Reconstruction of the Ulnar Collateral Ligament with Ulnar Nerve Transposition
Mark T. Bastan, Michael M. Reinold, Kevin E. Wilk and James R. Andrews
The ulnar collateral ligament (UCL) is the elbow’s primary stabilizer to valgus stress within a functional range of motion (ROM). For the overhead-throwing athlete, throwing motions promote valgus stress at the elbow that exceeds the ultimate tensile strength of the UCL. Repetitive throwing motions produce cumulative microtraumatic damage and may eventually cause the ligament to overstretch and create symptomatic medial elbow instability. To correct this, both surgical intervention and a carefully coordinated rehabilitation program are required if the athlete is to return to full, pain-free function. This chapter describes the way the anatomy and biomechanics of the elbow can be applied to a scientifically based rehabilitation program for use after UCL reconstruction.
Surgical Indications And Considerations
Bony Structures
The elbow joint has three articulations: the humeroulnar, humeroradial, and superior radioulnar joints. Collectively these joints may be classified as trochoginglymoid1 and are enclosed by a single joint capsule.
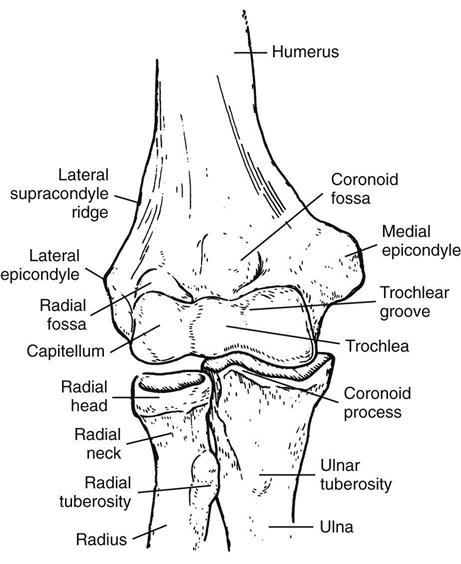
The humeroulnar joint is a single-axis diarthrodial joint with 1° of freedom—flexion and extension. The bony structures of the joint include the distal humerus and proximal ulna (Fig. 9-1). The distal humerus flares to form the medial and lateral epicondyles, which are directly above the capitellum and trochlea, respectively. The medial epicondyle is much more prominent than the lateral epicondyle; the UCL and flexor-pronator muscle group attach to it (Fig. 9-2). The flat, irregular surface of the lateral epicondyle serves as the attachment site for the lateral collateral ligament and the supinator-extensor muscle groups. Just posterior to the medial epicondyle is the cubital tunnel, or ulnar groove, a key depression that protects and houses the ulnar nerve. Immediately above the anterior articular surface of the humerus is a bony depression called the coronoid fossa. The olecranon process of the ulna glides into this concavity during flexion. The olecranon fossa, located on the posterior aspect of the humerus, accepts the large olecranon process during extension. The proximal ulna provides the major articulation of the elbow and is responsible for its inherent stability. The trochlear ridge is a bony projection running from the olecranon posteriorly to the coronoid process anteriorly. The trochlear notch is a concave surface located on either side of the trochlear ridge; it forms a close articulation with the humeral trochlea.
The proximal radius and distal lateral aspect of the humerus articulate to form the humeroradial joint, which is also a single-axis diarthrodial joint. Similar to the humeroulnar joint, the humeroradial joint contributes to flexion and extension movements by gliding around the coronal axis. However, the humeroradial articulation also pivots around a longitudinal axis with the superior radioulnar joint to perform rotational movements. The proximal radial head is mushroom shaped,2 with a central depression located above it. The radial head narrows distally to form the radial neck. The head and neck are not colinear, with the shaft of the radius forming an angle of approximately 15°. Further distal is the radial tuberosity, where the biceps tendon attaches. In the distal humerus the capitellum is almost spheric. A groove (the capitotrochlear groove) separates the capitellum from the trochlea. The rim of the radial head articulates with this groove throughout the arc of flexion and during pronation and supination.
The superior and inferior radioulnar joints function as single-axis diarthrodial joints that allow the elbow to pronate and supinate. Proximally, the convex medial rim of the radial head articulates with the concave radial ulnar notch. During supination and pronation, the radial head rotates within a ring formed by the annular ligament and radial ulnar notch. An interosseous membrane connects the shafts of the radius and ulna to form a syndesmosis. Distally, the ulnar head with the radial ulnar notch forms the inferior radioulnar joint articulation. This joint is L-shaped and has an articular disk between the lower ends of the radius and ulna. During supination and pronation, the ulnar notch and articular disk swing on the ulnar head.
Ligamentous Structures
A single joint capsule surrounds the elbow joint and is lined by a synovial membrane. Specialized thickenings of the medial and lateral capsule form the collateral ligament complexes.
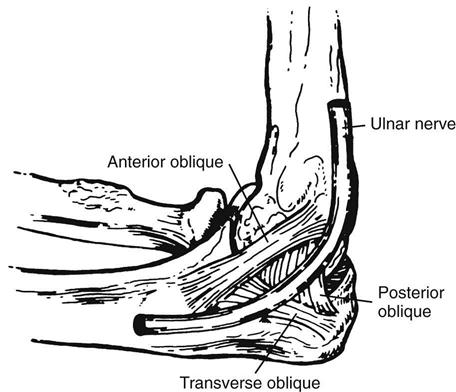
The UCL is traditionally described as having three portions: the anterior, posterior, and transverse bundles (Fig. 9-3).2 The anterior bundle of the UCL is the strongest and most discrete component, coursing from the medial epicondyle to the sublime tubercle on the medial coronoid margin. The anterior bundle consists of two layers: (1) a thickening within the capsular layers and (2) an added complex superficial to the capsular layers.3 The anatomic design of this ligament makes pathologic conditions in the central portion of the anterior bundle (as seen in a chronic, attenuated state) difficult to see during arthroscopic surgery. Functionally, the UCL is subdivided into two bands: (1) the anterior band, which is tight in extension, and (2) the posterior band, which is taut in flexion.4
The anterior oblique bundle of the UCL is the primary stabilizer to valgus stress at the elbow. Compromise of this structure causes gross instability in all elbow positions except full extension. The fan-shaped posterior bundle runs from the medial epicondyle to the middle margin of the trochlear notch. This band becomes especially taut in flexion beyond 60°,5,6 but sectioning the posterior oblique ligament does not significantly affect medial elbow stability.7 The transverse ligament (also known as the Cooper ligament) has an ulnar-to-ulnar attachment and contributes minimally to elbow stability.5
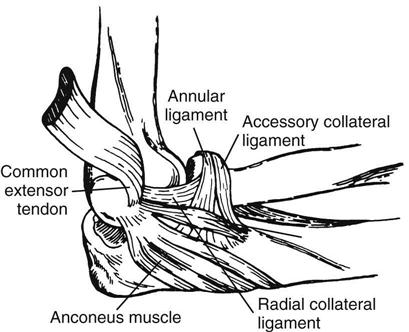
The anatomy of the lateral collateral ligament complex can vary significantly.8,9 Typically four components are found: (1) the radial collateral ligament (RCL), (2) the annular ligament, (3) the lateral UCL, and (4) the accessory lateral collateral ligament (Fig. 9-4). The RCL originates from the lateral epicondyle and terminates on the annular ligament. It provides varus stability by maintaining close approximation of the humeral and radial articular surfaces.8 The annular ligament is a strong band of tissue encompassing and stabilizing the radial head in the radial ulnar notch. The anterior part of this ligament becomes taut with extreme supination and the posterior portion with extreme pronation.10 The lateral UCL originates at the midportion of the lateral epicondyle, passes over the annular ligament, and attaches to the tubercle of the supinator. This ligament is analogous to the anterior band of the UCL and is the primary lateral stabilizer of the elbow, preventing posterolateral rotary instability.9 Finally, the accessory lateral collateral ligament extends proximally from the inferior margin of the annular ligament and attaches distally on the tubercle of the supinator crest.
It further stabilizes the annular ligament during varus stress.5,9–11
Muscular Structures
The musculature surrounding the elbow joint may be divided into four main groups:
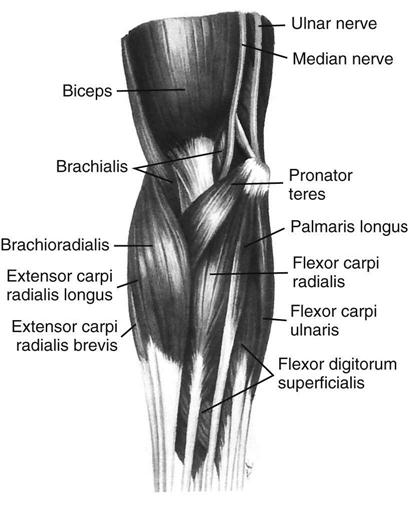
The flexor group is located anteriorly and comprises the biceps brachii, brachialis, and brachioradialis muscles. The biceps brachii acts both as a major elbow flexor and as a supinator of the forearm (primarily with the elbow flexed), with a distal insertion at the radial tuberosity and bicipital aponeurosis, which attaches to the anterior capsule of the elbow. The brachioradialis originates at the proximal two thirds of the lateral supracondylar ridge of the humerus and attaches distally at the base of the styloid process of the radius, giving it the greatest mechanical advantage of the elbow flexors. The cross-sectional area of the brachialis is the largest of the elbow flexors, but this has no mechanical advantage because it crosses so closely to the axis of rotation. As the brachialis crosses the anterior capsule, some muscle fibers insert into the capsule and help retract the capsule during flexion.
The anconeus and triceps brachii perform elbow extension and are located posteriorly. The triceps brachii has three heads (long, lateral, and medial) proximally that converge distally to form a single insertion at the posterior olecranon. The much smaller anconeus originates at the posterior aspect of the lateral epicondyle and inserts on the dorsal surface of the proximal ulna. Besides extending the elbow, the anconeus may be a lateral joint stabilizer.
The flexor-pronator muscles, which all originate completely or in part at the medial epicondyle, include the pronator teres, flexor carpi radialis, palmaris longus, flexor carpi ulnaris, and flexor digitorum superficialis. The primary role of these muscles is in hand and wrist function, but they also act as elbow flexors and dynamically stabilize the medial aspect of the elbow.
Finally, the extensor supinator muscles include the brachioradialis, extensor carpi radialis brevis and longus, supinator, extensor digitorum, extensor carpi ulnaris, and extensor digiti minimi. Each of these muscles originates near or directly onto the lateral epicondyle of the humerus and provides dynamic support over the lateral aspect of the elbow.
Neurologic Structures
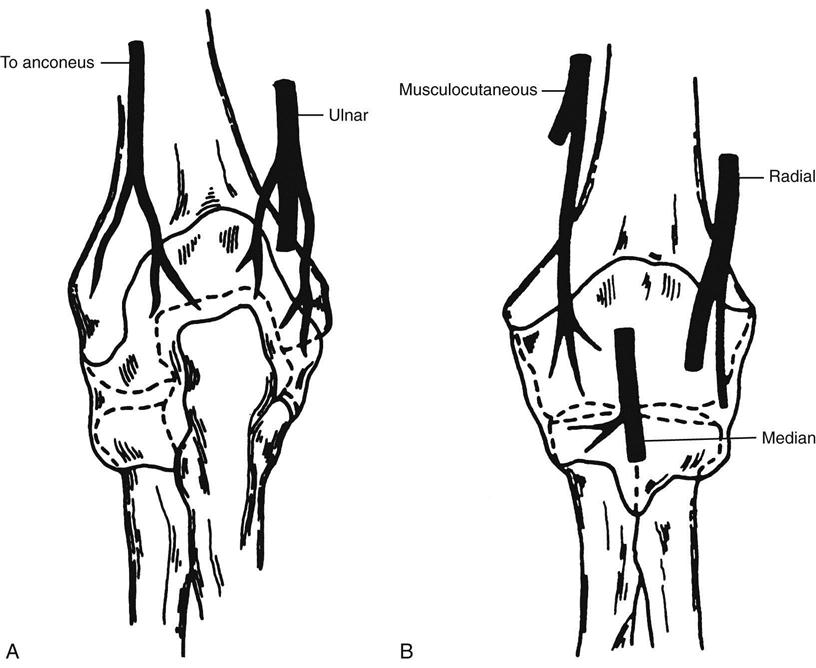
The relationship of neurologic structures coursing through the elbow to their surrounding features can be crucial to function, pathologic conditions, and treatment (Fig. 9-5). The radial nerve descends anterior to the lateral epicondyle, behind the brachioradialis and brachialis muscles. At the antecubital space, the nerve divides into superficial and deep branches, with the superficial branch continuing distally in front of the lateral epicondyle and running under the brachioradialis muscle while on top of the supinator and pronator teres muscles. The deep branch pierces the supinator, travels around the posterolateral radial neck, and emerges distally 8 cm below the elbow joint to the terminal motor branches.
The median nerve follows a straight course into the medial aspect of the antecubital fossa, medial to the biceps tendon and brachial artery. From the antecubital fossa, the median nerve continues under the bicipital aponeurosis and usually passes between the two heads of the pronator teres, then travels below the flexor digitorum superficialis.
The musculocutaneous nerve innervates the major elbow flexors of the anterior brachium, then passes between the biceps and brachialis muscles to pierce the brachial fascia lateral to the biceps tendon. It continues distally to terminate as the lateral antebrachial cutaneous nerve, providing sensation over the lateral forearm.
Finally, the ulnar nerve travels anterior to posterior in the brachium through the arcade of Struthers. It then extends around the medial epicondyle and through the cubital tunnel. The cubital tunnel is the most frequent site for ulnar nerve injury; length changes in the medial ligament structures during elbow flexion can lead to significant reduction of the volume of the cubital tunnel, resulting in ulnar nerve compression.12 This compression occurs as the cubital retinaculum, which forms a roof over the cubital tunnel, tightens with elbow flexion.13 Absence of the cubital tunnel retinaculum has been associated with congenital ulnar nerve subluxation. After passing through the cubital tunnel, the ulnar nerve enters the forearm by traveling between the two heads of the flexor carpi ulnaris.
Cause
Injury to the UCL and resultant medial elbow instability are secondary to valgus loads that exceed the ultimate tensile strength of the ligament. Although excessive valgus loads may be secondary to trauma, as with an elbow dislocation caused by a fall or playing a sport such as football or wrestling, the most common mechanisms of injury are associated with repetitive overhead activities, such as baseball, javelin throwing, tennis, swimming, and volleyball. The single largest patient population experiencing medial elbow instability is undoubtedly overhead throwers.14 This is secondary to the tremendous forces imparted to the elbow joint during the overhead-throwing motion.
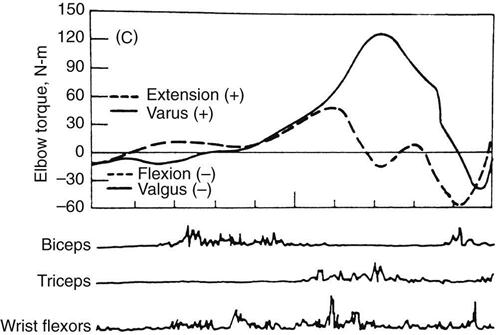
The initiation of valgus stress occurs at the conclusion of the arm-cocking stage. The thrower’s shoulder is abducted, extended, and externally rotated about 130°, with the elbow flexed at about 90°. In transition from cocking to acceleration, the shoulder then internally rotates and the elbow flexes another 20° to 30°; this further increases the valgus load on the medial elbow. As the arm continues to accelerate, the elbow extends from about 125° to 25° of flexion at ball release.15,16 Dillman, Smutz, and Werner17 report that mean ultimate valgus torque measured from cadaveric testing was 33 N-m (newton-meters) (Fig. 9-6). During analysis of the dynamic demands of the pitching motion, Fleisig and associates18 estimate that 35 N-m of valgus torque is placed on the UCL. The flexor carpi ulnaris and flexor digitorum superficialis muscles are located directly over the anterior band of the UCL and assist in combating medial joint distraction forces during the throwing motion. With any increased load transmitted to the UCL—whether with improper mechanics, warm-up, or conditioning—the structural integrity of the primary medial stabilizer of the elbow may be compromised.
Injuries to the UCL are described as either acute or chronic. An acute rupture of the UCL is frequently associated with a “pop,” a feeling of pain during late acceleration or at ball release; it is often accompanied by swelling. More commonly, chronic injuries to the ligament are seen in the overhead-throwing athlete.19 These occur from the accumulated repetitive microtrauma of overloading the ligament with throwing and can result in symptomatic medial elbow instability.20 Accurate identification of medial instability is often difficult with clinical examination alone because laxity is only slightly increased. In addition, performing valgus laxity assessment is often difficult because of humeral rotation. Often magnetic resonance imaging (MRI) is used to confirm diagnosis. Timmerman, Schwartz, and Andrews21 believe that use of saline-enhanced MRI improves the results when a UCL tear is suspected. The authors of this chapter have found a typical leakage of contrast fluid around the ulnar insertion of the UCL when an undersurface tear is present, which has been called the T-sign.22
Surgical reconstruction of the UCL is indicated in athletes who have persistent medial elbow pain, cannot throw or participate in desired sports, show documented valgus laxity, and fail a 6-month conservative course of treatment.
Surgical Procedure
The goal of reconstruction is to restore the static stability of the anterior bundle of the UCL. The surgical procedure used at the authors’ center by Dr. James Andrews is a modification of an earlier technique.
The presence or absence of the palmaris longus must be documented before surgery because it is the preferred donor tendon. If it is not present, then alternate donor sites must be evaluated, including the contralateral palmar longus, the plantaris tendon, and the extensor tendon from the fourth toe.
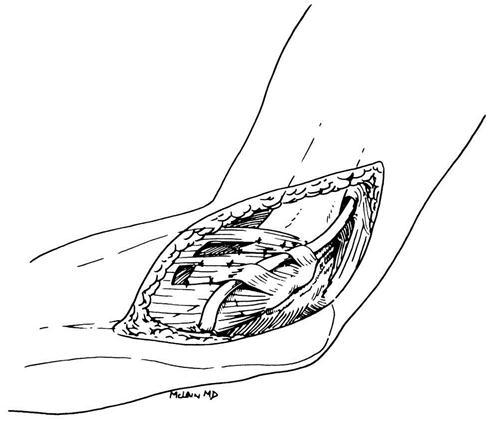
Surgery to correct for valgus instability is initiated with a brief arthroscopic evaluation. The procedure itself begins with arthroscopic examination to assess the integrity of the intraarticular structures and valgus instability. After that is completed, a medial incision is made with subcutaneous ulnar nerve transposition. The incision is centered over the medial epicondyle and extends about 3 cm proximally and distally (Fig. 9-7). The medial antebrachial cutaneous nerve is identified, preserved, and protected during the procedure to avoid neuroma development. After elevating the skin flaps to expose the deep fascia covering the flexor pronator muscles, the surgeon identifies the ulnar nerve. Anterior transposition of the ulnar nerve must be performed before the medial ligament complex is explored. To do so, the cubital tunnel is first incised to mobilize the nerve. Proximally, the mobilization continues to include the arcade of Struthers, and a portion of the intermuscular septum is excised to prevent impingement of the nerve as it is transposed anteriorly. Distally, the flexor carpi ulnaris is incised along the course of the nerve. The ulnar nerve is then transposed anteriorly and preserved throughout the remainder of the procedure.
To complete visualization of the UCL, the split in the flexor carpi ulnaris is followed down to the insertion of the anterior band of the UCL on the sublime tubercle of the ulna. Starting at the insertion of the ulna, the surgeon develops the interval between the UCL and flexor muscle mass, extending proximally to the medial epicondyle. The flexor muscles are then retracted anteriorly to provide full exposure to the ligament, at which point the pathologic condition can be assessed. In a complete rupture, the joint is exposed. If the external surface appears normal, then a longitudinal incision is made in line with the fibers of the anterior bundle. This incision may reveal pathology, including tissue discoloration, fraying of the tissue, and detachment from the bony insertion on the ulna indicative of an undersurface tear, as described by Timmerman and Andrews.23
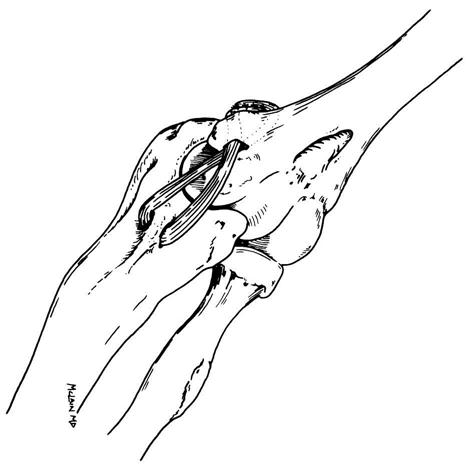
The remnants of the ligament are preserved and augmented with the tendon graft. After the donor tendon has been secured, muscle is stripped off the graft, the ends are trimmed, and a nonabsorbable suture is placed at each end with a locking stitch to help graft passage. Two drill holes are made at right angles just anterior and posterior to the sublime tubercle at the level of insertion of the anterior bundle. The drill holes are then connected with curettes and a towel clip. Proximally, two convergent tunnels are drilled to meet at the insertion of the ligament on the medial epicondyle. The graft is then passed through the ulna and crossed in a figure eight across the joint. Each end is then brought out through the two tunnels at the humerus end. If the graft is long enough, then one end is passed through a second time. The graft tension is adjusted with the elbow in 30° of flexion and by application of a varus stress. The graft is then secured with nonabsorbable 2-0 sutures over the medial epicondyle. The remaining ligament is sutured to the graft for added stability, and the flexor carpi ulnaris is loosely closed (Fig. 9-8).
Ulnar nerve transposition is now completed. An incision is made in the flexor pronator fascia, leaving attachments at the medial epicondyle; these flaps are about 3 cm long and 1 cm wide. Muscle is dissected away from the fascia, and the defect is closed to prevent herniation. The nerve is then transferred subcutaneously and anteriorly to lie under the fascial flaps. The flaps are reattached loosely to provide a sling to keep the nerve in position without compressing it. A drain is placed subcutaneously, and the skin is closed with an absorbable 3-0 subcuticular suture.
Therapy Guidelines For Rehabilitation
Rehabilitation after UCL reconstruction should match the surgery used and meet the needs of the patient, which include additional care for the individual’s specific donor site. The following guidelines are based on the procedure just described and are geared to the overhead-throwing athlete. The complete rehabilitation program is outlined in the home maintenance box.
Phase I
TIME: 1 to 3 weeks after surgery
GOALS: Decrease pain and inflammation, retard muscle atrophy, protect healing tissues (Table 9-1)
TABLE 9-1
< ?comst?>
| Rehabilitation Phase | Criteria to Progress to This Phase | Anticipated Impairments and Functional Limitations | Intervention | Goal | Rationale |
| Phase I Postoperative 1-3 wk |
Postoperative |
At 2 wk, add wrist flexion and extension |
|
< ?comen?>< ?comst1?>
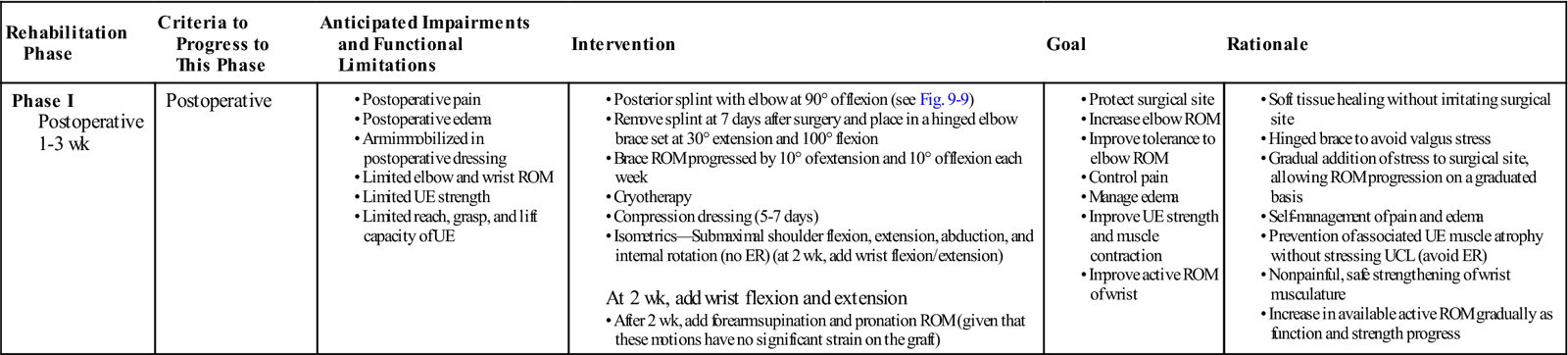
< ?comst1?>
< ?comen1?>
ER, External rotation; ROM, range of motion; UCL, ulnar collateral ligament; UE, upper extremity.
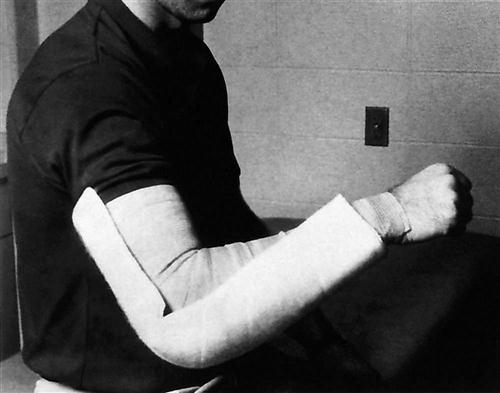
The patient should be placed in a posterior elbow splint at 90° of flexion (Fig. 9-9), which allows initial healing of the UCL graft and soft tissue healing of the fascial slings for the transferred ulnar nerve.24 Edema and pain are managed with frequent gripping exercises, cryotherapy, and a bulky dressing. The dressing is applied immediately after surgery and is removed between postoperative days 5 and 7.
![]() The therapist initiates submaximal shoulder isometrics (except external rotation, which promotes a valgus stress at the elbow) and active wrist ROM to prevent neuromuscular inhibition.
The therapist initiates submaximal shoulder isometrics (except external rotation, which promotes a valgus stress at the elbow) and active wrist ROM to prevent neuromuscular inhibition.
The therapist evaluates ulnar nerve function postoperatively and frequently throughout the rehabilitation process. Paresthesia and impaired motor function occur at rates as high as 31% with intramuscular ulnar nerve transposition. The procedure described in this chapter uses fascial slings to complete transposition of the nerve, so the chance of postoperative neurologic complications is extremely low, usually less than 3%.
![]() Compression wraps that are too tight and ill-fitting braces also may lead to transient ulnar nerve paresthesia and should be carefully assessed.
Compression wraps that are too tight and ill-fitting braces also may lead to transient ulnar nerve paresthesia and should be carefully assessed.
Early ROM and frequent assessment are vital in the early rehabilitative process. After 7 days, the posterior splint is removed and the elbow placed in a hinged brace set at 30° to 100° (Fig. 9-10). ROM is then advanced weekly by 10° of extension and 10° of flexion. Forearm supination and pronation ROM are assessed and progressed in postoperative week 2, given that these motions have no significant effect on graft strain.25 During the third postoperative week, active range of motion (AROM) for the wrist, elbow, and shoulder may be initiated.
Phase II
TIME: 4 to 7 weeks after surgery
GOALS: Gradually increase ROM, heal tissues, restore muscular strength (Table 9-2)
TABLE 9-2
< ?comst?>
| Rehabilitation Phase | Criteria to Progress to This Phase | Anticipated Impairments and Functional Limitations | Intervention | Goal | Rationale |
| Phase II Postoperative 4-8 wk |
Continue exercises as in phase I as indicated |
0°-145° |
|
< ?comen?>< ?comst1?>
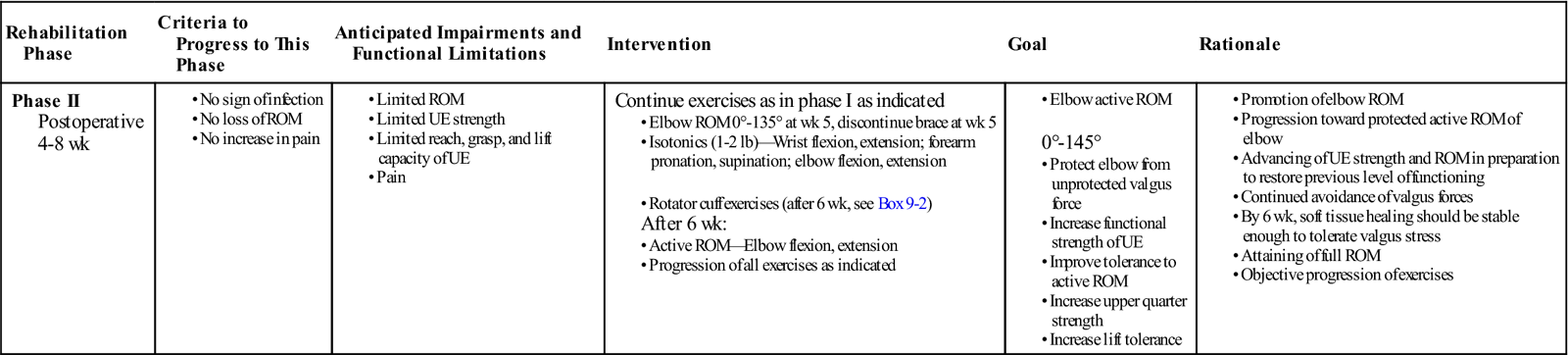
< ?comst1?>
< ?comen1?>
The intermediate phase begins approximately at week 4. Advancement through the rehabilitation process is adjusted based on the response of the patient to surgery, tissue healing constraints, and a criterion-based progression.
Light wrist and elbow isotonics can be initiated during week 4, as well as rotator cuff strengthening. The therapist should advance the resistance with isotonic exercises as the patient’s strength improves. Typically, the patient progresses by 1 lb per week.
Training the muscles in the way they are to perform with throwing is the focus. For example, the flexor carpi ulnaris and flexor digitorum superficialis muscles are located directly over the anterior band of the UCL and may contribute to dynamic stabilization of the medial elbow. Rhythmic stabilization drills in the throwing position assist in training these muscles in a similar manner. In addition, the elbow extensors act concentrically to accelerate the arm during the acceleration phase, whereas the elbow flexors act eccentrically to control the rapid rate of elbow extension during follow-through. Biasing the exercise selection appropriately for these muscle groups allows more effective strength training and provides neuromuscular training, allowing the muscles to function more efficiently when performing skilled movement patterns.
During this phase the therapist should pay careful attention to the patient’s ROM. One of the most common complications after UCL reconstruction is development of an elbow flexion contracture and joint stiffness. In addition, flexion contracture is common in overhead-throwing athletes. Throwing athletes have demonstrated a 7.9° average loss of elbow extension ROM before their competitive season.26 Therefore early intervention and progressive motion and stretching exercises are important preventatives against elbow flexion contracture (Box 9-1).27
ROM is gradually progressed to achieve 0° to 135° by week 5. At this time, the brace may be removed. The intimate configuration of the elbow joint is prone to develop contractures. In addition, scarring of the brachialis muscle to the capsule may further lead to loss of motion. ROM and stretching techniques are continued to ensure the prevention of motion complications. Additionally, low-load long-duration stretching may be incorporated as needed.
Phase III
TIME: 8 to 13 weeks after surgery
GOALS: Increase strength, power, and endurance, maintain full ROM, gradually add sports activities (Table 9-3)
TABLE 9-3
< ?comst?>
< ?comen?>< ?comst1?>
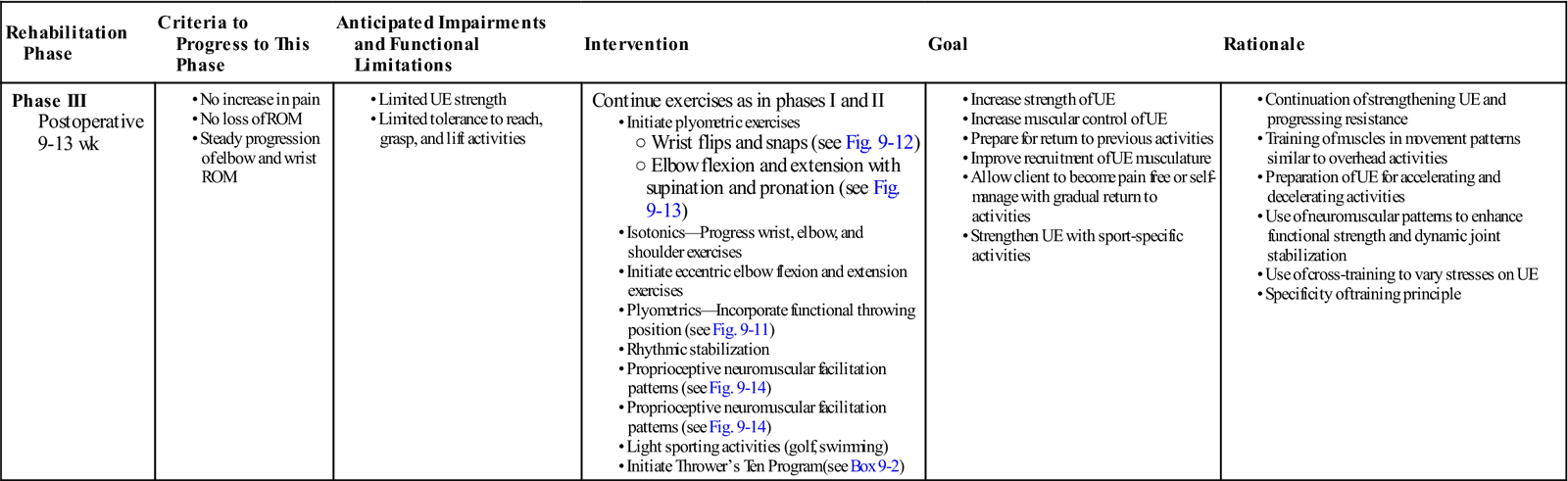
< ?comst1?>
< ?comen1?>
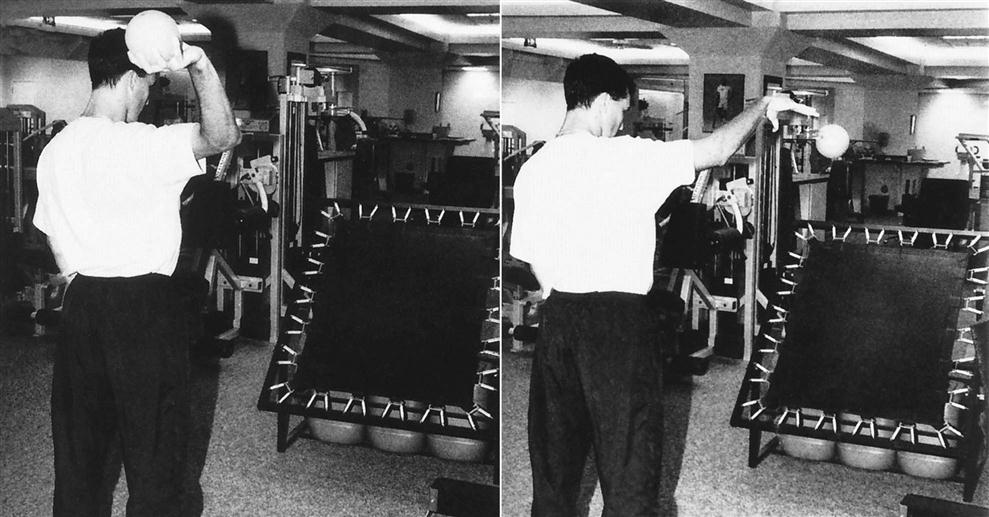
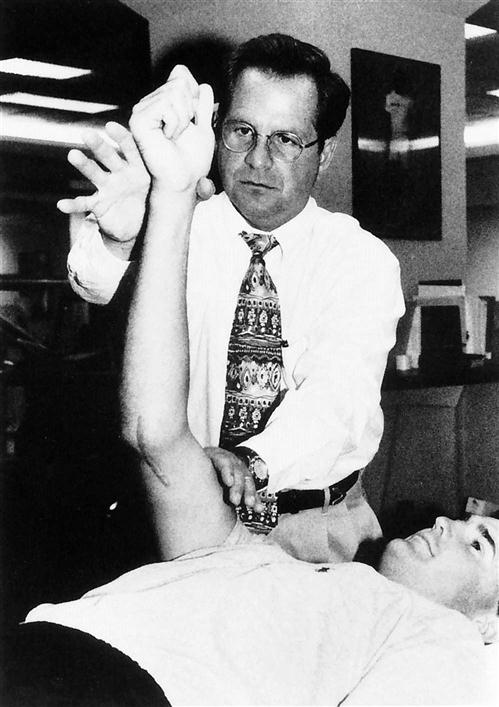
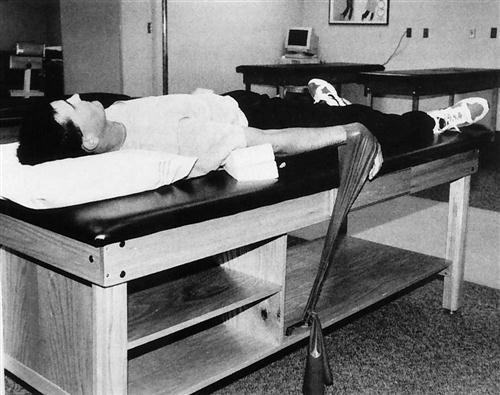
During this phase aggressive wrist, forearm, elbow, and shoulder strengthening are advanced with a Thrower’s Ten Program (Box 9-2). The patient may begin light plyometric exercise during this phase. Plyometrics are initiated with two-hand drills, close to the body, such as a chest pass. These exercises are progressed away from the body to include side-to-side and overhead throws and, finally, one-hand drills at week 12. These drills are used to develop power and explosiveness with weighted balls, often incorporating the functional throwing position (Fig. 9-11). Forearm plyometrics should also be introduced in this phase (Fig. 9-12). Exercises such as wrist flips and snaps will incorporate wrist flexors while extension grips will address wrist extension strength. Manual proprioceptive neuromuscular facilitation (PNF) drills integrate elbow flexion and extension with respective supination and pronation, helping to improve joint stability (Fig. 9-13). Emphasis should be placed on the concentric and eccentric roles of each muscle during the throwing motion. D2 flexion and extension PNF drills incorporate the shoulder, thus further encouraging strength and dynamic stabilization in functional movement patterns (Fig. 9-14). Rhythmic stabilization drills should also be incorporated in more functional throwing positions to establish control through the core stabilizers as well. Stability deficits throughout the kinetic chain will place added stress on the repaired UCL (Fig 9-15).
Phase IV
TIME: 14 to 26 weeks after surgery
GOALS: Increase strength, power, and endurance of upper extremity muscles, gradually return to sports activities (Table 9-4)
TABLE 9-4
< ?comst?>
| Rehabilitation Phase | Criteria to Progress to This Phase | Anticipated Impairments and Functional Limitations | Intervention | Goal | Rationale |
| Phase IV Postoperative 14-26 wk |
< ?comen?>< ?comst1?>
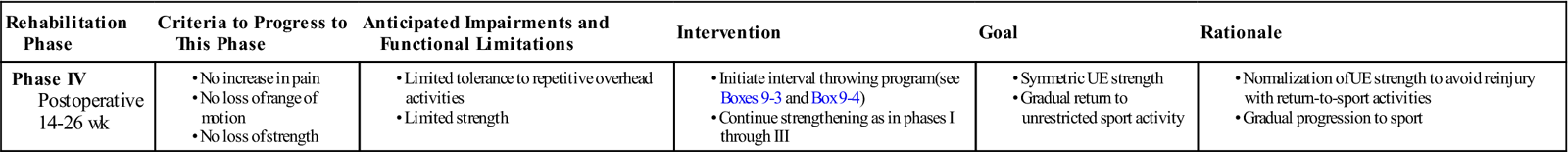
< ?comst1?>
< ?comen1?>
In this final phase, the physical therapist should take care to return the patient to sports activities gradually; an interval sports program may help ensure that goal (Boxes 9-3 and 9-4). Other throwing programs are described in Chapters 3 and 13. An interval throwing program may be initiated for an overhead thrower at 16 weeks after surgery, with throwing off the mound usually occurring around 5 to 6 months after surgery.27 Return to competition typically occurs between 9 and 12 months. The competitive overhead athlete should participate in a year-round conditioning program that consists of isotonic strengthening, plyometric and neuromuscular training, and a sport-specific training program. Wrist, elbow, and forearm strength should continue to improve. Professional throwing athletes have significantly greater forearm pronation and wrist flexion strength on the dominant arm.28 In addition, the athlete should continue flexibility exercises for the elbow, wrist, and hand. The interval throwing program emphasizes a proper warm-up, correct throwing mechanics, and a gradual progression of intensity. The therapist also must teach the athlete to “listen” to the arm: if pain is present, then the patient should not advance the program prematurely.
Suggested Home Maintenance For The Postsurgical Patient
The home maintenance box, as well as Box 9-2, reviews exercises that are commonly prescribed for the patient to perform at home. The exercises are progressed gradually to allow the tissue proper healing time, with the ultimate goal of full restoration of strength and ROM. The exercises are to be performed at home in conjunction with treatment sessions in the rehabilitation setting.
Troubleshooting
As already noted, the most common complication after UCL reconstruction is a flexion contracture or stiff joint. Factors that predispose the elbow joint to this loss of ROM include the following:
1 The intimate congruency of the elbow joint complex, especially the humeroulnar joint
2 The tightness of the elbow joint capsule
3 The tendency of the anterior capsule to scar and become adhesive29
Box 9-1 outlines a program found to be effective in combating flexion contractures of the elbow. It includes both passive and active warm-up, joint mobilizations, and manual stretching techniques. One of the most effective components to the stretching regimen is the low-load, long-duration stretching technique. The three most important components of this technique are (1) duration of stretch (10 to 15 minutes), (2) intensity of stretch (low to moderate), and (3) frequency of stretch (5 to 6 times daily) (Fig. 9-16).
This stretching technique may be enhanced by the use of other modalities such as moist hot packs or ultrasound. The rationale for the success of this technique is its ability to produce a plastic response within the collagen tissue, resulting in permanent elongation.7,30–32
If ROM complications persist, the therapist may want to prescribe a splint to be worn both day and night. A static splint holds the joint in a constant position, whereas a dynamic splint uses a spring to exert force and create a progressive stretch. Patients are encouraged to remove the splint daily for strengthening and stretching exercises.
During the aggressive stretching program the patient often experiences increased elbow soreness or pain. Pain control using cryotherapy, high-voltage galvanic stimulation (HVGS), transcutaneous electric nerve stimulation (TENS), and interferential current is highly effective.
Other complications include hand and grip weakness, ulnar neuropathy, rotator cuff tendonitis, and UCL failure. Intrinsic weakness of the hand may be avoided by initiating gripping exercises immediately after surgery and increasing intensity as rehabilitation progresses. Ulnar neuropathy generally develops immediately after surgery. Transposition of the ulnar nerve may cause sensory changes of the little finger and ulnar half of the ring finger. Motor deficits may include the inability to adduct the thumb, weakness of the finger abductor and adductors, adduction of the little finger, and weakness of the flexor carpi ulnaris. The most frequent patient complaint is paresthesia through the ulnar nerve sensory distribution, but this is usually transient and should resolve within 7 days.
Inactivity can lead to rapid deterioration of rotator cuff strength and a subsequent inability to stabilize the glenohumeral (GH) joint during the throwing motion. Integrating a Thrower’s Ten Program with the emphasis on rotator cuff strengthening several weeks before throwing greatly reduces the chances of developing tendonitis.
UCL failure is the most serious of all postoperative complications. Graft failure or poor bone quality with inadequate graft stabilization necessitates subsequent surgery or the cessation of overhead activities. Fortunately, with advanced surgical and rehabilitation techniques, successful outcomes are much more likely than failures. Andrews and Timmerman33 found 78% of professional baseball players returning to their previous level of play after UCL reconstruction. Additionally, Cain and associates34 found that 83% of overhead athletes returned to their previous level or higher upon 2-year follow-up. Major complications occurred with only 4%.
Clinical Case Review
1 The patient is a 16-year-old female tennis player who had UCL reconstruction 16 weeks ago. She has full ROM and has been progressing with her isotonic strengthening program. She expresses that she is ready to start playing. What types of intervention still need to be incorporated in her program before she can begin sporting activities, and what is the rationale for doing so?
Before any overhead sporting activity such as hitting a tennis ball, it is important that the patient has progressed through a proper rehabilitation program, including isotonics, dynamic stabilization drills, a plyometric program, and an interval sport program. These exercises are essential to enhancing functional strength and dynamic joint stability, as well as preparing the upper extremity for the acceleration and deceleration forces required of her sport-specific activity.
2 The patient is a college baseball pitcher that had UCL surgery with ulnar nerve transposition 7 weeks ago. He is now performing some light isotonic exercises. What two muscles should the therapist target to enhance the dynamic stabilization of the medial elbow during a throwing motion?
The focus should be on training the muscles in the way they are to perform during throwing. The flexor carpi ulnaris and the flexor digitorum superficialis muscles are located directly over the anterior band of the UCL and may contribute to dynamic stabilization of the medial elbow.
3 The patient is a 20-year-old male pitcher who had UCL reconstruction 6 weeks ago. He arrives from another clinic with a 15° flexion contracture. What course of action should the therapist take to address this ROM deficit immediately?
The patient is behind with his ROM. The elbow joint is prone to develop a flexion contracture as the result of the intimate joint congruency. In the instance of a flexion contracture, the therapist should introduce treatments designed to create a plastic response in the collagen tissue. These include a passive warm-up, followed by active warm-up, joint mobilizations (including distraction and posterior ulnar glides), low-load, long duration, as well as contract-relax and passive stretching.
4 A patient who had UCL surgery 16 weeks ago wants to begin throwing. Is this appropriate?
Provided the patient has full ROM, good strength, and is pain free, an interval throwing program is initiated at week 16. Each stage is to be performed twice, with a day of rest in between, before moving to the next stage. Should the patient report pain or excessive soreness, he or she should move back a stage and continue from there.
5 A patient who had UCL surgery 8 months ago is beginning to throw on the mound near full effort and begins to report medial elbow pain. What should the therapist do?
The therapist should tell the patient to step back to a partial effort for a week and treat the pain symptoms. If the patient continues to feel pain when progressing, then he or she may need to see a physician and potentially stop throwing to allow time to heal while continuing with exercises.
6 A patient had UCL surgery 3 days ago and has been unable to adduct his thumb, abduct or adduct his fingers, and has weakness in the flexor carpi ulnaris. He also reports numbness in the fifth digit. What is the assessment? Is this cause for concern?
These signs and symptoms are consistent with an ulnar neuropathy, which is common after ulnar nerve transposition. The therapist can check for tight-fitting wraps or ill-fitting braces, but typically these complications resolve within 7 days after surgery.
7 Patient is a 19-year-old hockey player who had UCL reconstruction following an acute UCL tear as a result of a fall and subsequent elbow dislocation. How might the acute mechanism of injury affect progression of this patient’s postoperative ROM?
Early postoperative PROM can be progressed more quickly following reconstruction of acute tears. Full PROM should be expected by week 5. Chronic tears will progress more gradually, attaining full PROM closer to postoperative weeks 6 through 8.
8 A 23-year-old pitcher is 6 weeks out of surgery following an acute UCL tear. He is having trouble achieving full extension. How aggressive should manual techniques be when trying to restore full ROM?
There are a few factors to consider when trying to determine if aggressive mobilization and stretching is indicated. Consider the end feel and what type of tissue is constraining the ROM. An empty end feel with pain or swelling should be a sign to use a more gradual, less aggressive approach. Yet, a hard, bony end feel should present as a situation where more aggressive mobilization techniques would be indicated.
9 A 32-year-old NFL quarterback is postoperative week 2 following UCL reconstruction with ulnar nerve transposition. His posterior splint has been removed and early elbow flexion/extension ROM has been initiated. Is forearm pronation/supination ROM permitted during this phase?
Pronation and supination of the forearm place no strain on the UCL graft. Therefore, PROM in these directions can be initiated during week 2. Pronation and supination isometrics also have no effect on the strain in the UCL, allowing for their addition during this phase. Initiate pronation/supination isotonics during week 4, as you would for the wrist and elbow.
10 A professional baseball pitcher has met all of the criteria to progress to phase IV of his rehabilitation and is ready to begin an interval throwing program. He is leaving our care to gradually return to sports activities with his team’s training staff. What are some important things to stress to the trainers during their progression through this phase?
It is important to advance through an interval throwing program step by step, including timely progression to throwing off the mound. The overhead athlete should also participate in a year round conditioning program that includes isotonic strengthening, and plyometric and neuromuscular training. Forearm and elbow strength should continue to increase to greater than the nondominant side. Professional throwing athletes have greater wrist flexion and forearm pronation strength on their dominant arm, as well as greater strength on elbow flexion and extension.
11 Following UCL reconstruction, a patient asks why a hamstring graft was used despite the presence of palmaris longus. Are there situations where hamstring grafts might be preferable to palmaris longus grafts?
This type of questioning should always be referred to the referring physician. However, generally speaking, use of the contralateral gracilis muscle may be indicated when there is boney involvement of the UCL. The presence of bone within the UCL represents a chronic ligamentous deficiency, which requires use of a larger graft. Data suggest use of the contralateral hamstring graft is reliable, reproducible, and may provide improved results with return to play.35