Dilatation of intrahepatic and extrahepatic biliary ducts
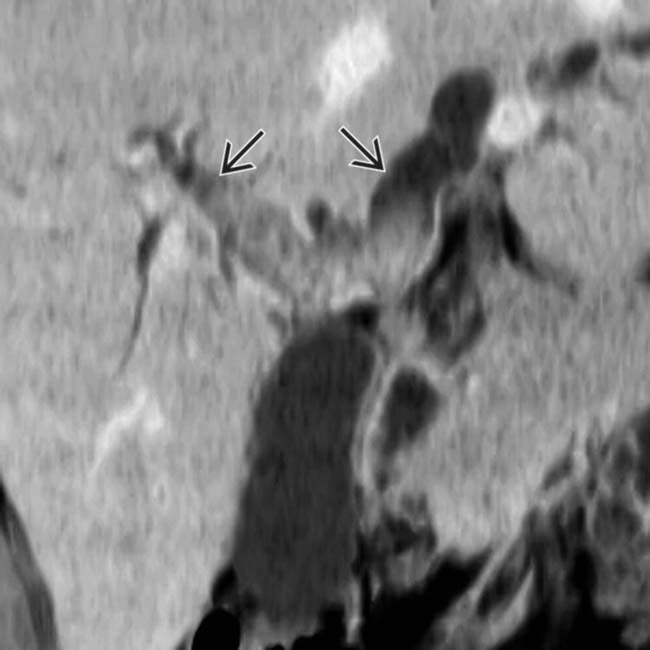
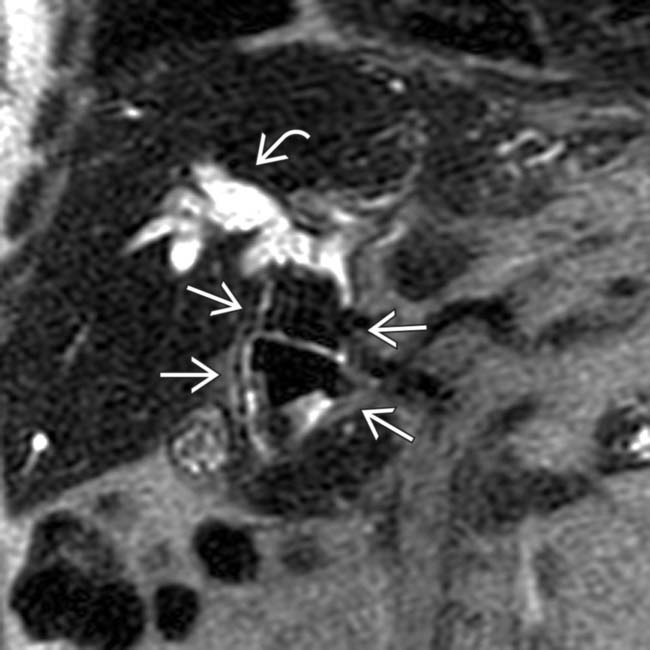
– MRCP nicely illustrates ↓ arborization of peripheral ducts, multiple intrahepatic biliary strictures, and rapidly tapering intrahepatic ducts (arrowhead sign)

 . This patient later underwent surgery with a choledochoenterostomy.
. This patient later underwent surgery with a choledochoenterostomy.
 . Notice the multiple low signal stones
. Notice the multiple low signal stones  within the left hepatic ducts.
within the left hepatic ducts.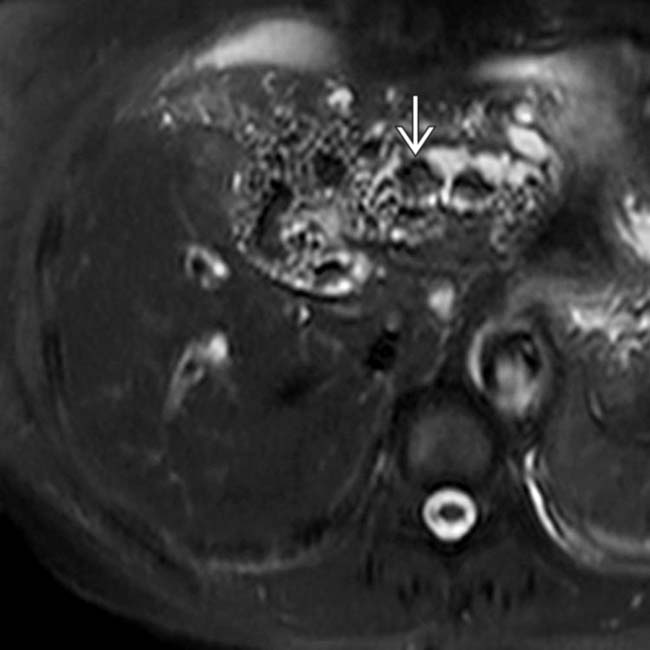
 . Note that the left lobe is mildly atrophic with subtly increased T2 signal. The findings in this case are classic for RPC.
. Note that the left lobe is mildly atrophic with subtly increased T2 signal. The findings in this case are classic for RPC.IMAGING
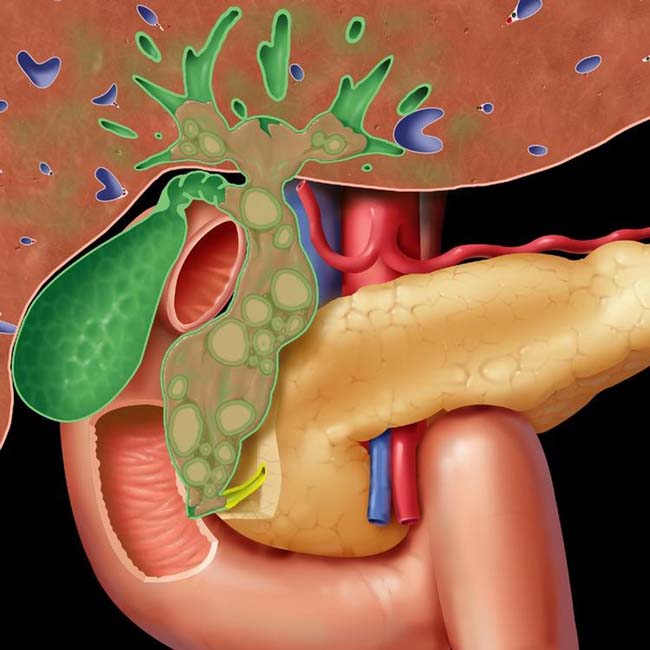
General Features
CT Findings
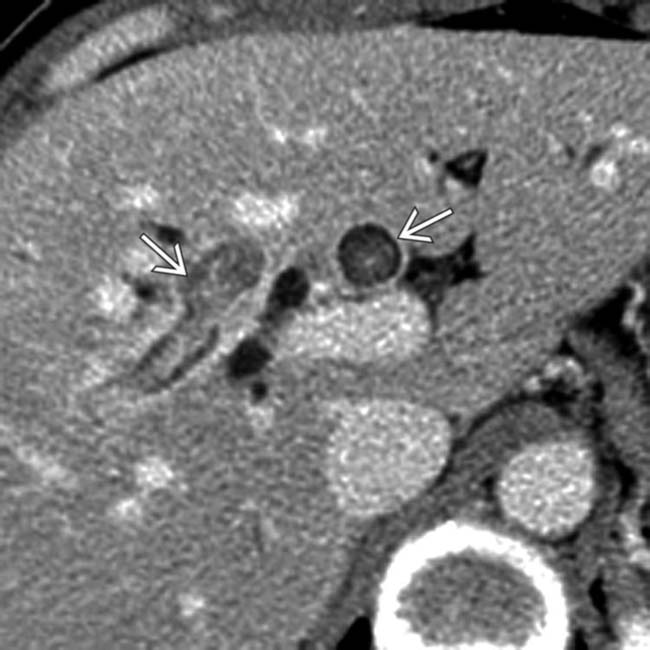
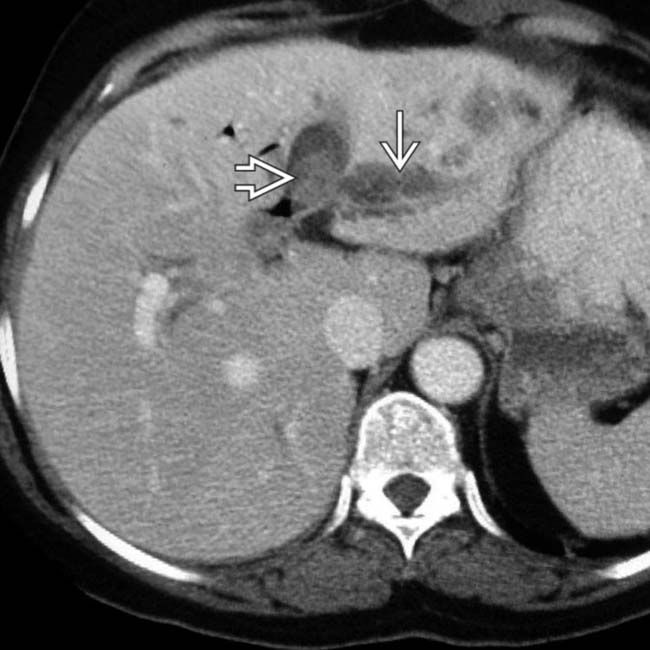
• Dilatation of intrahepatic and extrahepatic biliary ducts
 Disproportionate dilatation of extrahepatic and central intrahepatic bile ducts: CBD may be markedly enlarged
Disproportionate dilatation of extrahepatic and central intrahepatic bile ducts: CBD may be markedly enlarged
 Disproportionate dilatation of extrahepatic and central intrahepatic bile ducts: CBD may be markedly enlarged
Disproportionate dilatation of extrahepatic and central intrahepatic bile ducts: CBD may be markedly enlarged
MR Findings
• Dilatation of intrahepatic and extrahepatic bile ducts, with disproportionate dilatation of extrahepatic and central intrahepatic ducts
 MRCP nicely illustrates ↓ arborization of peripheral ducts, multiple intrahepatic biliary structures, and rapidly tapering intrahepatic ducts (arrowhead sign)
MRCP nicely illustrates ↓ arborization of peripheral ducts, multiple intrahepatic biliary structures, and rapidly tapering intrahepatic ducts (arrowhead sign)
 MRCP nicely illustrates ↓ arborization of peripheral ducts, multiple intrahepatic biliary structures, and rapidly tapering intrahepatic ducts (arrowhead sign)
MRCP nicely illustrates ↓ arborization of peripheral ducts, multiple intrahepatic biliary structures, and rapidly tapering intrahepatic ducts (arrowhead sign)
PATHOLOGY
General Features
• Etiology
 Precise etiology is not completely understood, but likely related to parasitic or bacterial infection of biliary tree
Precise etiology is not completely understood, but likely related to parasitic or bacterial infection of biliary tree
 Different theories based on geographic clustering of disease (suggestive of role of epidemiologic factors)
Different theories based on geographic clustering of disease (suggestive of role of epidemiologic factors)
 Precise etiology is not completely understood, but likely related to parasitic or bacterial infection of biliary tree
Precise etiology is not completely understood, but likely related to parasitic or bacterial infection of biliary tree Different theories based on geographic clustering of disease (suggestive of role of epidemiologic factors)
Different theories based on geographic clustering of disease (suggestive of role of epidemiologic factors)
– Parasitic infection
CLINICAL ISSUES
Presentation
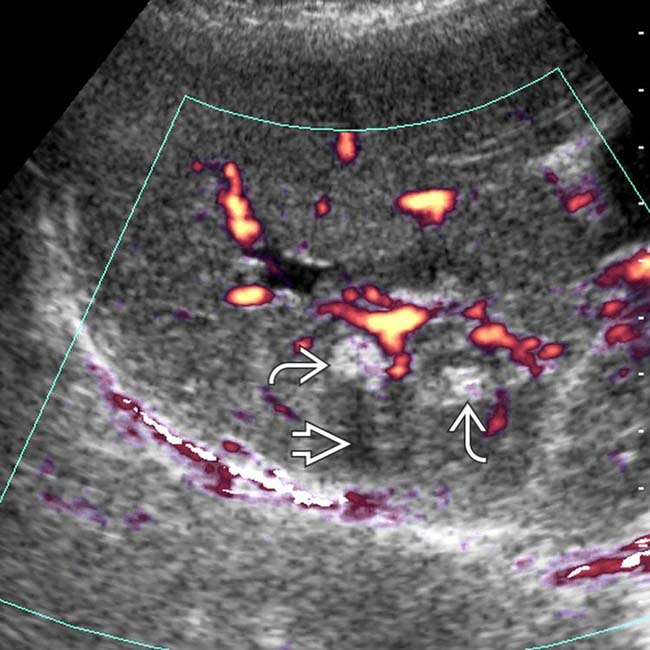
 . Note the posterior acoustic shadowing
. Note the posterior acoustic shadowing  . In a patient from Southeast Asia, these imaging findings are characteristic of RPC.
. In a patient from Southeast Asia, these imaging findings are characteristic of RPC.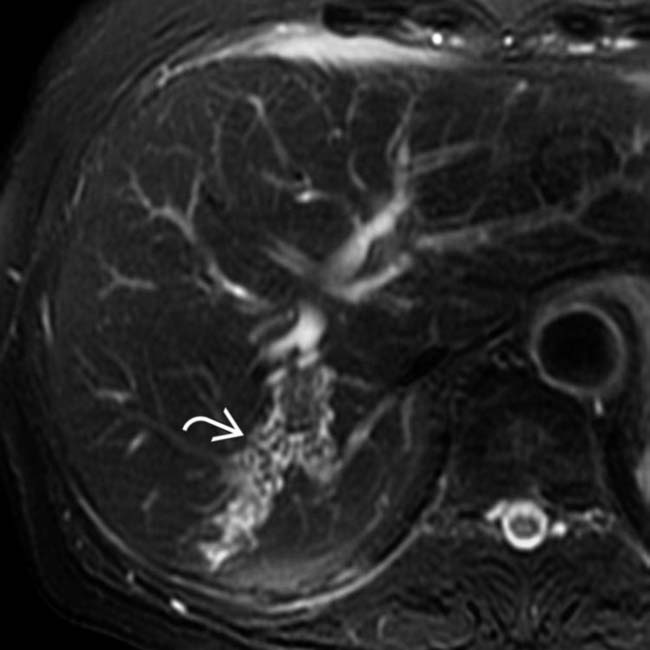
 with multiple low-signal internal stones. Localized involvement of the right posterior ducts is less common in RPC than localized involvement of the left lobe ducts.
with multiple low-signal internal stones. Localized involvement of the right posterior ducts is less common in RPC than localized involvement of the left lobe ducts.
 within dilated left lobe bile ducts, and gas
within dilated left lobe bile ducts, and gas  within a hepatic abscess in the right hepatic lobe.
within a hepatic abscess in the right hepatic lobe.
 , and a stone in the right posterior bile duct
, and a stone in the right posterior bile duct  .
.
 . Note the absence of peripheral biliary ductal dilatation.
. Note the absence of peripheral biliary ductal dilatation.
 , with an adjacent heterogeneous, solid mass
, with an adjacent heterogeneous, solid mass  within the left lobe that proved to represent a cholangiocarcinoma. RPC is a known risk factor for the development of cholangiocarcinoma.
within the left lobe that proved to represent a cholangiocarcinoma. RPC is a known risk factor for the development of cholangiocarcinoma.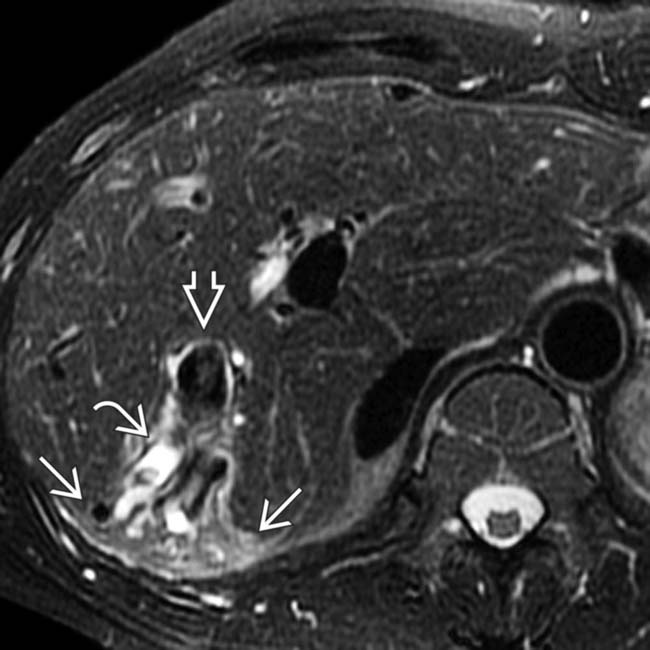
 , a right biliary calculus
, a right biliary calculus  , peripheral atrophy, and increased parenchymal T2 signal
, peripheral atrophy, and increased parenchymal T2 signal  , characteristic of RPC.
, characteristic of RPC.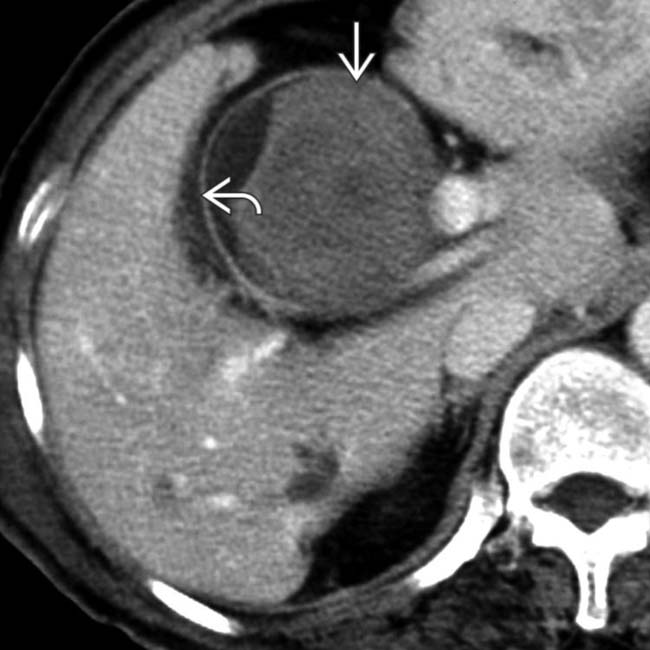
 adjacent to a small crescent of low-attenuation bile
adjacent to a small crescent of low-attenuation bile  .
.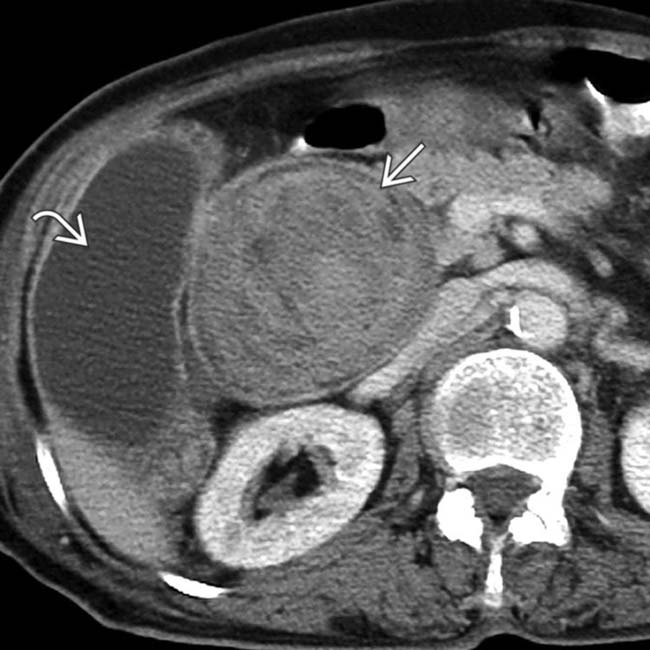
 . Note that there are no stones in the normal-appearing gallbladder
. Note that there are no stones in the normal-appearing gallbladder  .
.
 , later cleared by a basket sweep of the duct.
, later cleared by a basket sweep of the duct.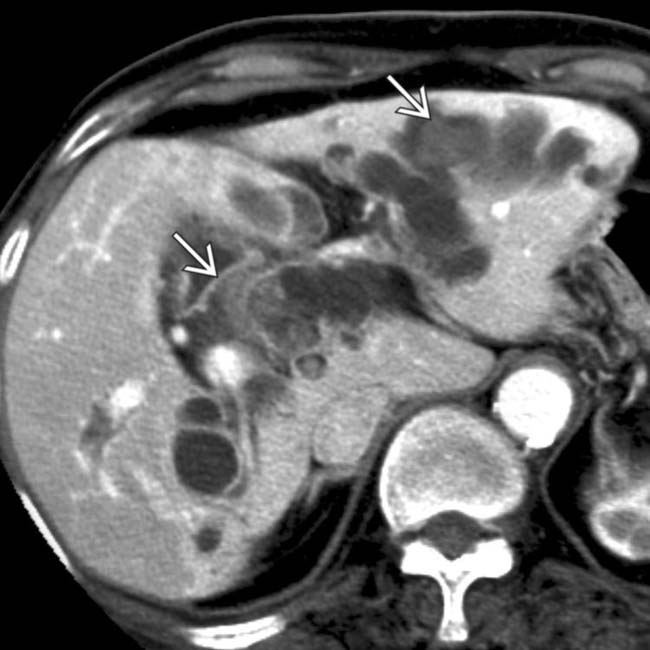
 .
.
 .
.
 .
.
 and multiple large stones within a massively dilated extrahepatic duct
and multiple large stones within a massively dilated extrahepatic duct  .
.
 involving the left ductal system, and a filling defect due to pigment calculus
involving the left ductal system, and a filling defect due to pigment calculus  . As the calculi are predominantly composed of pigment, they are not as dense as calculi containing calcium.
. As the calculi are predominantly composed of pigment, they are not as dense as calculi containing calcium.
 seen in the lateral segment of the left lobe. Abscesses are a common complication in patients with RPC.
seen in the lateral segment of the left lobe. Abscesses are a common complication in patients with RPC.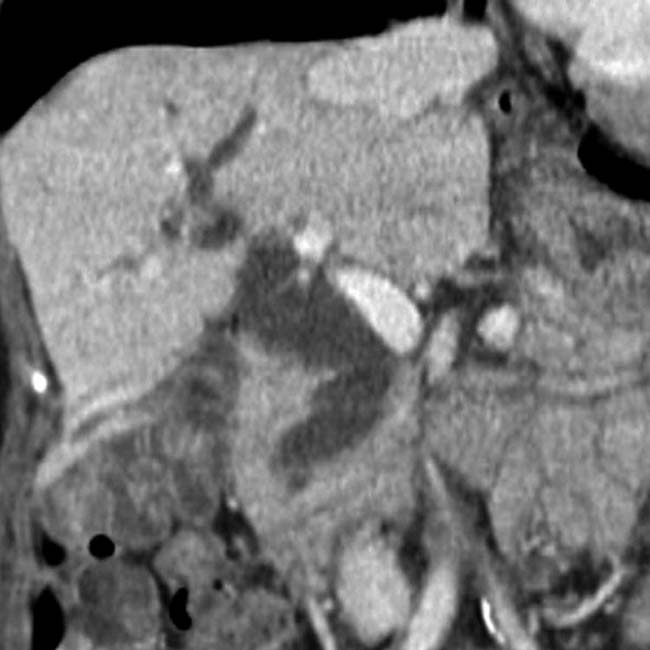

 , which are dilated out of proportion to the right lobe ducts. The CT findings in this case are classic for recurrent pyogenic cholangitis, consisting of chronic infection and stone formation within the biliary system, usually without gallbladder stones.
, which are dilated out of proportion to the right lobe ducts. The CT findings in this case are classic for recurrent pyogenic cholangitis, consisting of chronic infection and stone formation within the biliary system, usually without gallbladder stones.








































































