Reconstruction of the Nose
Introduction
During the last decade, reconstruction of the nose has reached a high level of sophistication with enhancement of aesthetic results.1–3 This has been achieved by emphasizing the necessity of replacing surgically ablated tissue with like tissue. Skin is replaced with skin that matches in color and texture as closely as possible. Cartilage and bone are replaced, and mucosa is used to replace any loss of the nasal lining. The concept of nasal aesthetic units has emerged with an emphasis on replacing the skin of an entire unit if the majority of the skin is missing. Another important concept that has led to enhancement in the results of restorative surgery has been the emphasis on the placement of incisions for local flaps along borders of aesthetic regions or units to maximize camouflage of scars. Whenever possible, local flaps are designed so that they are not transferred across the borders of aesthetic regions, particularly if the border has a concave topography. An example of such a border is the alar-facial sulcus, which represents a concave border between three aesthetic facial regions: the nose, the cheek, and the upper lip.4,5
Topographic Analysis
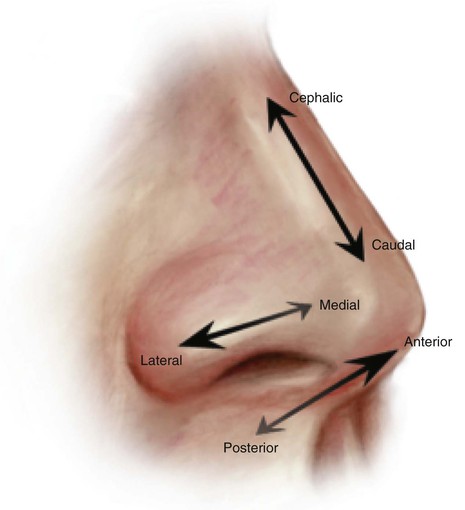
The aesthetic proportions of the ideal nasal shape and size have been established. On the lateral view, the distance from the vermilion border of the upper lip to the subnasale is equal to the distance from the subnasale to the pronasale.6 The distance from the alar-facial sulcus to the midpoint of the nares ideally equals that from the midpoint to the caudal edge of the nasal tip. On the lateral view, a right-angle triangle with the ratios of its sides being 3 : 4 : 5 and the vertices being at the nasion, alar-facial sulcus, and tip has been described to illustrate the ideal nasal proportions and size.7 Figure 18-1 illustrates the standard directional nomenclature.
Facial Aesthetic Regions
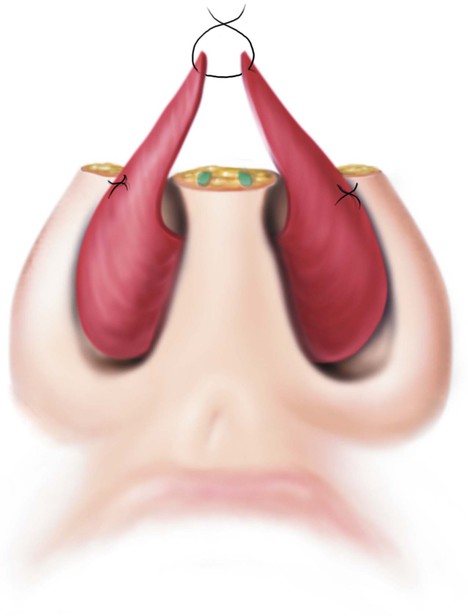
The face can be divided into topographic regions, each with its individual intrinsic characteristics of skin color, texture, contour, and hair growth.5 Each has an individual shape created by the underlying facial skeleton. The nose is one of the aesthetic regions of the face and may be divided into several aesthetic units (Fig. 18-2). Each unit may be proportionally overdeveloped or underdeveloped relative to other noses, but there is a consistent general configuration from nose to nose. There are nine aesthetic units of the nose identified by distinctive convex or concave surfaces, including the nasal tip (lobule), dorsum, paired sidewalls, paired alae, paired soft tissue facets, and columella. In general, the shape of the tip is determined by the size and contour of the alar cartilages and specifically by the domal portion of the nasal cartilages. It is covered by relatively thick skin containing many sebaceous glands (sebaceous skin). Each dome causes a point of reflected light. Above the tip is a supratip depression that separates the tip from the dorsum. The skin of the dorsum tends to be less thick and sebaceous than the skin of the tip, becoming progressively thinner as it ascends to the rhinion and thickening again as it approaches the glabella. The nasal bones together with the upper lateral cartilages and cartilaginous septum provide skeletal support for the dorsum. The lateral borders of the dorsum are defined by the lateral shoulders of the upper lateral cartilages and the junction of the nasal bones with the frontal processes of the maxillae. These structures separate the dorsum from the sidewalls and create a line of reflected light and shadows separating the lateral walls from the dorsum. The nasal sidewalls are most often a combination of convex and concave elements extending laterally from the dorsum to the junction of the nose with the cheek. Structurally, the sidewalls are supported by the lateral extensions of the nasal bones and upper lateral cartilages and the medial extension of the frontal processes of the maxillae. The skin of the sidewalls is thin and contains fewer sebaceous glands than that of the dorsum and tip; it is separated from the ala by the alar groove, which is the deepest contour line of the nose. This groove is continuous laterally with the alar-facial sulcus, and together they circle the alae, delineating them from the tip, sidewalls, and cheeks. The alar unit itself is a smooth bulge reflecting a single spot of light and is covered with thick skin similar in texture and porosity to the skin of the tip. The structural support of the ala is provided by thick fibrofatty tissue that does not contain cartilage.
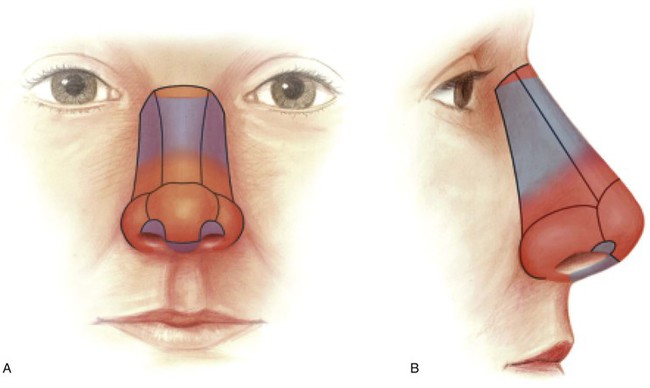
FIGURE 18-2 A, B, Aesthetic units of nose. Blue represents thin-skinned regions; red represents regions of thicker skin. (From Jewett BS: Anatomic considerations. In Baker SR, editor: Principles of nasal reconstruction, ed 2, New York, Springer, 2011.)
Menik has stressed that the goal of restorative nasal surgery is not simply to fill a defect.2 Depending on the extent of the defect, wounds should be altered in size, configuration, and depth to allow reconstruction of an entire unit. If the majority of the surface area of a unit is lost, resurfacing of the entire unit is usually preferable. This is accomplished by discarding the remaining skin of the unit and designing the covering flap so it will compensate for the discarded skin. This arrangement places scars at the junction between units, where they will lie in depressions or along shadow lines, maximizing scar camouflage. In these junctions, scars blend with normal contour lines of the nose and distract the viewing eye. Resurfacing of an entire aesthetic unit causes a mild trap-door scar contraction phenomenon, which in turn causes the entire unit to bulge slightly, simulating the normal convexity of the tip and alae.2 The columella, dorsum, and sidewalls are not convex, and I do not routinely resurface the entire surface of these aesthetic units when defects occupy more than half of their entire surface area.
An aesthetic nasal unit that is to be entirely resurfaced is covered with a flap that exactly duplicates its surface area and pattern whenever possible. A fresh wound is always enlarged by retraction of its margins; thus, the contralateral unit should be used to design covering flaps. If the contralateral counterpart is missing or a unit does not have a matching pair, a template replicating the ideal unit size for that specific patient is used. The nose is a three-dimensional structure and reconstruction of each unit must duplicate the normal contour. This is accomplished by concomitantly integrating structural support in each step of the repair. Reconstructed skeletal elements are attached to a stable foundation, such as remaining nasal cartilages or the bone of the maxilla, to prevent collapse or distortion of the unit during the healing process.2 Within the defect, the constructed skeletal structures are designed to completely span the defect. This is accomplished before wound healing to prevent distortion from scar contraction during the healing process.
Lining Flaps
The vascular supply to the internal nose is shown in Figure 18-3. On the basis of the vascular anatomy, Burget and Menik have demonstrated that the entire ipsilateral septal mucoperichondrium can be transferred with a narrow pedicle containing the septal branch of the superior labial artery.1 Likewise, the entire contralateral mucoperichondrium can be turned laterally as a dorsally based hinge flap based on the anterior and posterior ethmoid arteries to line the sidewall of the nose.1 Burget and Menik have also shown that if both right and left septal branches are included in the pedicle, the entire septum can be rotated out of the nasal passage as a composite flap containing a sandwich of cartilage between the two mucoperichondrial leaves.1 Such flaps, whether they are composite or simple mucoperichondrial hinge flaps, can be designed to extend from the floor of the nose to within 1 cm of the junction of the upper lateral cartilage and cartilaginous septum. The flaps may extend posteriorly well beyond the bone-cartilage junction of the septum, producing a hinged mucosal flap measuring as much as 3 cm wide and 5 cm long.1 Burget and Menik advocate a back cut of the mucosa in the area of the anterior septal angle to facilitate flap transfer.3 I prefer to leave the flap hinged on the entire length of caudal septum to maintain a wider pedicle and to enhance the vascularity of the flap. These authors have also described a bipedicle flap of vestibular skin and mucosa based medially on the septum and laterally on the floor of the nasal vestibule. Such a flap may be elevated away from the undersurface of the lateral crus and mobilized inferiorly to reline alar defects. All of these lining flaps have a reliable vascularity and are thin and supple, providing natural physiologic material for the interior of the nasal passage.
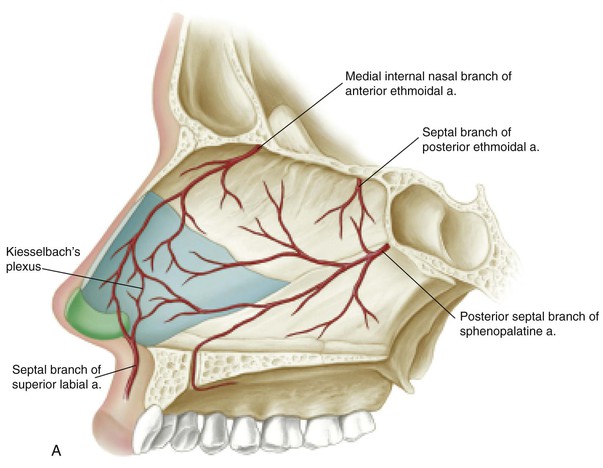
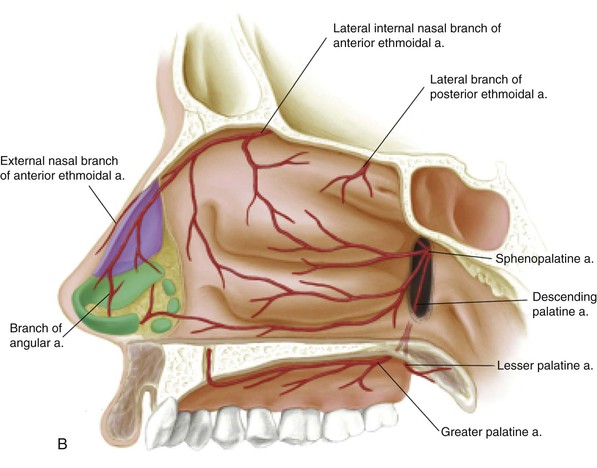
FIGURE 18-3 Arterial blood supply of left septum (A) and right lateral wall (B) of nasal cavity. (From Jewett BS: Anatomic considerations. In Baker SR, editor: Principles of nasal reconstruction, ed 2, New York, Springer, 2011.)
Bipedicle Vestibular Skin Advancement Flap
Lining for full-thickness alar or unilateral tip defects that have a vertical dimension (caudal to cephalic) of 1.0 cm or less can be provided by the thin skin of the remaining nasal vestibule. Defects with vertical dimensions as large as 1.5 cm may sometimes be lined by this method if the remaining skin of the lower nasal vault is of sufficient size. Before the bipedicle flap is created, the vertical height of the remaining vestibular skin is measured to ensure that there will be sufficient width for the flap to cover the lining defect. An extended intercartilaginous incision is made between the lateral crus and caudal aspect of the upper lateral cartilage. The incision extends from the anterior septal angle to the most lateral aspect of the floor of the vestibule. The remaining vestibular skin is then mobilized caudally in the form of a bipedicle advancement flap by elevating it away from the overlying lateral crus (Fig. 18-4).8 Dissection of the flap is assisted by hydrodissection, accomplished by infiltrating the subdermal plane with an anesthetic solution of lidocaine containing epinephrine. Mobilization is continued until the caudal border of the flap can be easily positioned without tension 1- to 2-mm below the caudal margin of the lining defect. To accomplish this, it is occasionally necessary to extend the intercartilaginous incision inferomedially from the anterior septal angle toward the membranous septum.
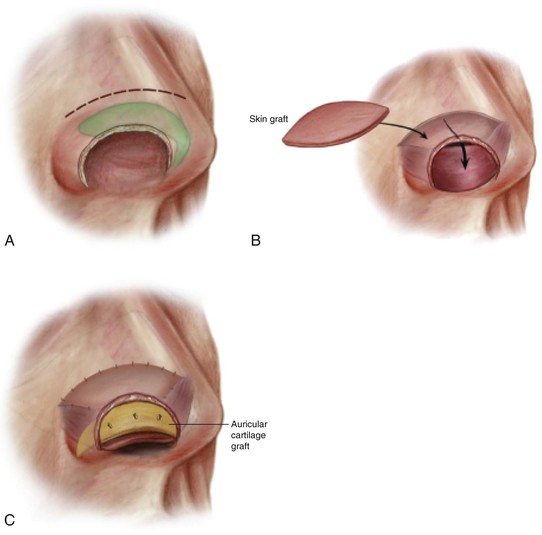
FIGURE 18-4 A, Bipedicle vestibular skin advancement flap created by making an intercartilaginous incision between upper and lower lateral cartilages. B, Flap mobilized sufficiently to allow caudal border to reach nostril margin. Thin full-thickness skin graft used to repair flap donor site. C, Auricular cartilage graft provides framework for nostril margin. Lining flap secured to cartilage graft with mattress sutures. (From Baker SR: Internal lining. In Baker SR, editor: Principles of nasal reconstruction, ed 2, New York, Springer, 2011.)
The bipedicle vestibular skin advancement flap consists only of skin. The overlying alar cartilage and fibrofatty tissue of the ala are left intact. As the flap is advanced caudally, redundancy occurs near the caudal aspects of the medial and lateral pedicles. This represents the standing cutaneous deformities that form with all advancement flaps. The tissue redundancy should not be trimmed because it will dissipate during wound healing. In the case of full-thickness defects that extend through the margin of the nostril, the flap is positioned so that the caudal border extends 1- to 1.5-mm below the inferior aspect of the framework used to reinforce the nostril margin. This enables the inferior border of the covering flap to be sutured to the vestibular skin flap, restoring the delicate nostril margin. When the lining defect does not extend through the nostril margin, the caudal border of the flap is sutured to the caudal border of the lining defect. Structural support for the flap is provided by septal or auricular cartilage grafts. The flap is suspended to the overlying cartilage grafts with 5-0 polydioxanone sutures (see Fig. 18-4). The sutures pass from the external surface of the cartilage graft, through cartilage and flap, and back through the flap and overlying cartilage. Three or four loosely tied sutures are usually required to support the flap and to suspend it completely to the framework. The number of sutures is limited to minimize risk of vascular impairment of the flap. The donor site of the flap is repaired with a thin full-thickness skin graft. If an interpolated cheek flap is used for covering, the standing cutaneous deformity that forms along the inferior aspect of the medial cheek during primary closure of the cheek donor site becomes the source of the skin graft.
Ipsilateral Septal Mucoperichondrial Hinge Flap
In general, the septal mucoperichondrial hinge flap should be designed as large as possible. Large flaps measuring 4.0 to 4.5 cm in length and 2.5 to 3.0 cm in width can provide sufficient mucoperichondrium to line the entire lower nasal vault and limited portions of the caudal aspect of the middle vault. A solution of lidocaine containing epinephrine is infiltrated in the subperichondrial plane along the entire length of the septum. Two horizontal incisions extending from anterior to posterior are made with a scalpel on an extended handle (Fig. 18-5). The dorsal incision begins 0.75 cm posterior to the anterior septal angle and extends along a line 0.5 to 1.0 cm below the roof of the middle vault. It should extend 1 to 2 cm posterior to the bone-cartilage junction of the septum. The inferior incision starts 1.0 cm posterior to the anterior nasal spine and usually extends along the junction of the nasal crest and the floor of the nose. The incision should extend as far posteriorly as the dorsal incision. A posterior vertical incision is then made between the ends of the dorsal and inferior septal incisions. This is accomplished with a right-angled scalpel. A No. 66 Beaver eye blade is useful for this purpose.
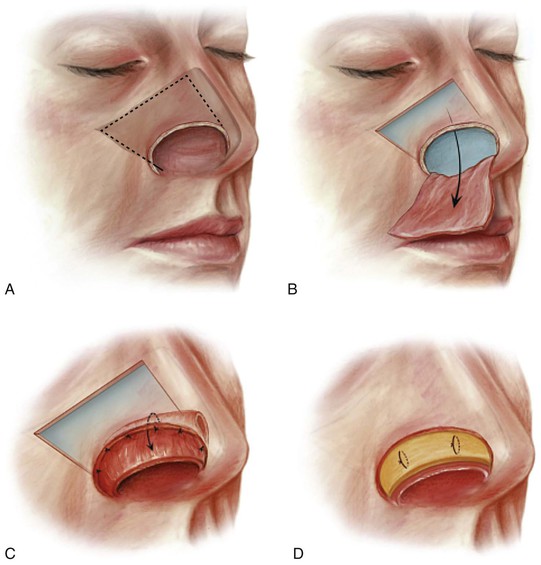
FIGURE 18-5 A, Unipedicle septal mucoperichondrial hinge flap developed by incising through mucosa and perichondrium along floor of nose and 1.5 cm below and parallel to cartilaginous dorsum. Incisions extend posteriorly beyond septal bony cartilaginous junction. B, Flap dissected from superior to inferior and anterior to posterior. Anterior dissection remains 1 cm posterior to caudal border of septum and 1.5 cm posterior to nasal spine. Flap based on intact mucoperichondrium of caudal septum and septal branch of superior labial artery. C, Hinged on caudal septum, flap is reflected laterally to line lower nasal vault. D, Cartilage graft provides nasal framework. Lining flap secured to framework with mattress sutures. (From Baker SR: Internal lining. In Baker SR, editor: Principles of nasal reconstruction, ed 2, New York, Springer, 2011.)
Bilateral Caudally Based Septal Mucoperichondrial Hinge Flaps
A septal mucoperichondrial hinge flap based on the caudal septum may be developed bilaterally (Fig. 18-6). Concurrent bilateral flaps preclude the use of a dorsally based septal mucoperichondrial hinge flap for repair of more cephalically located lining deficits. Bilateral flaps are indicated when a full-thickness defect of the entire nasal tip is present but with an intact columella. In this situation, each flap provides lining for the ipsilateral hemi-tip and any portions of the adjacent ala that may be absent. The flaps are designed, incised, and dissected in a fashion identical to the methods for a unilateral flap. The exposed septal cartilage is removed, leaving a permanent septal perforation as bilateral resurfacing of the cartilage by secondary intention healing is unlikely. A 1.5-cm-wide dorsal and caudal strut of septal cartilage is maintained for proper support of the nasal bridge. Each flap is turned laterally and anteriorly in a hinged fashion with the raw surface of the mucoperichondrium turned outward. The flaps are sutured to their respective lining defects and suspended to a framework of cartilage grafts used to restore the structure and topography of the nasal tip and any portions of the alae that may be missing.
Contralateral Dorsal Septal Mucoperichondrial Hinge Flap
A mucoperichondrium hinge flap harvested from the side opposite the nasal defect and based on the nasal dorsum may be turned laterally to resurface the roof and lateral wall of the middle vault of the nose (Fig. 18-7).8 The flap may be designed to include all of the mucosa covering the cartilaginous septum, except for the mandatory maintenance of the caudal and dorsal strut of the septum. Similar to the mucoperichondrial flap hinged on the caudal septum, the elevation is facilitated by hydrodissection with a solution of local anesthetic injected beneath the perichondrium. Anterior and posterior vertical incisions are made with a right-angled scalpel. Incisions extend from the floor of the nose to within 1 cm of the nasal dorsum. The incisions are separated by the distance appropriate for the desired width of the flap. The mucoperichondrium is dissected with a Freer elevator as a bipedicle flap attached to the dorsum above and the floor of the nose below. Once the mucoperichondrium has been completely freed from the septal cartilage, it is released from the floor with a scalpel blade attached to an extended handle. The exposed septal cartilage is removed for grafting purposes (Fig. 18-8), leaving adequate dorsal support for the nasal bridge. The flap is reflected laterally across the midline toward the side of the lining defect while maintaining its attachment to the contralateral nasal dorsum. This maneuver turns the raw undersurface of the mucoperichondrium outward, away from the nasal passage. This flap is most commonly combined with an ipsilateral mucoperichondrial flap hinged on the caudal septum. The dorsally based flap passes through the large septal perforation necessitated by the use of the two flaps. The caudal border of the dorsally based flap is sutured to the undersurface of the hinge ipsilateral flap (see Fig. 18-7C). This maneuver seals off the nasal passage from the exterior portion of the nasal defect. A continuous carpet of mucoperichondrium can then be used to nourish an overlying cartilage framework. The flaps are suspended to the framework with mattress sutures so there is intimate contact between the mucoperichondrium and the entire undersurface of the cartilage grafts used for framework.
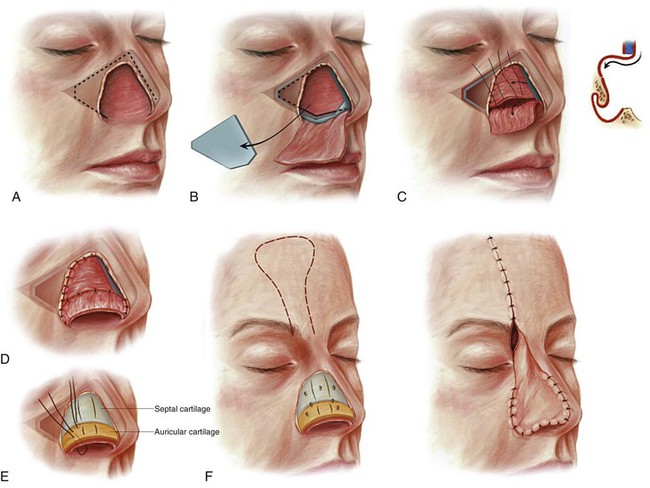
FIGURE 18-7 A, Broken line indicates incision for ipsilateral septal mucoperichondrial flap. B, Flap reflected outward and exposed septal cartilage removed. Broken and solid lines indicate incisions used to create contralateral dorsal septal mucoperichondrial hinge flap. C, Dorsally based flap reflected laterally and sutured to borders of middle vault lining defect. Caudal border of flap sutured to raw surface of ipsilateral flap to seal nasal passage from exterior. D, Caudally based hinge flap provides lining for lower nasal vault; contralateral dorsally based hinge flap provides lining for middle and upper nasal vaults. E, Septal cartilage (blue) provides framework for middle nasal vault; auricular cartilage (yellow) provides framework for lower nasal vault. Cartilage grafts scored to create desired convex contour. Lining flaps attached to framework with mattress sutures. F, Nasal framework covered by paramedian forehead flap. (From Baker SR: Internal lining. In Baker SR, editor: Principles of nasal reconstruction, ed 2, New York, Springer, 2011.)



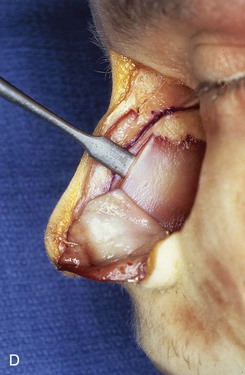
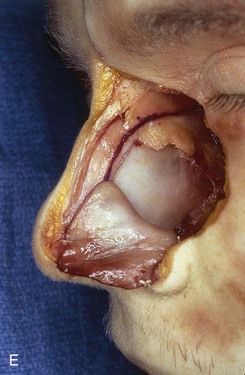




FIGURE 18-8 A, Outline of ipsilateral mucoperichondrial hinge flap. Dorsal incision is parallel and 1 cm below attachment of upper lateral cartilage to nasal septum. Inferior incision extends along junction of nasal crest with cartilaginous septum. B, Flap is elevated in subperichondrial plane from anterior to posterior. C, Mucoperichondrium based on caudal septum is reflected laterally as hinge flap. D, Exposed septal cartilage is freed from contralateral mucoperichondrium. L-shaped strip of septal cartilage 1 to 1.5 cm wide is preserved dorsally and caudally to support middle and lower nasal vaults. E, Septal cartilage removed for grafting purposes. Contralateral mucoperichondrium remains intact. Exposed bony septum may be removed or left in place. F, Contralateral dorsal septal mucoperichondrial hinge flap outlined. The majority of contralateral mucoperichondrium is incorporated in flap. Flap is created by two vertical and one inferior horizontally oriented incisions. G, Flap incised and reflected laterally. H, Flaps sutured in position. Caudal edge of contralateral flap is tacked to exposed raw submucosal surface of ipsilateral flap to seal off nasal passage from exterior. I, Ipsilateral flap is reflected laterally to line lower nasal vault. Suture suspension of flap to overlying cartilaginous framework (not yet in place) restores arc of nasal vestibule. (From Baker SR: Intranasal flaps. In Baker SR, editor: Principles of nasal reconstruction, ed 2, New York, Springer, 2011.)
Septal Composite Chondromucosal Pivotal Flap for the Tip and Columella
When the columella and nasal tip are both missing, a septal composite chondromucosal pivotal flap provides the cartilage necessary for the framework of the columella and the concomitant lining to resurface the area of the membranous septum and nasal domes (Fig. 18-9). The flap is designed with the maximum width possible while still preserving an adequate dorsal septal strut. The flap is extended the entire length of the cartilaginous septum and usually includes portions of the bony septum. Typically, the flap is 3 cm wide and 5 cm long. Bilateral mucoperichondrial flaps are created with a periosteal elevator along the anterior floor of the nose adjacent to the nasal spine. Access to this dissection is through the anteroinferior margin of the defect near the nasal spine. The dissection is extended superiorly over the lateral aspect of the nasal crest until the septal cartilage is encountered.
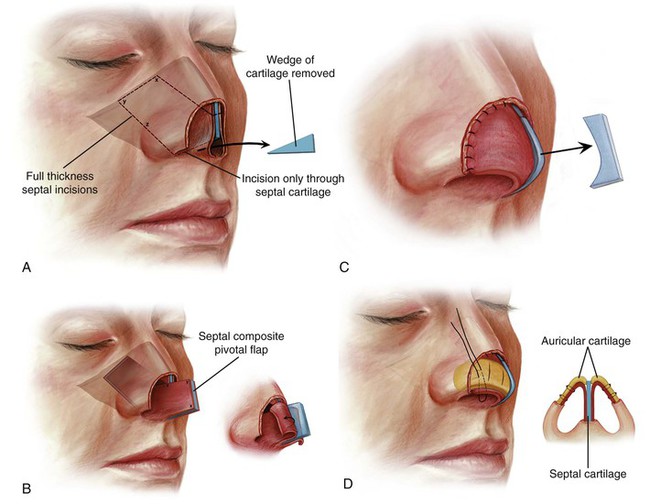
FIGURE 18-9 A, Bold broken line indicates full-thickness incision through septal cartilage, bone, and bilateral mucosa to create composite septal chondromucosal pivotal flap. Faint broken line indicates incision made only through septal cartilage, preserving overlying mucoperichondrium. Wedge of cartilage removed to enable flap to pivot anterocaudally. B, Cephalic aspect of pivotal flap locked into place by abutting it against remaining cartilaginous dorsum. Bilateral mucoperichondrial flaps reflected laterally to provide lining for nasal tip. C, Excess septal cartilage trimmed. Reflected mucoperichondrial flaps sutured to borders of lining defect. D, Auricular cartilage graft (yellow) provides bilateral framework for nasal tip, replacing missing lateral crura. Septal cartilage (blue) of composite flap serves as medial crura for reconstruction. Mucoperichondrial flaps attached to framework with mattress sutures. (From Baker SR: Internal lining. In Baker SR, editor: Principles of nasal reconstruction, ed 2, New York, Springer, 2011.)
A 4-mm-wide osteotome is used to excise a 2-cm-long segment of anterior nasal crest at the pivotal point of the flap while preserving the anterior septal spine. A No. 11 scalpel blade is used to make a full-thickness incision through the cartilaginous septum parallel to and 1.0 cm below the attachments of the upper lateral cartilages to the septum. The incision extends in an anterior direction from the bony perpendicular plate through the exposed margin of the caudal septum. A similar full-thickness incision is made with the same blade along the interface of the cartilaginous septum and the nasal crest, extending anteriorly from the vomer until it is juxtaposed to the previously resected nasal crest. The incision should remain 1.5 cm posterior to the anterior nasal spine to ensure a sufficient vascular pedicle. The pedicle is represented by bilateral mucoperichondrial flaps that are in continuity with the floor of the nose anteriorly and nourished by septal branches of the superior labial arteries.1 A posterior vertical incision is then made to connect the two previously performed parallel horizontal incisions. If the flap extends only to the bone-cartilage junction, the incision is made with a right-angled scalpel; however, it is usually necessary to include bony septum in the flap to achieve adequate flap length. In these instances, the horizontal incisions are extended posteriorly full thickness through the bony septum and the covering mucosa on either side with heavy-duty angled turbinectomy or bone-cutting scissors. It is important to ensure that the superior horizontal incision of the bony septum is completed before an osteotome is used to make the vertical incision through the bony septum so that the force of the osteotome is not transmitted to the region of the cribriform plate.
Once the septal incisions are completed, the composite flap is pivoted 90° on its base in an anterocaudal direction until the inferior border of the flap locks in place, bracing it against the remaining dorsal septal strut (see Fig. 18-9).9 After the flap is positioned, bilateral septal mucoperichondrial hinge flaps are dissected from the distal portion of the flap’s bone and cartilage. The flaps are reflected laterally to provide lining to the nasal domes. Denuded cartilage and bone extending beyond the planned dorsal line are resected and used for framework grafts. The borders of the reflected mucoperichondrial flaps are sutured to the margins of the lining defect. A framework of cartilage grafts is created from septal and auricular cartilage to replace the missing portions of the dome complex and lateral crura. The cartilage remaining within the composite flap serves as the medial crura for the construction and provides support to the columella. It also serves as the foundation for the framework grafts used for the nasal domes. These grafts are sutured directly to the cartilage of the composite flap and are then scored and bent in a fashion to restore the contour of the domes. The mucoperichondrial flaps reflected laterally from the composite chondromucosal flap are approximated to the overlying framework grafts with sutures placed through the framework cartilage and underlying flaps. Some of the cartilage of the caudal aspect of the composite flap may require trimming if it causes excessive caudal positioning of the reconstructed columella.
Septal Composite Chondromucosal Pivotal Flap for Dorsum
There are occasions when a patient presents with an intact nasal tip but has a full-thickness dorsal defect involving loss of cartilaginous dorsum and nasal bones. In these circumstances, the remaining septum may be used as a composite chondromucosal pivotal flap to provide a mucosal lining and structural support for the roof of the middle and upper nasal vaults (Fig. 18-10). The anterior septal angle is usually missing along with the upper lateral cartilages, and the composite flap is used to resurface the interior of the entire dorsal defect. The flap is harvested in a manner similar to that described for the pivotal flap used to reconstruct full-thickness defects of the tip and columella. The flap pivots only 45°, compared with 90° for repair of the tip and columella, so it is not necessary to remove the anterior nasal crest bone. Working through an endonasal approach as well as through the dorsal defect, a full-thickness horizontal incision is made through the septum along the length of the nasal crest. The anterior extent of this incision remains 1.5 cm posterior to the anterior nasal spine. The length of the incision depends on the defect but usually extends 2 to 3 cm posteriorly through the bony septum. This is usually necessary to ensure sufficient length to enable the flap to engage the frontal bone or remaining nasal bones once it is pivoted into position. A vertical incision is extended from the posterior end of the horizontal incision along the floor of the nose. This septal incision extends upward to join the most cephalic aspect of the bony or cartilaginous septum exposed by the defect. The flap is delivered from the nasal passage by manually pivoting the flap 45° on its pedicle. It may be necessary to remove cartilage in the area of the posterior septal angle to pivot the flap. This should be performed so that the adjacent mucoperichondrium is not damaged; this tissue represents the pedicle for the flap.
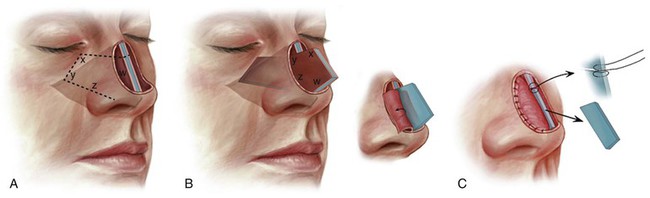
FIGURE 18-10 A, Broken line indicates full-thickness incision through septal cartilage, bone, and bilateral mucosa to create composite septal chondromucosal pivotal flap. B, Cephalic aspect of pivoted flap locked into place by abutting it against remaining nasal bony septum. Bilateral mucoperichondrial flaps reflected laterally to provide lining to nasal passage. C, Excess septal cartilage and bone trimmed and mucoperichondrial flaps sutured to borders of lining defect. Figure-of-eight suture fixes composite flap to remaining nasal bony septum. (From Baker SR: Internal lining. In Baker SR, editor: Principles of nasal reconstruction, ed 2, New York, Springer, 2011.)
Septal Composite Chondromucosal Pivotal Flap for the Tip, Columella, and Dorsum
Total and near-total nasal reconstruction may use the septum for internal lining if sufficient septum remains. This requires incorporation of the entire remaining nasal septum in the composite flap (Fig. 18-11). These cases are frequently associated with resection of the caudal cartilaginous septum and loss of the septal branches of the superior labial artery. In these circumstances, the flap is based on the mucoperiosteum of the anterior floor of the nose, and delay of the flap is necessary. Three stages are used to line the nose.
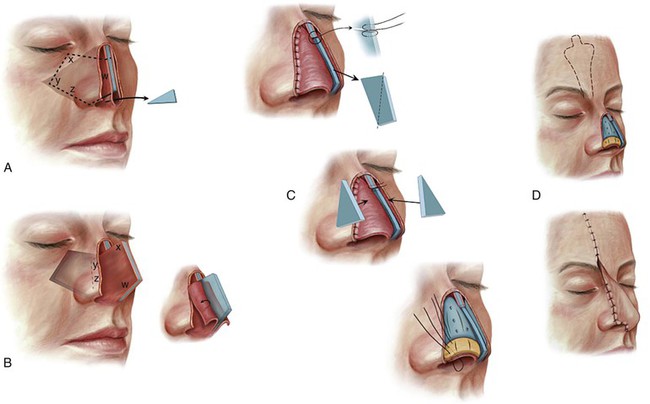
FIGURE 18-11 A, Bold broken line indicates full-thickness incision through septal cartilage, bone, and bilateral mucosa. Solid bold line indicates incision only through septal cartilage, preserving mucoperichondrium. Wedge of cartilage removed to enable flap to pivot anterocaudally. B, Cephalic aspect of pivoted flap locked into place by abutting it against nasal process of frontal bone. Bilateral mucoperichondrial flaps reflected laterally to provide lining to nasal passages. C, Excess septal cartilage and bone trimmed and mucoperichondrial flaps sutured to borders of lining defect. Figure-of-eight suture stabilizes composite flap to nasal process. Septal cartilage (blue) and auricular cartilage (yellow) provide nasal framework. Cartilage grafts scored to create desired convex contour. Mucoperichondrial flaps attached to framework with mattress sutures. D, Nasal framework covered by paramedian forehead flap. (From Baker SR: Internal lining. In Baker SR, editor: Principles of nasal reconstruction, ed 2, New York, Springer, 2011.)
Stage one consists of making the previously described inferior horizontal incision along the floor of the nose and vertical incision through the mucosa on either side of the septum but not through the bone and cartilage. Stage two is completed 3 weeks later by making incisions through the cartilage and bone of the septum, following the previous incision lines made in the covering mucosa. The composite flap is delivered from the nasal passage and is pivoted 90° to provide the maximum amount of mucosa for construction of the lining of the caudal portion of the nose. If the cephalic portion of the dorsum is missing, there will not be a buttress on which to stabilize the pivoted flap. In this case, nasal packing is used to stabilize the flap. Packing is left in place for 5 days. The flap is left protruding from the nasal passage for 4 to 6 weeks before proceeding with reconstruction of the nasal lining. Stage three consists of creating bilateral mucoperichondrial flaps based on the anteroinferior border of the mobilized composite flap. The flaps are reflected laterally to line the roof and sidewalls of the caudal nose. If the flaps are lacking sufficient tissue to line the cephalic portions of the nasal passage, local turn-in flaps or a paramedian forehead flap is used as lining for this portion of the nose. The reflected mucoperichondrial flaps are supported by an overlying framework of cartilage and bone that is covered by a paramedian forehead flap.
Turbinate Mucoperiosteal Flap
The middle and inferior turbinates may be used to line limited mucosal defects of the nose.10 These turbinates are richly supplied by a vascular network arising from a lateral descending branch of the sphenopalatine artery. The main supply to the inferior turbinate from this artery enters 1.0 to 1.5 cm from its posterior border and passes forward, giving off an anastomotic network of vessels. The artery also has anastomotic connections with the anterior blood supply of the turbinate. The anterior blood supply originates from the angular artery and is sufficient to allow the entire turbinate to be pedicled on this source.11,12
Middle and inferior turbinate flaps are harvested by a similar technique (Fig. 18-12). A local anesthetic solution containing a concentration of epinephrine of 1 : 100,000 is infiltrated along the turbinate, floor of the nose, and middle or inferior meatus, depending on which turbinate is used. The turbinate is medialized with a blunt elevator or the handle of a scalpel to open the meatus below the turbinate. A Cottle elevator or a 2-mm osteotome is placed in the meatus below the turbinate and pushed superiorly to perforate the bony attachment to the lateral nasal wall. Multiple perforations of the bone are made along the length of the turbinate, starting 1 cm posterior to the anterior end of the turbinate. The cutting instrument is maintained in a vertical plane against the lateral nasal wall to maximize the amount of tissue obtained without penetrating the paranasal sinuses. Pedicled anteriorly, the posterior aspect of the mobilized turbinate is pivoted toward the nasal defect with Takahashi forceps. The bone of the delivered turbinate is removed, leaving a mucosal flap that is transferred to the recipient site and sutured in position. If the location of the lining defect is the nasal tip, the pedicle of the flap will, by necessity, span the nasal passage and partially obstruct the airway. In this case, detachment of the pedicle is accomplished under local anesthesia 3 weeks later.
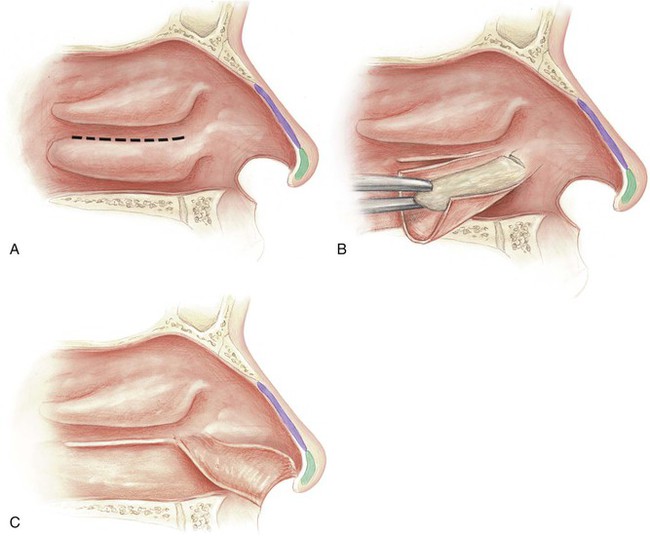
FIGURE 18-12 A, Inferior turbinate released from bony attachment to lateral nasal wall (dotted line). B, Mucoperiosteum dissected from underlying concha bone and unfurled. Bone removed. C, Pedicled anteriorly, inferior turbinate mucoperiosteal flap is usually sufficient to line entire ala. (From Baker SR: Intranasal flaps. In Baker SR, editor: Principles of nasal reconstruction, ed 2, New York, Springer, 2011.)
Framework
The tip is shaped by the alar cartilages, and the preferred replacement framework is conchal cartilage grafts. By coincidence, when it is turned upside down, the contralateral conchal cymba often closely resembles the shape of the dome cartilage (intermediate crus), and the conchal cavum resembles the shape of the lateral crus (Fig. 18-13). A graft 5 to 8 mm wide from the auricle can be used to replace the entire lower lateral cartilage. Such grafts may be used bilaterally or unilaterally as required and are fixed to any residual stumps of the medial and lateral crura. They support the dome and re-create the contour of the nasal tip.

FIGURE 18-13 When it is turned upside down, contralateral conchal cymba (above) resembles shape and contour of lower lateral cartilage (below).
An alar batten of septal or conchal cartilage 5 mm wide is used for the framework of the ala and nasal facet. The natural curvature of the conchal cartilage makes this material preferable to septal cartilage when it is available (Fig. 18-14). When a portion or all of the lateral crus is missing in addition to the ala, a separate conchal cartilage graft may be used to replace the missing crus. Alternatively, a single piece of ear cartilage may be used for both. In such circumstances, the graft is designed wider (0.75 to 1.0 cm) to replace the lateral crus and to provide support to the ala concomitantly. The graft is placed along the proposed margin of the missing nostril from the alar base to the nostril apex. It is inserted into a deep tissue pocket in the alar-facial sulcus and is attached medially to the framework of the dome (Fig. 18-15). The tissue pocket serves to stabilize the graft laterally. Similar to the grafts used to replace missing alar cartilage, grafts must be thinned, scored, and bent to replicate the bulging contour of the ala. If the nasal defect extends into the soft tissue facet, the cartilage graft is extended beneath the diverging angles of the intermediate and lateral crura to span any gap present. The graft fixes the reconstructed nostril rim in position, preventing upward migration and notching of the rim.
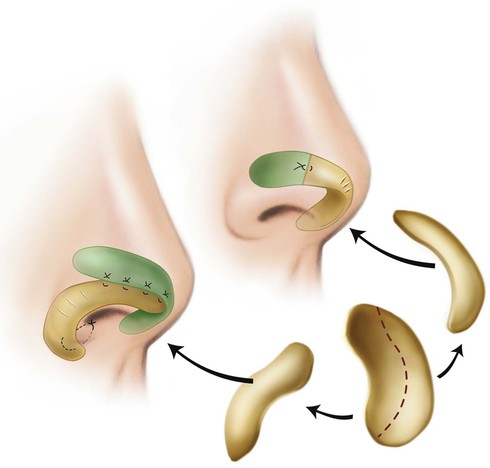
FIGURE 18-14 Auricular cartilage grafts used to replace missing segments of alar cartilage and to support ala. (From Naficy S: Structural support. In Baker SR, editor: Principles of nasal reconstruction, ed 2, New York, Springer, 2011.)
Covering Flaps
Nasal Cutaneous Flaps
Primary wound closure is possible for smaller skin defects of the nose, especially in the elderly patient, in whom nasal skin tends to be redundant, or when defects are very small relative to the size of the nose (Fig. 18-16). Defects that are 1.0 cm or smaller and located on the dorsum or sidewall are repaired most easily. This is accomplished by advancement of opposing wound margins after wide undermining of the skin adjacent to the defect. Standing cutaneous deformities form at the margins of the repair and usually require excision (Fig. 18-17). Primary wound closure of defects of the tip and supratip area frequently distorts the free margins of the nostril. Fortunately, alar cartilages typically have sufficient intrinsic strength to counteract this distortion; over time, the nostril margin usually returns to its natural position.

FIGURE 18-16 A, A 1.2 × 1.1-cm skin defect of nasal tip. Primary wound closure planned. Anticipated standing cutaneous deformities marked by horizontal lines. B, C, Deformities excised and wound closed. D, Postoperative view at 7 months. Scar dermabraded 3 months postoperatively.

FIGURE 18-17 A, A 1 × 0.8-cm skin defect of dorsum. Primary wound closure planned. Anticipated standing cutaneous deformities marked. B, Deformities excised. Wound closed. C, Postoperative view at 9 months. Scar dermabraded.
When primary wound closure is not possible, cutaneous flaps harvested from the nasal skin may be an alternative for repair of centrally located nasal skin defects that measure up to 2.5 cm in greatest dimension. Nasal cutaneous flaps are particularly useful for elderly patients because their skin is lax and mobile. When they are designed properly, flaps harvested from nasal skin have the advantage of color, texture, and thickness similar to those of the missing skin of the defect. Nasal cutaneous flaps are not sufficient to resurface an entire aesthetic unit of the nose, and the scars resulting from flap transfer do not always fall in the borders between aesthetic units. However, the ultimate contour of the nasal repair is far more important aesthetically than the location or number of scars.
Transposition Flaps
Transposition flaps are pivotal flaps with a linear axis. The base of the flap is positioned adjacent to the defect, and the donor site is repaired primarily by advancement of surrounding nasal skin. The use of transposition flaps is restricted to repair of defects 1.0 cm or smaller in the thin skin zones of the nose (Fig. 18-18). Flaps confined within thick skin zones work poorly unless the defect is small (0.5 cm or smaller in maximum dimension). The thicker skin of the caudal nose is stiff and inelastic; transposition flaps created from this skin produce large standing cutaneous deformities and excessive wound closure tension. Transposition flaps are most useful for repair of defects located on the cephalic nasal sidewall and dorsum in the vicinity of the rhinion. In these areas, the mobility of nasal skin allows ease of transposition and enables dissipation of most of the standing cutaneous deformity that forms from transfer of the flap. Remaining deformities may safely be removed without influencing the vascularity of the flap, thus making the repair one stage (Fig. 18-19). Confining transposition flaps to thin skin zones of the nose reduces contour irregularities by maintaining similar tissue thickness of the flap and recipient site. In contrast, transposition flaps transferred from thin to thick skin zones inevitably result in a mismatch of tissue thickness and create a permanent unnatural topography in the region of reconstruction.

FIGURE 18-18 A, A 1.2 × 1.2-cm skin defect of nasal sidewall. Transposition flap designed for repair. B, Flap transposed. C, D, Postoperative view at 1 year. No revision surgery performed.
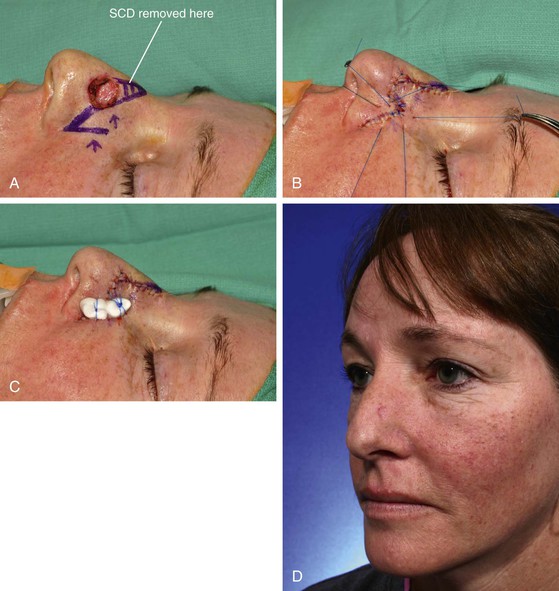
FIGURE 18-19 A, A 1.5 × 1.6-cm skin defect of nasal sidewall. Transposition flap designed for repair. Standing cutaneous deformity (SCD) marked. Arrows indicate orientation of greatest wound closure tension. B, Flap transposed and wound closed. Bolster sutures in place. C, Bolster dressing in place. D, Postoperative view at 2 years. Scar dermabraded.
V-to-Y Island Pedicle Advancement Flap
Small skin defects located in the region of the anterior alar groove between the ala and tip may be effectively repaired with a V-Y advancement flap transferred as a cutaneous island and based on a subcutaneous tissue pedicle consisting of nasalis muscle and subcutaneous fat. It is useful for skin defects up to 1.5 cm in maximum dimension located in the junctional zone between the nasal tip and ala, including the nasal facet (Fig. 18-20).




FIGURE 18-20 A, A 0.8 × 0.7-cm skin defect of alar groove. V-Y island subcutaneous tissue pedicled advancement flap designed for repair. B, Flap incised and advanced on nasalis muscle. C, Flap in place. D, Postoperative view at 4 months.
A triangular flap, with its base making up the cephalic border of the defect, is designed with the apex of the flap positioned laterally. The inferior border of the flap rests in the alar groove. The superior border extends laterally from the defect to include skin of the nasal sidewall and tapers to meet the inferior border in the alar-facial sulcus. The flap is incised to the level of the perichondrium of the lateral crus. The adjacent skin is undermined widely over the nasal tip, dorsum, and sidewall, extending inferiorly beneath the skin of the ala to the level of the caudal border of the defect. Beginning at the cephalic border of the defect, fine scissors are used to undermine beneath the cutaneous island, liberating the distal third of the island from soft tissue attachments. Next, the proximal (lateral) third of the flap is dissected in the subcutaneous plane, freeing it from surrounding tissue. The muscle and subcutaneous fat underlying the central third of the flap are not disturbed and represent the pedicle (Fig. 18-21). It is this zone of tissue attachment, located in the central portion of the alar groove, that provides mobility to the flap so that it may be advanced as far forward as the nostril margin. The pedicle is bluntly freed from the upper and lower lateral cartilages sufficiently to permit only the exact degree of flap advancement necessary for wound repair. The vascular supply to the flap is from the alar branch of the angular artery. This branch is occasionally observed during the dissection; it perforates the deep tissues in the extreme lateral aspect of the alar groove. The vessel is preserved whenever possible to provide the flap with a more axial vascular supply. The flap is secured at the recipient site first, and then the donor site is closed, creating a Y configuration to the repair.

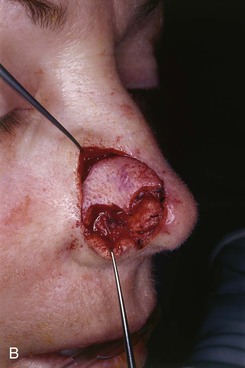


FIGURE 18-21 A, A 1 × 1-cm skin defect of lateral tip and alar groove. V-Y island advancement flap incised. B, Muscle and subcutaneous fat underlying central third of flap provide vascular supply to flap. C, Flap in place. D, E, Preoperative and 6-month postoperative views. No revision surgery performed.
Dorsal Nasal Flaps
The dorsal nasal flap recruits redundant skin of the glabella and is a pivotal flap that can be used to repair skin defects of the nasal tip, dorsum, and sidewall. The dorsal nasal flap enables the surgeon to repair relatively large caudal and midnasal defects measuring 2.5 cm in diameter or less with matching adjacent tissue. There is insufficient nasal skin to repair larger defects in this manner. The flap is ideally suited for elderly patients for repair of defects located centrally on the tip. By necessity, the flap is large to maximize tissue movement and to decrease wound closure tension at the donor site. Distortion of the free margins of the nasal tip and alae is prevented by the compensatory size of the flap, which incorporates the majority of the remaining nasal skin. It is imperative to assess skin laxity and to plan for some degree of secondary movement at the free margins of the nasal alae and tip. Skin laxity in the glabella and dorsal nasal regions is best determined by the pinch test, which consists of grasping the skin between the surgeon’s thumb and index finger and determining the amount of redundancy.13 For success, sufficient skin laxity is present when the surgeon can gather 1 to 2 cm of skin on the nasal bridge and glabella. Greater laxity is necessary as the size of the defect increases.
The author occasionally uses a modified design of the dorsal nasal flap for midline skin defects of the cephalic dorsum (see Chapter 7 for in-depth discussion). The design is such that the lateral border of the flap remains anterior to the thin skin of the medial canthal region to avoid mismatch in skin thickness. I call this design a dorsal heminasal flap. The design limits the arc of tissue movement; therefore, the modified flap may be used only for smaller (less than 2 cm) skin defects of the nasal bridge that are cephalad to the nasal tip. The dorsal heminasal flap usually requires a glabellar incision. The lateral incision is along the junction of the nasal sidewall and dorsum and therefore recruits skin only from the nasal bridge and lower central forehead (Fig. 18-22).




FIGURE 18-22 A, A 1 × 1-cm skin graft on dorsum marked for excision. Dorsal heminasal flap designed for repair of wound after excision. Anticipated standing cutaneous deformity from pivot of flap marked with vertical lines. B, Graft excised and flap dissected. C, Flap in place. D, Postoperative view at 8 months. Flap dermabraded.
Bilobe Flaps
The bilobe flap has a geometrically precise configuration; design of the flap is discussed in detail in Chapter 10. The ideal nasal defect for repair with a bilobe flap is a small (less than 1.5 cm) defect at least 5 mm from the margin of the nostril located on the tip or sidewall. The flap is preferably based laterally and is designed so that the standing cutaneous deformity resulting from pivoting of the flap is removed parallel to or in the alar groove. When it is designed as a laterally based flap, the base of the standing cutaneous deformity develops at the lateral border of the defect with its apex pointing laterally. The base of the deformity is approximately one-half to two-thirds the diameter of the defect. Each lobe is designed with greater and lesser arcs that have the same center point (Fig. 18-23). This point is placed in or parallel to the alar groove at a distance from the lateral border of the defect equal to the radius of the defect. By use of this point, two arcs are created. The lesser arc bisects the defect, passing through the center of the defect. The greater arc is designed so it is tangent to the defect border most peripheral to the center point of the arc. Both lobes of the bilobe flap arise from the lesser arc. The height of the first lobe extends from the lesser to the greater arc. The height of the second lobe is twice the height of the first lobe and is triangulated to facilitate closure of its donor site. The width of the first lobe is designed equal to the diameter of the defect, which prevents elevation of the nostril free margin. The width of the second lobe may be reduced to two-thirds the width of the first lobe. The linear axes of each lobe are positioned at approximately 45° from each other with the primary lobe axis positioned 45° from the axis of the defect. The flap is elevated just above the perichondrium and periosteum of the underlying nasal framework. If the thickness of the primary lobe is greater than the recipient area, the lobe may require thinning even to the level of the dermis to match the thickness of the skin at the recipient site. After incision of the flap, wide peripheral undermining of essentially all of the skin of the nose is important to reduce wound closure tension, to facilitate flap transfer, and to minimize trap-door deformity. The first lobe of the flap is transposed into the defect and secured with sutures. Next, the donor site of the second lobe is closed primarily. Last, the second lobe is inset and trimmed appropriately to fit, without redundancy, the donor defect of the first lobe.
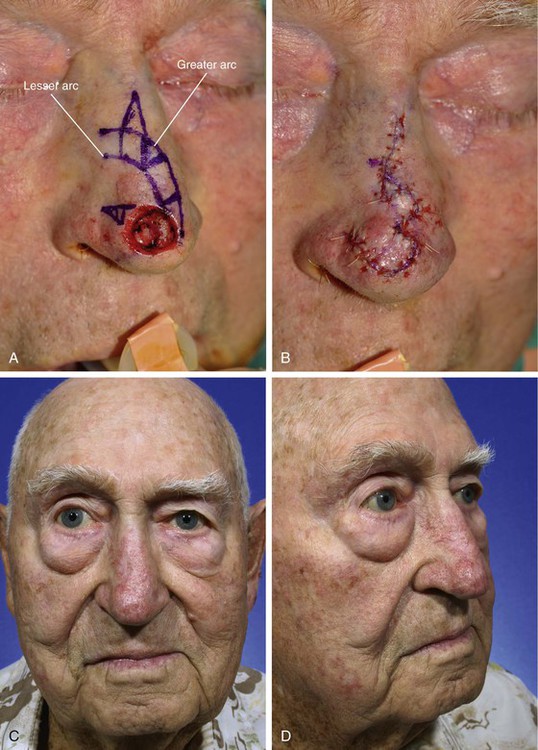
FIGURE 18-23 A, A 1.4 × 1.2-cm skin defect of tip. Bilobe flap designed for repair. Anticipated standing cutaneous deformity marked for excision in alar groove. Base of each lobe arises from lesser arc. Height of first lobe extends from lesser to greater arc. Height of second lobe twice height of first lobe. B, Flap in place. C, D, Postoperative views at 6 months. No revision surgery performed.
The bilobe flap is most useful in patients with nasal tip defects and having thin nasal skin. The flap is also useful for repair of skin defects of the lateral tip or caudal nasal sidewall (Figs. 18-24 and 18-25). In such cases, the flap is constructed from the lax skin along the nasal sidewall. The surgeon may estimate skin laxity by pinching the lateral nasal skin between the thumb and index finger. Patients with thick sebaceous skin have a higher risk of flap necrosis and development of trap-door deformity. Dermabrasion, 6 weeks after flap transfer, is recommended for most patients reconstructed with a bilobe flap.
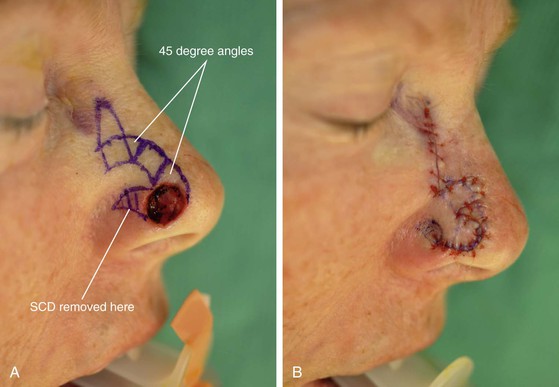
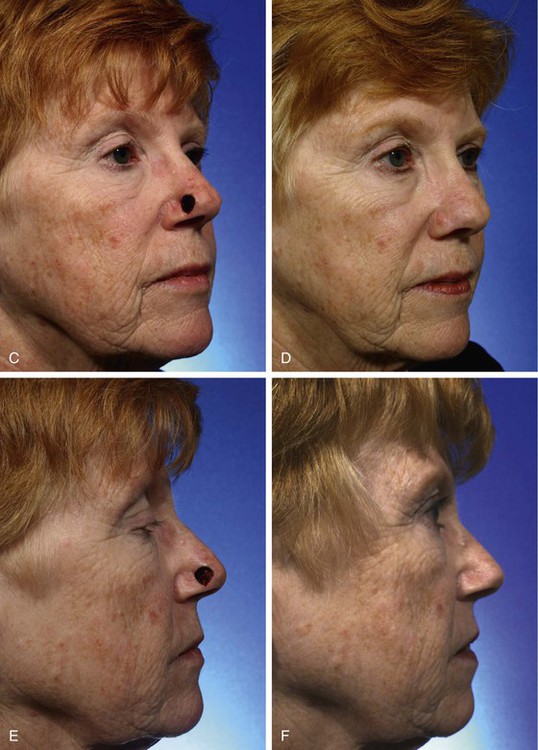
FIGURE 18-24 A, A 1.1 × 1.1-cm skin defect of lateral nasal tip. Linear axes of each lobe designed 45° from each other. This creates 45° skin triangles between lobes. Standing cutaneous deformity (SCD) marked. B, Flap in place. C-F, Preoperative and 1-year postoperative views. No revision surgery performed.
Melolabial Interpolated Flap
Most nasal cutaneous malignant neoplasms occur on the caudal third of the nose. Commonly, after micrographic surgery, the surgeon is requested to reconstruct the ala. Small skin defects of the tip, dorsum, or sidewall may be left to heal by secondary intention. Although this may at times create an unsightly scar, it rarely results in functional impairment. In contrast, even very small defects (1 cm) of the ala left to heal by secondary intention cause notching of the nostril and may cause partial collapse of the external nasal valve, especially on inspiration. For this reason, essentially all cutaneous defects of the ala require reconstruction. Most often it is necessary to use a melolabial interpolated flap as the covering flap for the ala. The predominant reason to use this flap rather than a transposition flap is that transposition flaps transferred from the cheek to the nose deform the alar-facial sulcus and lateral portion of the alar groove. A portion of the flap by necessity must pass through the superior aspect of the alar-facial sulcus, which represents an important topographic junction between the facial aesthetic regions of the nose, cheek, and upper lip. Whenever possible, local flaps should be designed so they do not cross borders that separate aesthetic regions. This is especially true if the border has a concave topography like that of the alar-facial sulcus.4 Too often, this sulcus has been violated by transposition flaps harvested from the cheek to reconstruct caudal lateral nasal defects. The flap passes through the sulcus, obliterating the valley between the ala and cheek. When this happens, it is extremely difficult to restore the valley to a completely natural contour. For this reason, an interpolated melolabial flap is recommended for reconstruction of the ala. The pedicle of the flap crosses over the alar-facial sulcus, avoiding the sulcus altogether. The pedicle may consist of skin and subcutaneous fat or subcutaneous fat only and is detached from the cheek 3 weeks after the initial transfer to the nose. Although 3 weeks is a lengthy period for the patient to endure the deformity caused by the flap, this interval enables the surgeon to thin and sculpt the subcutaneous tissues of the distal flap at the time of flap transfer and the proximal portion of the flap at the time of pedicle detachment and flap inset. On inset of the flap, the patient is left with a completely natural alar-facial sulcus because no incision or dissection has been performed in this region.
The nasal-alar unit is highly contoured, has a free margin, and functions as the external nasal valve. When the ala is reconstructed, consistent restoration of function requires a cartilage subsurface framework to resist the forces of contraction, to provide a stable external valve, and to serve as a scaffold for contour. The framework in the form of a cartilage graft is used at the time of the initial reconstructive procedure and requires vascularized tissue superficial and deep to the graft, totally enveloping the cartilage (Fig. 18-26). Adequate function of the nose requires a thin internal layer most appropriately supplied by vascularized mucosa. The external covering flap is provided by an interpolated cheek or forehead flap.
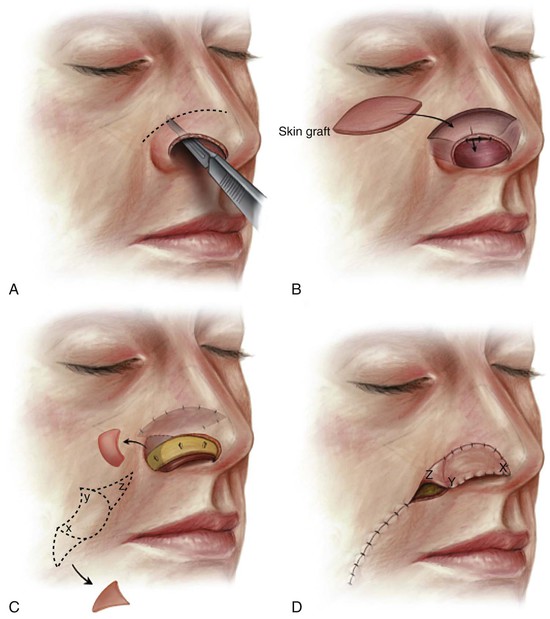
FIGURE 18-26 A, Bipedicle vestibular skin advancement flap used to line full-thickness alar or unilateral tip defects that have vertical dimension of 1 cm or less. Flap created by extended intercartilaginous incision between lateral crus and caudal aspect of upper lateral cartilage (broken line). B, Remaining vestibular skin mobilized caudally in form of bipedicle advancement flap. Flap donor site repaired with thin full-thickness skin graft. C, Auricular cartilage graft provides framework for nostril margin. Graft secured to vestibular skin flap with mattress sutures. Remaining skin of alar base discarded. Interpolated cheek flap designed (broken line). D, Interpolated flap based on subcutaneous tissue pedicle turned toward midline as covering flap. Note orientation of flap relative to design. Cheek donor site closed primarily after removal of standing cutaneous deformity inferiorly, which is used as source for skin graft. (From Baker SR: Interpolated cheek flaps: reconstruction of the alar and columellar units. In Baker SR, editor: Principles of nasal reconstruction, ed 2, New York, Springer, 2011.)
The porous and sebaceous nature of medial cheek skin closely resembles that of the caudal third of the nose, so an interpolated cheek flap is generally the preferred covering flap for alar reconstruction. The flap is based superiorly on the rich vascular supply in the region of the alar-facial sulcus.14 In this location, perforating branches from the angular artery penetrate the levator labii muscle. Other perforating vessels on both borders of the midportion of the zygomatic major muscle assist in supplying the cheek skin adjacent to the ala. The superiorly based flap may be designed as a peninsular flap based on a cutaneous pedicle or as an island based on a subcutaneous tissue pedicle. In most circumstances, I prefer to design the flap as a crescent-shaped island of skin based on a subcutaneous tissue pedicle. The superior extent of the island remains 5 mm below the alar-facial sulcus, preserving this important aesthetic area (see Fig. 18-26).4
An exact template of the alar unit is made from the contralateral normal side with a malleable material such as foil or a thin sheet of foam rubber (Fig. 18-27). The template is reversed to design the interpolated cheek flap. When the defect extends beyond the confines of the ala, a template is designed slightly smaller than the defect to accommodate the phenomenon of distraction of the wound margins, which creates an open wound that is larger than the surface area of the skin removed. If excision of additional skin is indicated to resurface an adjacent aesthetic unit, the template is fashioned before the remaining skin is removed because of this same phenomenon.



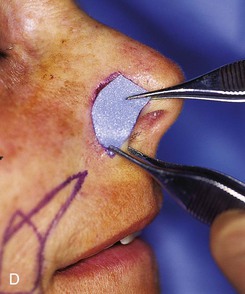




FIGURE 18-27 A, A 1.5 × 1-cm skin defect of ala. Remaining skin of aesthetic unit marked for excision. B, Auricular cartilage used for framework of ala. C, Skin excised and cartilage graft sculpted and positioned along nostril margin. D, E, Foam rubber sheet used to create template of defect and to design flap. F, Interpolated melolabial island flap designed as covering flap for ala. G, Flap transfer to nose based on subcutaneous tissue pedicle. H, I, Preoperative and 3-year postoperative views. Flap contouring procedure performed.
The fashioned template is placed on the melolabial fold so that the center of the flap is positioned 1 cm superior to the horizontal plane of the lateral oral commissure. The template is positioned over the melolabial fold so that the medial border of the designed flap lies in the melolabial crease. This arrangement ensures that the flap is harvested from the cheek, not the lip, and that donor site wound closure will lie within the melolabial crease, providing maximum scar camouflage. The flap is designed to pivot 90° toward the midline in a clockwise direction when it is harvested from the left cheek and counterclockwise when it is harvested from the right cheek. Thus, the template is positioned to design the flap with a specific orientation. As the flap is pivoted and transferred to the recipient site, the in situ medial border of the flap is sutured to the cephalic border of the defect. This in turn causes the in situ inferior border of the flap to join the anterior border of the defect. The lateral border of the in situ flap becomes the inferior border of the reconstructed ala (see Fig. 18-26).
A tracing is made around the template. A triangle of skin is marked superior and inferior to the tracing to fashion a crescent-shaped island of skin (see Fig. 18-27). The two triangles extending from the template tracing represent standing cutaneous deformities that will form when the cheek wound is closed. The lower triangle of skin is excised at the time of flap transfer, and the upper triangle is transferred with the skin of the flap and is discarded at the time of pedicle detachment and inset of the flap. The superior triangle of skin is minimized to reduce loss of tissue from the superior melolabial fold where the fold is well developed. Removal of skin from the superior portion of the fold may result in asymmetry of the medial cheeks.
The flap is incised, and the distal portion is elevated in the subcutaneous plane. The distal third of the flap is thinned, leaving 1 to 2-mm of subcutaneous fat attached to the undersurface. As the dissection proceeds superiorly, the plane extends deeper to facilitate development of the subcutaneous tissue pedicle (Figs. 18-28 and 18-29). The pedicle of fat is freed from the surrounding cheek fat by incising through the borders of the pedicle perpendicular to the surface of the skin. The depth of the incision is carried to the level of the superficial surface of the zygomatic major and levator labii muscles. On reaching the zygomatic major muscle, blunt dissection continues upward on the surface of the muscle, releasing the attachments of the pedicle to deeper structures until the flap can reach the recipient site without undue tension.








FIGURE 18-28 A, Skin defect of ala prepared for reconstruction with interpolated melolabial subcutaneous tissue pedicled island flap. Auricular cartilage graft in place for framework of ala. B, Island flap incised. C, Flap transferred on substantial subcutaneous tissue pedicle based adjacent to alar-facial sulcus. D, Flap in place. E, One week after transfer of flap to nose. F, Three weeks after transfer, pedicle divided and flap inset. G, Subcutaneous tissue pedicle amputated and cheek wound closed. H, Flap trimmed of excess skin and inset.

FIGURE 18-29 A-D, Same patient shown in Figure 18-28. Preoperative and 3-month postoperative views. No revision surgery performed.
When the alar defect extends into the alar-facial sulcus and medial cheek, a cutaneous cheek advancement flap is necessary to repair the cheek component of the defect. In this circumstance, the cheek advancement flap is dissected first, exposing the underlying subcutaneous tissues of the cheek. A cutaneous island transferred as a subcutaneous tissue pedicled interpolated flap is used as covering for the constructed ala. The island flap is dissected, and the pedicle is delivered to the nose beneath the cheek advancement flap (Fig. 18-30). The island flap does not require inset; however, the pedicle usually causes excessive fullness adjacent to the alar-facial sulcus. Thus, a procedure to contour the region is often necessary and is performed 2 to 3 months after flap transfer. On occasion, a second contouring procedure may even be necessary (Fig. 18-31).


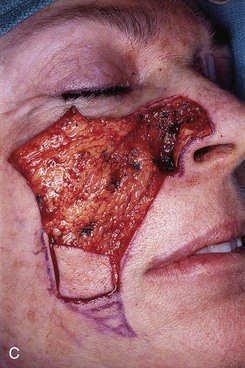
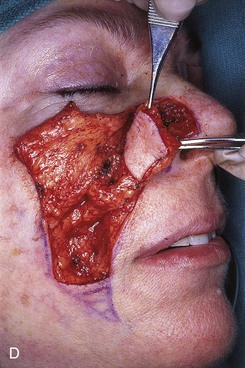

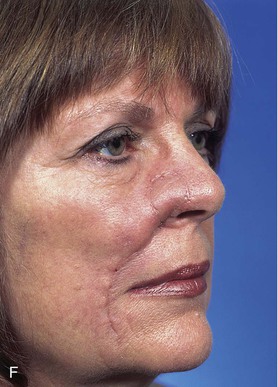





FIGURE 18-30 A, A 3 × 3-cm skin defect of ala and alar-facial sulcus. Interpolated subcutaneous tissue pedicled island flap designed for repair of alar component of defect. Broken line indicates pedicle of island flap; unbroken line marks melolabial crease; horizontal lines mark anticipated standing cutaneous deformity resulting from transfer of flap. Arrow indicates direction of cheek advancement flap. B, Auricular cartilage framework graft in place. C, Cheek advancement flap dissected to repair cheek component of defect. Flap reflected laterally for exposure to dissect subcutaneous tissue pedicle of island flap. D, Island flap based on subcutaneous tissue pedicle transferred to ala. E, Cheek advancement flap and island flap in place. F, Postoperative view at 1 month. Subcutaneous tissue pedicle of interpolated flap obliterates alar-facial sulcus. G, Contouring procedure performed to create alar-facial sulcus. H, Two months after contouring procedure. Fullness in area of reconstruction necessitated second contouring procedure. I, Patient marked for second contouring procedure 6 months after first contouring procedure. J, Alar groove constructed and cheek scar revised. K, Cotton bolster dressing used to maintain constructed alar groove.

FIGURE 18-31 Same patient shown in Figure 18-30. A-D, Preoperative views and postoperative result at 1 year, 3 months. Two contouring procedures and cheek scar revision performed.
Cheek flaps are inset 3 weeks after transfer. For subcutaneous tissue pedicled flaps, the pedicle is transected at the base, and the cheek skin is undermined for a distance of 2 cm around the periphery of the wound. After re-excision of the skin margins with a scalpel, the wound is closed by advancing the borders together (see Fig. 18-28). As this is accomplished, it is usually necessary to open the superior end of the donor site scar to facilitate excision of redundant subcutaneous tissue and a small standing cutaneous deformity that often forms as the wound margins are approximated.
The proximal portion of the flap attached to the nose is released from attachments to the adjacent nasal skin for a distance of 0.5 to 1.0 cm to achieve sufficient freedom to unfurrow the flap. Release enables the surgeon to remove excessive subcutaneous fat not trimmed at the time of flap transfer. The residual skin of the alar unit is excised if it is present. However, a 1-mm fringe of skin at the junction of the ala and the alar-facial sulcus is preserved (see Fig. 18-28). The flap is precisely trimmed to fit the skin defect and sutured in place with simple interrupted 5-0 fast-absorbing plain gut sutures. When the alar base is absent, the flap is tailored to replace the missing base and is integrated with the nasal sill. When the sill requires reconstruction, the flap is trimmed so that it has a tapered end that may serve as the sill. The end is turned medially and sutured to the upper lip.
A necessary third surgical stage in 75% of cases is subsequent flap contouring and the creation of an alar groove. It is performed 3 months after flap inset. A template of the contralateral normal alar unit is made, reversed, placed over the reconstructed ala, and traced carefully with a marking pen. The superior border of the tracing represents the appropriate location for the alar groove. If the superior border of the flap is no more than 1 cm superior to the border of the tracing, the scar marking the juncture of the flap and native nasal skin is used as the access incision for contouring the flap. If a larger portion of the sidewall was resurfaced, a 3-cm incision is made along the superior border of the tracing. The flap is undermined, leaving a few millimeters of subcutaneous fat attached to the dermis. For men, the flap is elevated in a more superficial plane immediately below the dermis to expose all of the hair follicles transferred from the cheek. This may require undermining of the entire flap caudally to the level of the nostril margin. The exposed follicles are cauterized individually under magnification with a fine-tipped monopolar electrocautery. The power setting of the cautery device is set sufficiently low to prevent damage of the adjacent dermis. To ensure flap survival in patients who use tobacco, it may be prudent to depilate the flap in two stages: the superior part of the flap at the time of flap contouring and restoration of the alar groove and the inferior part 2 to 3 months later.
Flap contouring and construction of an alar groove are accomplished by removal of scar tissue and the majority of the remaining subcutaneous fat beneath the flap. Excision continues deeply until the cartilage graft used in the first surgical stage is exposed. A trough of cartilage centered under the planned alar groove is excised from the graft with a scalpel. The trough typically measures 4- to 5-mm wide and extends along the entire projected length of the groove. See Chapter 27 for a detailed discussion of flap contouring and refinement. Care is taken not to deepen the cartilage trough excessively as this may cause a depressed narrow furrow to form in place of the shallow valley of the alar groove typically observed in most noses. Some of the cartilage shavings may be replaced if it is overcorrected. Proper contour is determined by replacing the skin of the flap and compressing it gently. Continued excision of soft tissue and cartilage is performed until the constructed groove is topographically identical to its counterpart. A dental cotton roll is cut longitudinally and used as a bolster. It is secured in place along the length of the constructed groove by passing interrupted 4-0 polypropylene sutures full thickness through the nose in such a manner as to straddle the groove. The roll offers an effective method of obliterating potential dead space, enhancing hemostasis, and maintaining the constructed groove. The bolster is removed on the fifth postoperative day along with the cutaneous sutures. Alternatively, full-thickness horizontal mattress transnasal bolster sutures of 4-0 plain gut are placed to eliminate dead space between the flap and deep tissues. These must be tied loosely to prevent skin necrosis as the flap swells postoperatively. The third stage of contouring the cartilaginous framework and subcutaneous tissues completes the reconstruction of the ala. It has the effect of improving the patency of the reconstructed nasal airway by removing excessive bulk in the area of the internal nasal valve.15,16
The peninsular flap is the other form of the melolabial interpolated flap used to reconstruct the ala. It depends on the dermal and subdermal vascular plexuses of the cutaneous pedicle to provide vascularity to the distal flap. The cutaneous pedicle must be of sufficient width and thickness to ensure this vascularity. In designing a peninsular flap, the orientation of the template remains the same as in designing an island flap (Fig. 18-32). The width of the cutaneous pedicle is approximately the width of the template, although it may be narrower than the template when a wide (more than 2 cm) flap design is required. The peninsular flap is elevated in a subcutaneous plane, maintaining 3 mm of fat on the undersurface of the cutaneous pedicle. This is in contrast to the island flap, based on a subcutaneous tissue pedicle that may be as much as 1.5 cm thick. Thus, the plane of dissection for the peninsular flap is considerably more superficial. Like the island flap, the peninsular flap pivots 90° toward the midline and is sutured to the nose in a fashion similar to that described for the island flap. Care is taken not to kink the pedicle on transfer of the flap. Like the island flap, the distal half of the flap may be thinned as necessary to replicate the thickness of the recipient site. The proximal portion of the flap bridging between cheek and nose is not thinned to ensure an ample vascular supply. The cheek wound is closed by a method identical to that for the island flap.
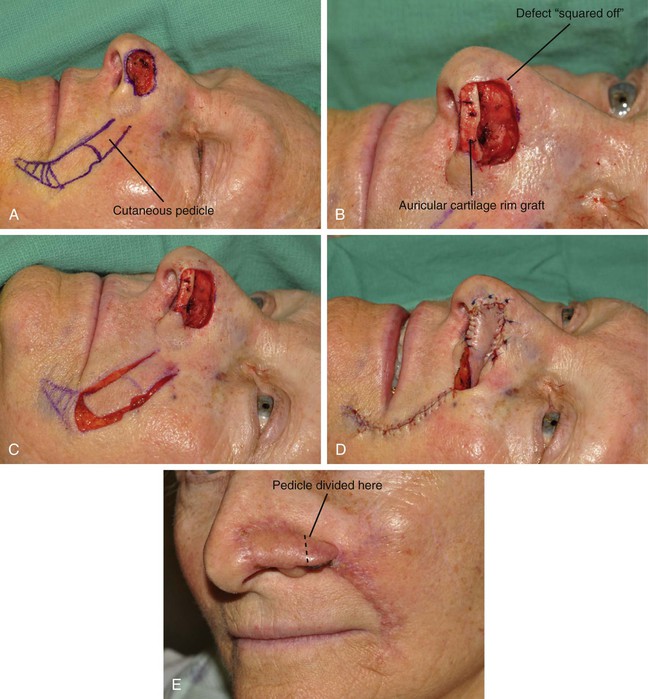


FIGURE 18-32 A, A 2 × 1.4-cm cutaneous defect of lateral tip and alar groove. Cutaneous pedicled interpolated melolabial flap designed for repair. B, Defect enlarged to create square corners. Auricular cartilage rim graft in place for support of nostril. C, In situ flap incised. D, Flap transferred to nose. E, Three weeks after initial transfer, flap is inset. F-K, Preoperative and 3-year postoperative views. No revision surgery performed.
Similar to the island flap, the peninsular flap remains attached to the cheek for 3 weeks to enable the establishment of collateral vascularity. The pedicle is divided at a second stage (see Fig. 18-32E), and the proximal portion of the pedicle is inset in the cheek by opening the superior portion of the donor site scar for 1 to 2 cm. The wound edges are spread widely, creating a space to accommodate the proximal pedicle. The skin adjacent to the opened wound is undermined for 2 cm. This allows the cheek skin to contract, assisting in enlarging the wound. The pedicle stump is then trimmed to precisely fit the wound and inset in the melolabial fold, creating a V-shaped wound closure. Returning most of the skin of the proximal pedicle to the cheek helps maintain the natural fullness observed in the superior portion of the melolabial fold.
Paramedian Forehead Flap
Paramedian forehead flaps are the preferred local flap for resurfacing most large nasal defects. The reader is referred to Chapter 13 for an in-depth discussion of the paramedian forehead flap, which is the sole topic of the chapter. The flap is usually dissected under local anesthesia. The base of the pedicle is placed in the glabellar region centered over the supratrochlear artery on the same side as the majority of the nasal defect (Fig. 18-33). The origin of the supratrochlear artery is consistently found to be 1.7 to 2.2 cm lateral to the midline and usually corresponds to the vertical tangent of the medial border of the eyebrow.17 The artery exits the orbit by piercing the orbital septum and passing under the orbicularis oculi and over the corrugator supercilii muscle. At the level of the eyebrow, the artery passes through orbicularis and frontalis muscles and continues in a vertical direction upward in a subcutaneous tissue plane. Because of this, the portion of the flap extending from the level of the eyebrow to the hairline can be trimmed of its frontalis muscle and much of the subcutaneous fat without harming the blood supply to the overlying skin. The axial nature of the flap, based on a single supratrochlear artery, enables the pedicle to be as narrow as 1.2 cm.17 The narrow pedicle minimizes the standing cutaneous deformity that develops as the flap pivots. An exact template of the defect is used to design the paramedian forehead flap, which is centered over the vertical axis of the supratrochlear artery. The length of the flap is determined by measurement. If an adequate length necessitates extending the flap into the hair-bearing scalp, the author prefers turning the flap obliquely along the hairline to prevent transfer of hair-bearing skin to the nose. However, this design may not be prudent if the flap must be more than 3 cm in width. Oblique forehead flaps wider than 3 cm remove excessive skin from the lateral portion of the forehead, sometimes causing unsightly scars or upward distortion of the central portion of the eyebrow. Thus, flaps wider than 3 cm should be extended into the hair-bearing scalp rather than designed in an oblique fashion.



FIGURE 18-33 A, A 1.9 × 1.4-cm skin and soft tissue defect of ala and medial cheek. Cheek flap advanced to alar-facial sulcus. Auricular cartilage graft provides framework for alar construction. B, C, Paramedian forehead flap provides external cover for defect. D-I, Preoperative views and postoperative result at 1 year, 9 months. Three contouring procedures and forehead scar revision performed. Right temple and nasal tip defects repaired with full-thickness skin grafts.
The paramedian forehead flap is elevated in a subfascial plane just superficial to the periosteum of the frontal bone. To avoid injury to the arterial pedicle, blunt dissection is used near the eyebrow to separate the corrugator muscle from the flap and to facilitate mobility. Incisions may be extended below the eyebrow if necessary to increase the length of the flap. Adequate flap mobilization usually requires complete sectioning of the corrugator supercilii muscle to achieve free movement. Before the flap is sutured in place, the flap is sculpted and contoured to fit the depth of the defect perfectly by removal of all or some of the muscle and subcutaneous tissue from the distal portion. When necessary, all but 1 mm of fat beneath the dermis may be removed. In instances in which the nasal skin is quite thin, it is sometimes even necessary to resect a portion of the dermis along the border of the flap so that the thickness of the skin of the flap matches the adjacent nasal skin. This is performed only along the border, not more centrally. Only the distal three-fourths of the surface area of the flap required for reconstruction is thinned; the proximal one-fourth is left thick and is debulked at the time of pedicle detachment 3 weeks later. Prudence in thinning the flap is advised in patients who smoke. Donor site closure is accomplished by undermining the forehead skin in the subfascial plane from the anterior border of one temporalis muscle to the other. Any portion of the donor site that cannot be closed primarily should be left to heal by secondary intention, keeping the open wound moist at all times. Healing usually results in an acceptable scar, but complete healing may take 6 weeks.
Skin Grafts
Full-Thickness Skin Grafts
A full-thickness skin graft consists of epidermis and full-thickness dermis. It resists contraction, has texture and pigmentation similar to those of normal skin, and requires a well-vascularized, uncontaminated recipient site for survival. The graft survives initially by diffusion of nutrition from fluid in the recipient site, a process called plasma imbibition. Vascular inosculation occurs during the first 24 to 48 hours. After 48 to 72 hours, capillaries in the recipient site begin to grow into the graft to provide new circulation. By 3 to 5 days, a new blood supply has been established. Initially, a full-thickness skin graft appears blanched; during 3 to 7 days, a pink color develops, signaling neovascularization. After 4 to 6 weeks, the pink color begins to fade, but the graft often remains lighter than the surrounding skin, especially in dark-skinned individuals.
Compared with split-thickness grafts, full-thickness grafts have the advantages of better color and texture match with nasal skin, fewer contour irregularities, no need for special equipment to harvest the graft, and easier donor site wound care. The disadvantages include reduced survival rate for larger grafts and longer healing time.18
The areas of the nose covered with thicker skin include the tip, alae, and caudal aspect of the sidewalls and dorsum (see Fig. 18-2). Although the nasal skin is thin in the area of the rhinion, it becomes thicker as it transitions toward the nasion. Full-thickness skin grafts used to repair defects of the nose in regions of thicker nasal skin tend to heal with a contour depression and noticeable textural discrepancies between graft and adjacent nasal skin. This is because the nasal skin in these areas tends to have a more sebaceous nature than the graft.
There is wide variation of nasal skin thickness among individuals, and the overall thickness of the nasal skin is an important preoperative consideration. For similar nasal defects, a skin graft may provide a perfect match in terms of thickness for one person and a poor match for another. There are individuals who have thin nasal skin covering the entire nose. These individuals are often fair-skinned women (Fig. 18-34). Except for patients with extremely thick skin, full-thickness skin grafts may be used in cases of very superficial cutaneous defects anywhere on the nose without the consequence of significant contour or textural discrepancies between graft and nasal skin (Fig. 18-35). The only exception is in the area of the nostril margin, where scar contraction after skin grafting is likely to distort the border of the nostril.


FIGURE 18-34 A, A 3 × 2.5-cm skin defect of nasal tip and dorsum repaired with full-thickness skin graft from supraclavicular fossa. B, Postoperative result at 1 year. Graft dermabraded. Skin grafts may be used to repair superficial skin defects anywhere on nose in individuals with thin nasal skin. Such individuals tend to be fair-skinned women.




FIGURE 18-35 A, A 2.5 × 2.5-cm superficial skin defect of nasal tip. B, Full-thickness skin graft harvested from supraclavicular fossa used to repair defect. C, Bolster dressing in place over skin graft. D, Postoperative view at 9 months. Graft dermabraded. Superficial nature of defect and thin nasal skin provided reasonable likelihood of acceptable aesthetic results with skin graft.
In general, cutaneous flaps from the nose, forehead, or cheek are the preferred method of resurfacing for deeper cutaneous defects of the nose. However, the infratip lobule is one site where a full-thickness skin graft is preferred to a cutaneous flap. Provided the defect does not involve the margin of the nostril and there is no loss of the intermediate crura, cutaneous defects of the infratip lobule are best covered with a full-thickness skin graft harvested from the preauricular or postauricular skin. The match in thickness and color between the skin from these sources and the skin of the infratip lobule is nearly perfect. Six weeks after grafting, the area may be lightly dermabraded to blend the graft with the nasal skin (Fig. 18-36).
Reconstruction of the Nasal Aesthetic Units
Defects of the nose may be classified according to location, depth, and size. Skin-only defects may be replaced with full-thickness skin grafts, local flaps (if the defect is small), or skin transferred from the cheek or forehead. Defects involving loss of skeletal structure require replacement of skeletal support with like tissue. Full-thickness defects of the nose require replacement of the missing lining with flaps harvested from the interior of the nose whenever possible. These defects always require replacement of the missing skeletal framework and thus should be resurfaced with an interpolated paramedian forehead or melolabial flap.
Reconstruction of Columella and Nasal Facets
The columella and nasal facets are the most difficult aesthetic units of the nose to reconstruct. Skin-only defects are best repaired with full-thickness skin grafts (see Fig. 18-36). Small defects of skin and cartilage limited to 1.5 cm in greatest dimension may occasionally be repaired with composite grafts from the auricle in nonsmokers (see Chapter 15 for detailed discussion of composite grafts). The grafts are chilled with ice compresses for 3 days after transfer, and systemic steroids are administered for 1 week. It is preferable to allow the initial defect to heal by secondary intention and then to perform the composite graft after preparation of a fresh recipient site by removal of all scar and neoepithelialization. The graft is oversized by 2-mm to accommodate wound contraction.
Full-thickness defects of the columella and tip are best reconstructed with a pivotal septal composite chondromucosal flap (see Fig. 18-9). Mucosa of the flap is peeled downward bilaterally to provide internal lining. Auricular cartilage grafts are attached to the composite flap to provide structural support laterally. A paramedian forehead flap is best for exterior covering.
Reconstruction of Nasal Tip
Small, skin-only superficial defects of the nasal tip may be repaired with a bilobe nasal flap as described earlier or a full-thickness skin graft. Sizeable defects of the nasal tip may be repaired with a full-thickness skin graft with expectations of an aesthetically pleasing result if the defect is shallow and the adjacent tip skin is thin (see Fig. 18-35). However, a paramedian forehead flap will usually give a more natural result because the entire aesthetic unit can be covered by the flap, placing scars in borders of aesthetic units. Cartilage grafts are used routinely along the margin of the nostril when the defect extends from the tip into the nasal facet. This is in addition to any missing lower lateral cartilage, which is replaced as well.
Bilateral full-thickness defects of the tip and columella are repaired with a pivotal septal composite chondromucosal flap (see Fig. 18-9). However, unilateral full-thickness defects can be nicely reconstructed with an ipsilateral intranasal hinge mucoperichondrial flap for internal lining. If the defect is large, a contralateral dorsal septal mucoperichondrial hinge flap is used to provide lining for the more cephalic portion of the defect (Fig. 18-37). Septal and auricular cartilage grafts are used for the framework. A paramedian forehead flap provides the external cover for the construction of the tip. The ipsilateral lining flap spans the nasal passage on the affected side. Concomitant with inset of the forehead flap 3 weeks after transfer, the hinge mucoperichondrial flap is released from the septum, restoring patency of the nasal airway.


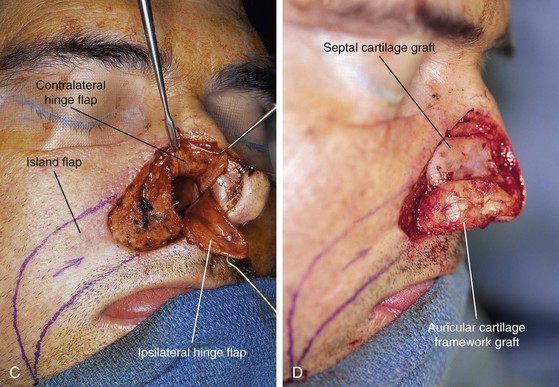


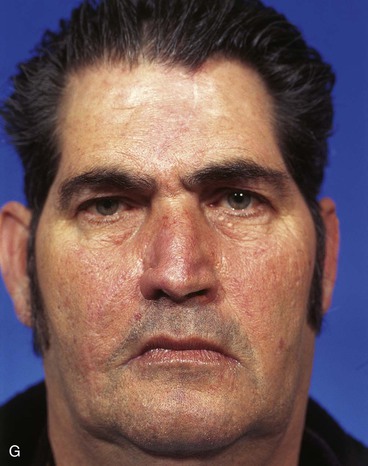
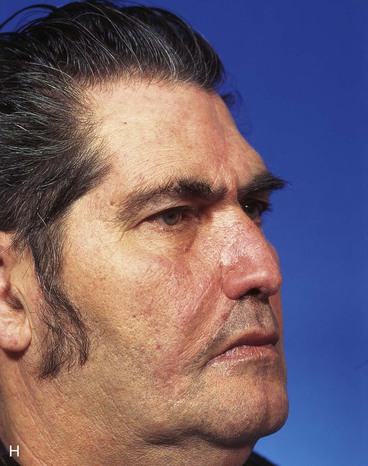
FIGURE 18-37 A, B, Full-thickness defect of nasal hemi-tip, ala, and caudal sidewall. Defect extends into medial cheek. C, Ipsilateral septal mucoperichondrial hinge flap reflected inferiorly and contralateral dorsal septal mucoperichondrial hinge flap reflected superiorly from depths of nasal passage. Flaps provided internal lining to hemi-tip, ala, and sidewall defect. V-Y subcutaneous tissue pedicled island advancement flap designed to repair cheek component of defect. D, Septal cartilage graft used to replace missing upper lateral cartilage. Auricular cartilage graft used for framework of ala and hemi-tip. E, Island flap advanced. Interpolated paramedian forehead flap designed to cover nasal component of defect. Remaining skin of sidewall aesthetic unit marked for excision. F, Flaps in place. Caudal border of forehead flap sutured to caudal border of ipsilateral mucoperichondrial hinge flap. G, H, Postoperative views at 9 months. Contouring procedure performed to create alar groove.
Full-thickness defects of the nasal tip that involve the nostril margin may also be reconstructed by a single paramedian forehead flap folded on itself to provide concomitant internal lining and external cover. This technique is reserved for patients with thin skin (Fig. 18-38) and in cases in which use of a septal mucoperichondrial flap is not possible or would not be prudent. This approach requires a multiple-stage reconstruction. Stage one is the initial transfer of the flap to the recipient site. In the second stage, the lining component of the flap is inset by making an incision through the paramedian forehead flap along the planned nostril margin. The lining flap is thinned of subcutaneous fat and early scar formation. An auricular cartilage graft is positioned along the planned nostril margin, spanning the entire width of the defect. The paramedian forehead flap remaining attached to the forehead is unfurled and used to resurface the external defect, covering the cartilage graft. The third surgical stage involves insetting of the forehead flap, covering the tip defect. The surgical stages are performed at 3-week intervals. It is sometimes necessary to perform a fourth surgical stage, which is to contour the covering flap to maximize the aesthetic result. This is more common in patients with thicker skin.
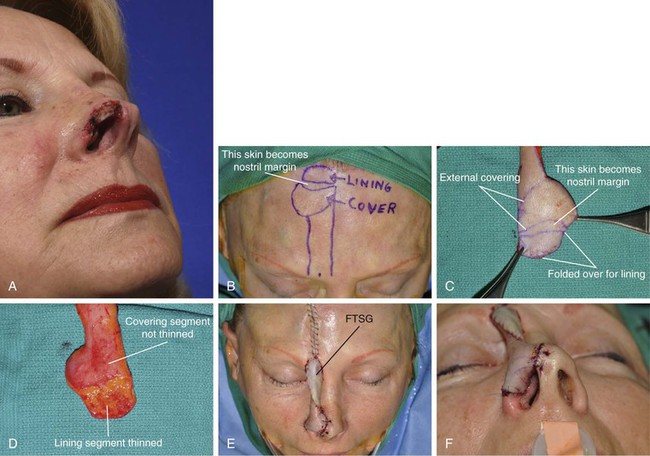
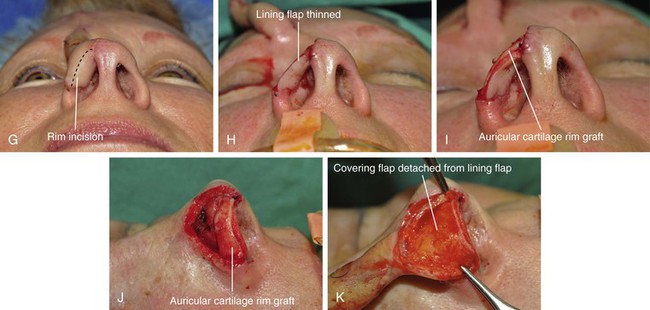
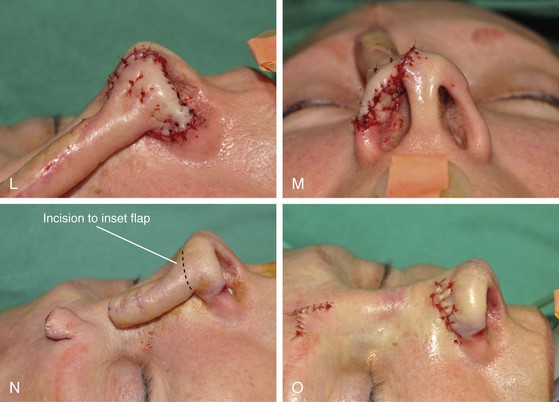


FIGURE 18-38 A, A 2.4 × 1.5-cm full-thickness defect of nasal tip. Caudal border of alar cartilage visible in depth of wound. B, Single paramedian forehead flap designed to resurface internal lining and external cutaneous defects. C, D, Dissected flap. Lining component of flap thinned before folding flap on itself. E, Forehead flap transferred to nose. Pedicle covered with full-thickness skin graft. F, Distal portion of flap provides lining to defect. G, Three weeks after initial flap transfer to nose, lining portion of flap inset by making incision along reconstructed nostril margin. H, Lining flap thinned of early scar deposition. I, J, Auricular cartilage rim graft sutured to lining flap. K-M, Distal portion of remaining forehead flap unfurled, thinned of scar and subcutaneous fat, used to cover cartilage graft and external cutaneous defect. N, O, Three weeks after second surgical stage, covering flap is inset. P-U, Preoperative and 2-month postoperative views after contouring procedure (fourth surgical stage).
Reconstruction of Ala
Skin defects of the ala may be reconstructed by a number of surgical approaches. One approach in patients with limited partial-thickness alar defects who wish to avoid an interpolated cheek or forehead flap is the combination of a subcutaneous tissue hinge cheek flap and full-thickness skin graft. A hinge flap consisting of subcutaneous tissue and harvested from the cheek is used to fill the depths of the nasal defect and is covered with a full-thickness skin graft.19 The flap may also nourish an alar rim cartilage graft when required. This approach is useful only for defects of the ala or sidewall that are not full thickness and are immediately adjacent to or involve the medial cheek or alar-facial sulcus. The technique has the advantage of a one-stage procedure that does not violate the melolabial fold (Fig. 18-39). It avoids the need for an interpolated cheek or forehead flap, and it restores a natural contour to the repair, often achieving comparable aesthetic results. When the nasal defect extends into the cheek, the cheek component is repaired by advancement of cheek skin to the level of the alar-facial sulcus (cheek-nose junction). This places scars in the aesthetic border and restores the sulcus between these structures. The subcutaneous tissue hinge cheek flap is discussed in Chapter 15.

FIGURE 18-39 A, A 1.5 × 1.5-cm skin defect of ala extending to alar-facial sulcus. Auricular cartilage graft held by forceps in anticipation of placing it along caudal border of alar defect. B, Subcutaneous tissue hinge flap harvested from medial cheek reflected medially over cartilage graft. Flap fills depths of defect. C, Borders of hinge flap tucked beneath edges of defect and held in place with mattress sutures. D, Full-thickness skin graft (FTSG) placed over hinge flap for external covering. E, Bolster dressing in place to secure skin graft. F, Postoperative view at 5 months. Graft dermabraded.
Superficial defects of the ala or nostril margin may sometimes be repaired with a full-thickness skin graft. This approach is most effective in patients with thin nasal skin. To reduce the risk of nostril retraction resulting from contraction of the skin graft, a narrow (5-mm) auricular cartilage graft is used to span the width of the defect at the margin of the nostril (Fig. 18-40). Soft tissue tunnels on either side of the defect are created at the inferior border of the nostril to accommodate the medial and lateral ends of the graft. The graft is sutured to the skin of the nasal vestibule with one or two horizontal mattress 5-0 absorbable sutures. A skin graft is then used to cover the skin defect and directly covers the exposed cartilage graft. The graft is secured in place with a gauze bolster dressing for 5 days.
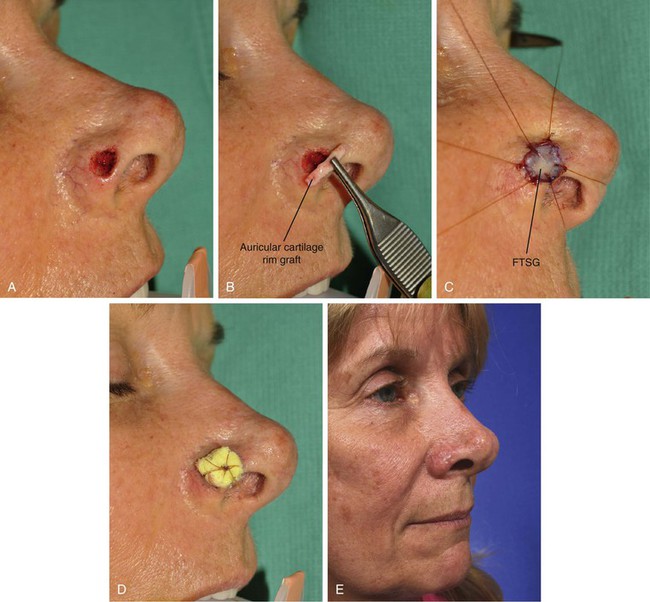
FIGURE 18-40 A, A 1 × 0.8-cm cutaneous defect of ala. B, Auricular cartilage rim graft inserted along nostril margin, spanning defect. C, D, Full-thickness skin graft (FTSG) secured by bolster dressing. E, Postoperative view at 4 months. No revision surgery performed.
Deeper defects confined to the ala with or without limited extension into the nasal tip or sidewall are best resurfaced with a superiorly based interpolated melolabial flap. This flap is discussed in a previous section of this chapter. When using this flap, I routinely resurface the entire ala regardless of the size of the alar defect.4 The melolabial flap based on a subcutaneous tissue pedicle is preferred because this design minimizes the amount of skin that is disturbed in the superior melolabial fold. Preserving the superior fold is paramount in maintaining symmetry of the cheeks after reconstruction of the ala with a cheek flap (Fig. 18-41). Cartilage grafts are used in the majority of alar defects. This is because most lesions involving resection of alar skin also require removal of the underlying firm fibrofatty subdermal tissue that provides the ala form and structural support. This must be replaced by cartilage to prevent upward migration of the ala and notching of the margin of the nostril.







FIGURE 18-41 A, A 1.5 × 1.5-cm deep skin and soft tissue defect of ala. B, Auricular cartilage graft sculpted for framework. Interpolated melolabial subcutaneous tissue pedicled island flap designed for repair of defect. C, In situ incised flap. Cartilage graft in place. Remaining skin of alar aesthetic unit excised. D, Flap transferred on subcutaneous tissue pedicle. E, F, Flap in place. Donor site closed. G, Postoperative view at 7 months. Contouring procedure performed.
Deep alar defects in younger patients without a developed melolabial fold or visible crease are often repaired with a paramedian forehead flap as the covering flap. Flap donor site scars tend to be less apparent on the forehead compared with the medial cheek in these patients (see Fig. 18-33). In addition, men with dark, thick facial hair may be better served with the forehead rather than the cheek as the donor site for covering flaps to repair alar defects (see Fig. 18-39). Use of the forehead flap usually avoids the problems of transferring hair-bearing skin to the ala.
Internal lining for full-thickness alar defects is provided by bipedicle vestibular skin flaps or ipsilateral hinge septal mucoperichondrial flaps (Fig. 18-42). As discussed in an earlier portion of this chapter, an additional contralateral hinge mucoperichondrial flap may be necessary if the vertical height of the defect is such that an ipsilateral hinged mucoperichondrial flap will not provide sufficient tissue to replace the entire missing lining. Defects of the ala that extend into the cheek or upper lip require flaps to repair these aesthetic regions that are independent from the flap used for construction of the ala.20 If the alar defect is full thickness, it is prudent to reconstruct the portion of the defect involving the upper lip as a first surgical stage and to delay the reconstruction of the ala. Alar reconstruction is performed once healing of the lip is complete and all scars have contracted to the maximum degree. This approach creates an upper lip that provides a stable foundation on which to build a new ala (Fig. 18-43).
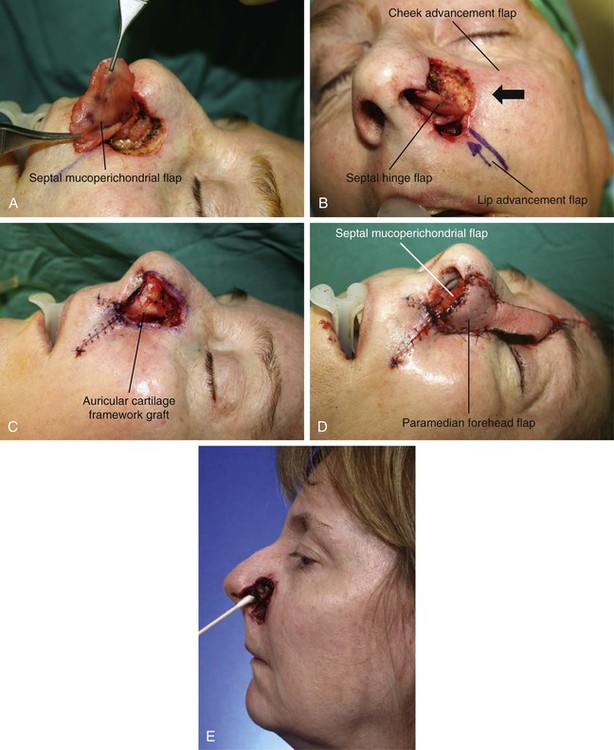

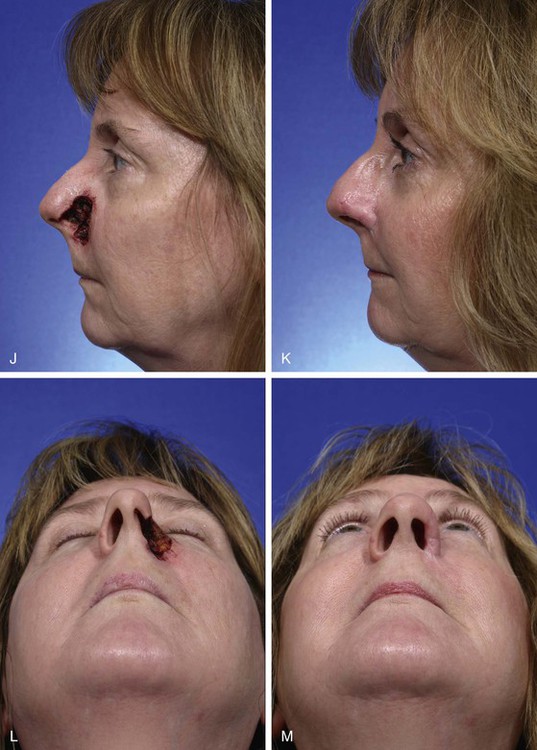
FIGURE 18-42 A, Full-thickness defect of ala and caudal sidewall. Ipsilateral septal mucoperichondrial hinge flap reflected inferiorly for repair of lining defect. B, Lip and cheek advancement flaps created to repair lip and cheek components of defect. C, Lip and cheek advancement flaps in place. Auricular cartilage framework graft provides structural support. D, Interpolated paramedian forehead flap transferred to cover cartilage graft and nasal cutaneous defect. E, Preoperative view demonstrating full-thickness nature of defect. F-M, Preoperative and 11-month postoperative views. Contouring procedure performed 4 months after inset of lining and forehead flaps. (From Baker SR: Intranasal flaps. In Baker SR, editor: Principles of nasal reconstruction, ed 2, New York, Springer, 2011.)


FIGURE 18-43 A, A 3 × 2.6-cm skin and soft tissue defect of medial cheek and 2 × 2-cm full-thickness defect of ala. V-Y subcutaneous tissue pedicled advancement flap designed to repair cheek defect. B, Island flap in place. Stent secures full-thickness skin graft placed along borders of alar defect. C, Postoperative view 3 months after first-stage reconstruction. Missing ala is evident. D, Ipsilateral septal mucoperichondrial flap reflected from nasal passage to provide lining to alar defect. Hinge flap of healed skin graft also used to assist mucosal flap in providing lining to ala. E, Hinged skin flap reflected downward and sutured to mucosal flap held by forceps. F, Auricular cartilage framework graft sutured to skin and mucosal lining flaps. G, Paramedian forehead flap provides external cover for alar reconstruction. H-J, Postoperative result at 1 year. Contouring procedure and Z-plasty lip scar revision performed.
Reconstruction of Nasal Dorsum
The nasal dorsum is perhaps the least complex portion of the nose to reconstruct. Superficial skin defects may be repaired with full-thickness skin grafts with expectant acceptable results. Forehead skin in the form of an interpolated paramedian flap is usually preferred for resurfacing of deeper skin and soft tissue defects of the caudal dorsum. However, bilobe flaps or full-thickness skin grafts may also be used. Likewise, skin defects of the cephalic dorsum may be repaired with glabellar flaps such as the dorsal nasal flap or full-thickness skin grafts. However, paramedian forehead flaps are usually preferred for reconstruction of more extensive dorsal defects, especially if they extend into other aesthetic units of the nose.
Internal lining for full-thickness dorsal nasal defects can usually be provided by mucoperichondrial flaps reflected laterally from the exposed dorsal septum as long as there is sufficient height to the remaining septum.20 Unilateral or bilateral hinge septal mucoperichondrial flaps based on the caudal septum and including the septal branch of the labial artery may sometimes be used for lining when there is not considerable loss of dorsal septal height. A pivotal septal composite chondromucosal flap, as discussed earlier in this chapter, should be used to provide lining and structural support for the dorsum in extensive bilateral full-thickness dorsal nasal defects. In instances in which this approach will not provide sufficient tissue, bilateral paramedian forehead flaps are recommended. One flap provides internal lining and the other provides external coverage. A cranial or rib bone graft is placed between the flaps for structural support.
Reconstruction of Nasal Sidewall
Reconstruction of the sidewall of the nose is relatively uncomplicated. Small skin-only defects of the caudal sidewall may be repaired with a bilobe flap harvested from the remaining nasal sidewall skin. Full-thickness skin grafts harvested from the preauricular area of the cheek or supraclavicular fossa also provide a reasonable option for covering defects located in the cephalic portion of the sidewall because of the thin skin in this location. Larger surface defects are best covered with a paramedian forehead flap (Fig. 18-44). When structural support is absent from the cephalic third of the nasal sidewall, it is replaced with a calvarial bone graft; the caudal two-thirds of the sidewall skeleton is best replaced with septal or costal cartilage grafts. Full-thickness sidewall defects may be lined with contralateral hinged septal mucoperichondrial flaps based on the nasal dorsum and delivered through a superiorly located nasal septal fenestra. For more caudal sidewall defects, a unilateral mucoperichondrial hinge flap based on the caudal septum may provide sufficient lining (Fig. 18-45). However, this approach requires subsequent detachment of the flap’s pedicle. It is usually necessary to use both the contralateral dorsally based flap and the ipsilateral caudally based septal mucoperichondrial hinge flap to provide lining for full-thickness defects that involve the ala and extend the entire length of the nasal sidewall.

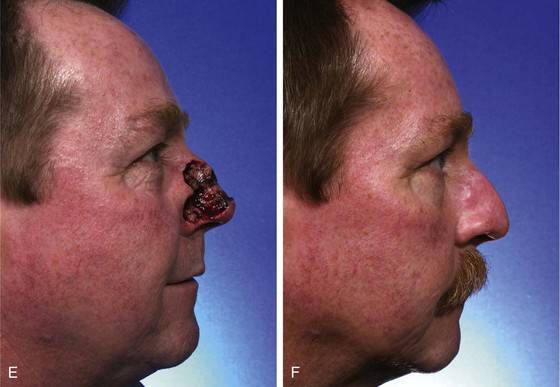
FIGURE 18-44 A-F, Preoperative and 1-year postoperative views after paramedian forehead flap to reconstruct 4 × 3.5-cm skin and soft tissue defect of nasal dorsum, sidewall, and ala. Contouring procedure (third surgical stage) performed 5 months after forehead flap inset. Forehead and nasal scar revisions also performed.
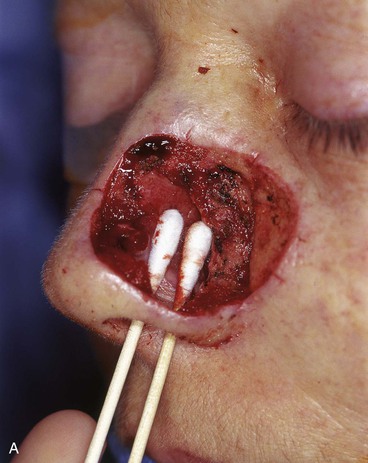
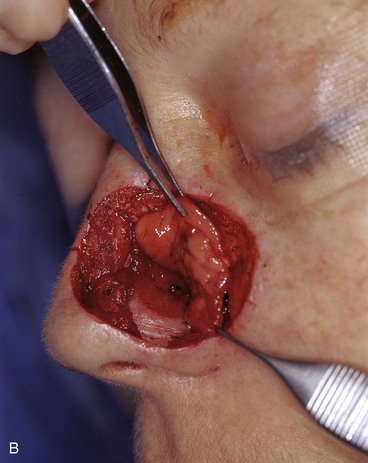
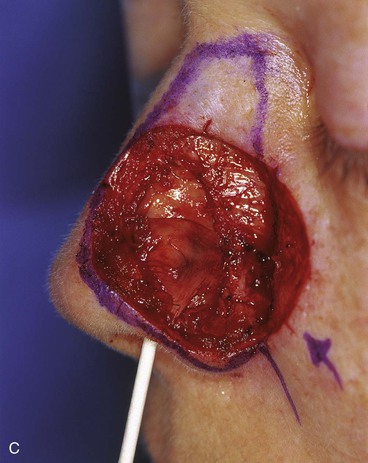




FIGURE 18-45 A, A 3 × 4-cm full-thickness defect of ala, caudal sidewall, and dorsum. B, Ipsilateral septal mucoperichondrial hinge flap dissected for internal lining. C, Septal flap sutured to margins of mucosal defect to seal nasal passage from external exposure. D, Septal cartilage graft (superior) replaces missing upper lateral cartilage. Auricular cartilage graft (inferior) provides framework of ala. E, Interpolated paramedian forehead flap transferred for external covering. F, G, Postoperative views at 2.5 years. Contouring procedure performed.
Flap Refinement
A contouring procedure to create an alar groove is a necessary third surgical stage in 75% of cases of alar reconstruction. This is performed 3 months after inset of an interpolated melolabial or forehead flap used for resurfacing of the ala. The procedure is necessary whenever the defect extends cephalic to the alar groove (Fig. 18-46).
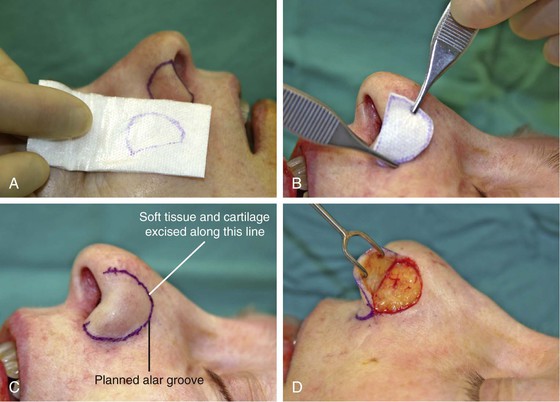
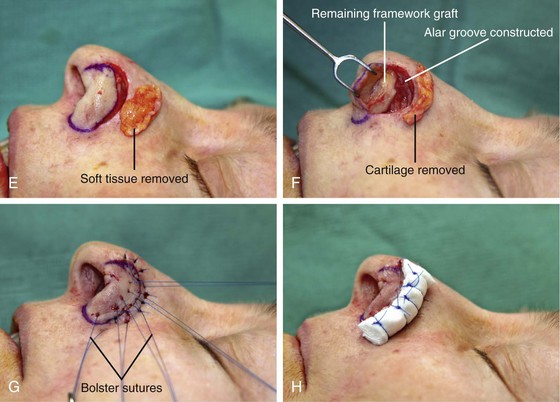
FIGURE 18-46 A-C, Template of contralateral ala used to mark location of planned alar groove. D, Previously transferred interpolated melolabial flap dissected in subdermal plane and reflected inferiorly. E, Soft tissue resting on surface of nose represents tissue removed to contour flap. F, Trough in previously grafted cartilage creates contour of alar groove. G, Flap repositioned. Bolster sutures straddle reconstructed alar groove. H, Cotton bolster secured with sutures along constructed alar groove. (From Baker SR: Interpolated melolabial flaps: reconstruction of alar and columellar units. In Baker SR, editor: Principles of nasal reconstruction, ed 2, New York, Springer, 2011.)
Summary
Reconstruction of the nose has in the last decade progressed to a new level of finesse that allows the surgeon to restore nearly normal form and function to all but the most extensive defects of the nose. These advances are based on the contemporary concepts of respecting the borders of aesthetic units of the nose and replacing missing tissue with like tissue. The nose is reconstructed separately from any extension of a nasal defect into the cheek and lip, which in turn are repaired by tissue within their respective aesthetic regions. Internal lining is replaced with nasal mucoperichondrial flaps, which because of their nature provide adequate vascularity to nourish and to sustain the cartilage and bone grafts used for nasal skeletal replacement. Missing bone and cartilage are replaced with similar tissue that is carefully crafted to replicate the exact size, configuration, and contour of the missing nasal skeleton. The majority of surface defects are covered with cheek or forehead skin transferred by interpolation to prevent disturbance of the aesthetic boundaries between the nose and other regions of the face. This surgical approach provides natural building material precisely fitted to restore nasal deficits to a condition as nearly normal as possible.
References
1. Burget, GC, Menick, FJ. Nasal support and lining: the marriage of beauty and blood supply. Plast Reconstr Surg. 1989; 84:189.
2. Menick, FJ. Reconstruction of the nose, local flaps in facial reconstruction. In: Baker SR, Swanson NA, eds. Local flaps in facial reconstruction. St. Louis: Mosby; 1995:305–337.
3. Burget, GC, Menick, FJ. Aesthetic reconstruction of the nose. St. Louis: Mosby; 1993.
4. Baker, SR, Johnston, TM, Nelson, BR. The importance of maintaining the alar-facial sulcus in nasal reconstruction. Arch Otolaryngol Head Neck Surg. 1995; 121:617.
5. Baker, SR, Contemporary aspects of nasal reconstruction. Advances in otolaryngology—head and neck surgery. Myers, E, Krause, CJ, eds. Advances in otolaryngology—head and neck surgery; vol. 12. Mosby, St. Louis, 1998:235–261.
6. Simons, RL. Adjunctive measures in rhinoplasty. Otolaryngol Clin North Am. 1975; 8:17.
7. Crumley, RL, Lancer, R. Quantitative analysis of nasal tip projection. Laryngoscope. 1988; 2:202.
8. Baker, SR. Nasal lining flaps in contemporary reconstructive rhinoplasty. Facial Plast Surg. 1998; 14:1.
9. Baker, SR. Reconstruction of facial defects. In: Cummings CW, Fredrickson JM, Harker LA, et al, eds. Otolaryngology—head and neck surgery. 3rd ed. Philadelphia: Mosby; 1998:527.
10. Murakami, CS, Kriet, D, Ierokomos, AP. Nasal reconstruction using the inferior turbinate mucosal flap. Arch Facial Plast Surg. 1999; 1:97.
11. Burnham, HH. An anatomical investigation of blood vessels of the lateral nasal wall and their relationship to turbinates and sinuses. Laryngol Otol. 1935; 50:569.
12. Padgham, N, Vaughan-Jones, R. Cadaver studies of the anatomy of arterial supply to the inferior turbinates. J R Soc Med. 1991; 84:728.
13. Rohrich, RJ, Muzaffar, AR, Adams, WP, Jr., et al. The aesthetic unit dorsal nasal flap: rationale for avoiding a glabellar incision. Plast Reconstr Surg. 1999; 104:1289.
14. Herbert, DC. A subcutaneous pedicled cheek flap for reconstruction of alar defects. Br J Plast Surg. 1978; 31:79.
15. Robinson, JK, Burget, GC. Nasal valve malfunction resulting from resection of a cancer. Arch Otolaryngol Head Neck Surg. 1990; 116:1419.
16. Constantian, MB. The incompetent external nasal valve: pathophysiology and treatment in primary and secondary rhinoplasty. Plast Reconstr Surg. 1994; 93:919.
17. Baker, SR, Alford, EL. Mid-forehead flaps. Oper Tech Otolaryngol Head Neck Surg. 1993; 4:24.
18. Glogau, RG, Haas, AF. Skin grafts. In: Baker SR, Swanson NA, eds. Local flaps in facial reconstruction. St. Louis: Mosby; 1995:247.
19. Johnson, TM, Baker, SR, Brown, MD, et al. Utility of the subcutaneous hinge flap in nasal reconstruction. Dermatol Surg. 1994; 30:459.
20. Baker SR, ed. Principles of nasal reconstruction, 2nd ed, New York: Springer, 2011.