2 shows various local anesthetics and their maximum accepted doses.
| Anesthetic | Maximum Dose (mg) | pH |
|---|---|---|
| Lidocaine | 300 | 6.5 |
| Mepivacaine | 500 | 4.5 |
| Bupivacaine | 150 | 4.5-6 |
| Ropivacaine | 225-300 | 4.6 |
2 Proper Anesthetic Setting
In addition to proper expertise in regional anesthesia and difficult airway management, the proper equipment for difficult airway management should be in good order and readily accessible during the entire perioperative period. Support should be available because calling for help is one of the first steps according to the revised version of the airway algorithm.3 The time commitment to manage the airway appropriately should be weighed against the relative availability of the anesthesiologist during the entire perioperative period, because management of the airway may be required intraoperatively. This is especially important when the anesthesiologist supervises more than one location. An anesthesiologist who is supervising residents or certified registered nurse anesthetists or who is on call is not as available as when he or she supervises one location.
C Surgical Environment
1 Type of Surgery
Use of a regional anesthesia technique is not appropriate for all types of operations. For a patient with an established difficult airway, a successful block does not obviate intraoperative management because the patient becomes uncomfortable or there are major hemodynamic changes or bleeding. Regional anesthesia should be considered for shorter procedures with minimal expected blood loss. For example, a short abdominal procedure may benefit from a spinal, epidural, or in some cases, bilateral paravertebral blocks. Diaphragmatic function is not blocked by a spinal or epidural anesthetic, which explains why most anesthesiologists favor the use of neuraxial blocks for low abdominal procedures. In orthopedics, it is important to consider all surgical requirements, especially those related to the use of a tourniquet. Although in surgical procedures of less than 30 minutes’ duration, tourniquet pain is usually not an issue, the mechanism of tourniquet pain should be well understood and managed, because it usually requires sedation or analgesics, or both, that are often contraindicated in patients with unsecured difficult airways (Table 45-3).
TABLE 45-3 Regional Anesthesia Versus Preoperative Management for Difficult Airways
| Approach | Surgical Application |
|---|---|
| Surgeries That Might Be Performed Using Regional Anesthesia | |
| Peripheral nerve blocks | Minor orthopedic trauma of the upper and lower extremity |
| Open reduction with internal fixation of the small finger, elbow, and ankle and wrist fracture | |
| Minor arthroscopy surgery (e.g., shoulder, knee, ankle) | |
| Neuraxial blocks | Gynecologic surgery |
| Cesarean section | |
| Surgeries More Suitable for Preoperative Management | |
| Airway management for long operations associated with major blood loss | Major or multiple trauma |
| Major abdominal surgery | |
| Revised total hip surgery | |
| Major orthopedic oncology surgery | |
| Airway management for long operations performed in the prone position | Spinal surgery |
| Achilles’ tendon surgery | |
| Airway management for blocks unlikely to provide adequate anesthesia | Interscalene block for high humeral fracture |
| Lumbar plexus block for hip surgery | |
V Clinical Pearls
• The decision to perform regional anesthesia should include the surgeon’s opinion.
• Choosing regional anesthesia is easier when intraoperative management of the airway can be easily accomplished during surgery (e.g., lower extremity surgery with the patient in the supine position).
• Performing a regional technique before surgery may help to assess the patient’s level of anxiety and agitation and to confirm whether the choice is the right one.
• The reliability of the surgeon and the type of surgery should weigh heavily in determining whether a regional anesthesia approach is appropriate.
• If regional anesthesia is chosen, it is important to wait for the surgical block to be confirmed.
• The block should be performed as close as possible to the start of surgery.
• The duration of a block is shorter in young patients than in elderly patients.
All references can be found online at expertconsult.com.
10 Delgado Tapia JA, Garcia Sánchez MJ, Priéto Cuellar M, et al. Infraclavicular brachial plexus block using a multiple injection technique and an approach in the cranial direction in a patient with anticipated difficulties in tracheal intubation. Rev Esp Anestesiol Reanim. 2002;49:105–107.
14 Auroy Y, Narchi P, Messiah A, et al. Serious complications related to regional anesthesia: Results of a prospective survey in France. Anesthesiology. 1997;87:479–486.
15 Caplan RA, Ward RJ, Posner K, et al. Unexpected cardiac arrest during spinal anesthesia: A closed claims analysis of predisposing factors. Anesthesiology. 1988;68:5–11.
19 Liguori GA, Sharrock NE. Asystole and severe bradycardia during epidural anesthesia in orthopedic patients. Anesthesiology. 1997;86:250–257.
23 Ananthanarayan C, Cole AF, Kazdan M. Difficult intubation and brain-stem anaesthesia. Can J Anaesth. 1997;44:658–661.
26 Pousman RM, Mansoor Z, Sciard D. Total spinal anesthetic after continuous posterior lumbar plexus block. Anesthesiology. 2003;98:1281–1282.
27 Baraka A, Hanna M, Hammoud R. Unconsciousness and apnea complicating parascalene brachial plexus block: Possible subarachnoid block. Anesthesiology. 1992;77:1046–1047.
28 Cook LB. Unsuspected extradural catheterization in an interscalene block. Br J Anaesth. 1991;67:473–475.
29 Durrani Z, Winnie AP. Brainstem toxicity with reversible lock-in syndrome after intrascalene brachial plexus block. Anesth Analg. 1991;72:249–252.
30 Dutton RP, Eckhardt WF, III., Sunder N. Total spinal anesthesia after interscalene blockade of the brachial plexus. Anesthesiology. 1994;80:939–941.
33 McGlade DP. Extensive central neural blockade following interscalene brachial plexus blockade. Anaesth Intensive Care. 1992;20:514–516.
34 Ross S, Scarsborough CD. Total spinal anesthesia following brachial-plexus block. Anesthesiology. 1972;39:458.
1 Benumof JL. ASA difficult airway algorithm: New thoughts and considerations. In: Hagberg CA, ed. Handbook of difficult airway management. Philadelphia: Churchill Livingstone; 2004:31–48.
2 Hagberg CA, Ghatge S. Does the airway examination predict difficult intubation? In: Fleisher L, ed. Evidence-based practice of anesthesiology. Philadelphia: WB Saunders; 2004:34–46.
3 American Society of Anesthesiologists Task. Force on Management of the Difficult Airway: Practice Guidelines for Management of the Difficult Airway: An updated report by the American Society of Anesthesiologists Task Force on Management of the Difficult Airway. Anesthesiology. 2003;98:1269–1277.
4 Langeron O, Masso E, Huraux C, et al. Prediction of difficult mask ventilation. Anesthesiology. 2000;92:1229–1236.
5 Rocke DA, Murray WB, Rout CC, et al. Relative risk analysis of factors associated with difficult intubation in obstetric anesthesia. Anesthesiology. 1992;77:67–73.
6 Hagberg CA, Iannucci DG, Goodrich AL. An evaluation of endotracheal intubation using the Macintosh video laryngoscopy. Anesth Analg. 2003;96:S157.
7 Hagberg CA, Kaplan MB, Lazada L, et al. The experience of four American clinics with the Macintosh video laryngoscopy. Eur J Anaesthesiol. 2003;20:A–164.
8 Kheterpal S, Han R, Tremper KK, et al. Incidence and predictors of difficult and impossible mask ventilation. Anesthesiology. 2006;105:885–891.
9 Kheterpal S, Martin I, Shanks AM, Tremper KK. Prediction and outcomes of impossible mask ventilation: a review of 50,000 anesthetics. Anesthesiology. 2009;110:891–897.
10 Delgado Tapia JA, Garcia Sánchez MJ, Priéto Cuellar M, et al. Infraclavicular brachial plexus block using a multiple injection technique and an approach in the cranial direction in a patient with anticipated difficulties in tracheal intubation. Rev Esp Anestesiol Reanim. 2002;49:105–107.
11 Gil S, Jamart V, Borrás R, et al. Airway management in a man with ankylosing spondylitis. Rev Esp Anestesiol Reanim. 2007;54:128–131.
12 Khanna R, Singh DK. Cervical epidural anaesthesia for thyroid surgery. Kathmandu Univ Med J (KUMJ). 2009;7:242–245.
13 Knapik P, Przybylski R, Nadziakiewicz P, et al. Awake heart valve surgery in a patient with severe pulmonary disease. Ann Thorac Surg. 2008;86:293–295.
14 Auroy Y, Narchi P, Messiah A, et al. Serious complications related to regional anesthesia: Results of a prospective survey in France. Anesthesiology. 1997;87:479–486.
15 Caplan RA, Ward RJ, Posner K, et al. Unexpected cardiac arrest during spinal anesthesia: A closed claims analysis of predisposing factors. Anesthesiology. 1988;68:5–11.
16 Chester WL. Spinal anesthesia, complete heart block, and the precordial chest thump: An unusual complication and a unique resuscitation. Anesthesiology. 1988;69:600–602.
17 Frerichs RL, Campbell J, Bassell GM. Psychogenic cardiac arrest during extensive sympathetic blockade. Anesthesiology. 1988;68:943–944.
18 Hodgkinson R. Total spinal block after epidural injection into an interspace adjacent to an inadvertent dural perforation. Anesthesiology. 1981;55:593–595.
19 Liguori GA, Sharrock NE. Asystole and severe bradycardia during epidural anesthesia in orthopedic patients. Anesthesiology. 1997;86:250–257.
20 Cheney FW. The American Society of Anesthesiologists Closed Claims Project: What have we learned, how has it affected practice, and how will it affect practice in the future? Anesthesiology. 1999;91:552–556.
21 Hawkins JL. Anesthesia-related maternal mortality. Clin Obstet Gynecol. 2003;46:679–687.
22 Ross BK. ASA closed claims in obstetrics: Lessons learned. Anesthesiol Clin North Am. 2003;21:183–197.
23 Ananthanarayan C, Cole AF, Kazdan M. Difficult intubation and brain-stem anaesthesia. Can J Anaesth. 1997;44:658–661.
24 Lonnqvist PA, MacKenzie J, Soni AK, et al. Paravertebral blockade: Failure rate and complications. Anaesthesia. 1995;50:813–815.
25 Muravchick S, Owens WD. An unusual complication of lumbosacral plexus block: A case report. Anesth Analg. 1976;55:350–352.
26 Pousman RM, Mansoor Z, Sciard D. Total spinal anesthetic after continuous posterior lumbar plexus block. Anesthesiology. 2003;98:1281–1282.
27 Baraka A, Hanna M, Hammoud R. Unconsciousness and apnea complicating parascalene brachial plexus block: Possible subarachnoid block. Anesthesiology. 1992;77:1046–1047.
28 Cook LB. Unsuspected extradural catheterization in an interscalene block. Br J Anaesth. 1991;67:473–475.
29 Durrani Z, Winnie AP. Brainstem toxicity with reversible lock-in syndrome after intrascalene brachial plexus block. Anesth Analg. 1991;72:249–252.
30 Dutton RP, Eckhardt WF, III., Sunder N. Total spinal anesthesia after interscalene blockade of the brachial plexus. Anesthesiology. 1994;80:939–941.
31 Edde RR, Deutsch S. Cardiac arrest after interscalene brachial-plexus block. Anesth Analg. 1977;56:446–447.
32 Kumar A, Battit GE, Froese AB, et al. Bilateral cervical and thoracic epidural blockade complicating interscalene brachial plexus block: Report of two cases. Anesthesiology. 1971;35:650–652.
33 McGlade DP. Extensive central neural blockade following interscalene brachial plexus blockade. Anaesth Intensive Care. 1992;20:514–516.
34 Ross S, Scarsborough CD. Total spinal anesthesia following brachial-plexus block. Anesthesiology. 1972;39:458.