Reconstruction of the Lips
Introduction
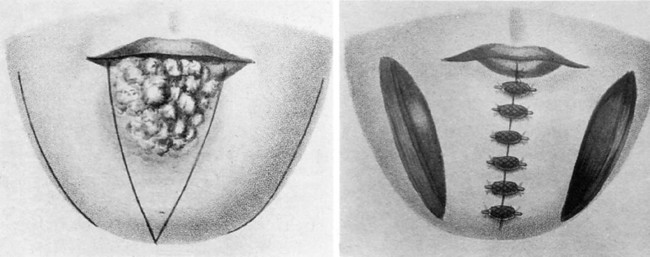
The upper and lower lips compose a distinct anatomic unit that is the principal feature of the lower face. The lips have a major importance to facial appearance and function. Reconstruction of the lip can present a challenge to the reconstructive surgeon who seeks excellence in restoration of the aesthetics and functioning of this unique structure. Descriptions of lip reconstruction date to at least BC 1000 in the Eastern Sanskrit writings of Susruta.1,2 Early reports of lip reconstruction in the Western literature date to at least the first century (Fig. 19-1). Description of the classic V-shaped excision of the lip and primary repair has been credited to a writing by Louis in 1768, although this method of treating lip neoplasms was certainly performed many centuries before that.1 A large variety of methods for reconstructing the lips were developed and reported in the medical literature of the 19th century, from which most of the procedures performed today have some derivation.
Anatomic Considerations
Lip tissue is a composite of skin, muscle, and mucosa (Fig. 19-2). The most distinguishing feature of the lip is the vermilion, which is modified mucosa that covers the free margin of the lips and is adapted for external exposure. There are relatively few glands beneath the vermilion, in contrast to the multitude of minor salivary glands found immediately deep to labial and buccal mucosa. The well-defined line where the anterior limit of the vermilion adjoins the adjacent lip skin is referred to as the mucocutaneous or anterior vermilion line. It represents an important landmark in lip reconstruction. The posterior vermilion line is defined as the innermost line of contact between the upper and lower lips when the mouth is closed. Labial vermilion is characteristically red among those of light skin color and dark among those with dark skin color. Fullness of the rounded vermilion, particularly in women, is considered a mark of beauty in many cultures.
Upper and lower labial arteries are the principal vascular supply to the lips. Both arteries are derived from the facial artery on either side of the face. The labial arteries course horizontally across the lip in the submucosal plane, immediately posterior to the orbicularis muscle at approximately the same level as the anterior vermilion line. Whereas the labial artery of the lower lip tends to remain in the same horizontal plane as it crosses the lip, that of the upper lip may rise slightly as it passes medially toward the center of the lip. Some labial arteries may have a tortuous course through the muscle. The course of the labial artery can be detected with gentle palpation and is typically easy to map out with use of a Doppler device. In studies of arterial anatomy of the lower face, a variable pattern of vessels anastomosing across the lower lip and chin was found, with one or more vertically oriented labiomental branches descending to the chin region. A horizontally oriented mental branch was noted in many cases.3,4 Multiple anastomoses between the vertical and horizontal branches were observed when both were present.3 In the central region of the upper lip, the superior labial artery gives rise to multiple septal and alar branches.3 The exact pattern for venous drainage is less well defined and has commonly been considered to be largely by venae comitantes. Superior and inferior labial veins have been described. Both veins typically drain into the ipsilateral facial vein and are less distinct than the arteries and difficult to identify. In a cadaver study, Park et al3 identified a deep venous system of the upper lip that was considered to be independent of the arterial system. An understanding of the vascular supply of the lips is important in the planning of many reconstructive lip flaps.
The limit of the superior border of the upper lip centrally is the nasal base. The limit of the inferior border of the lower lip centrally is the mental crease, which separates the lip from the chin. The lateral borders of the upper and lower lips are marked by the melolabial and labiomandibular creases that separate the lips from the cheeks. These peripheral defining lines may not be so obvious in young children, but they are more pronounced with age and are recognized natural lines of the face. The melolabial and mental creases mark the sites where muscles of facial expression attach to the orbicularis muscle, providing the muscle with an indirect connection to the facial skeleton. These crease lines are strongly favored sites for making incisions required for excision of lip tumors and for the outline of many reconstructive flaps.
The relaxed skin tension lines for the lips course in a radiant fashion about the oral stoma in a manner analogous to the spokes of a wheel and reflect the wrinkle lines of older patients (Fig. 19-3). These lines are vertical in the central region of the lips and are progressively more oblique or slanted in lateral regions of the lips. The orientation of the lines is perpendicular to the underlying orbicularis muscle fibers. The philtrum is an embryologically derived structure with two parallel raised ridges that has no functional significance but has aesthetic importance to the central region of the upper lip. Incisions of either lip create less unsightly scars when they are made parallel to the long axis of the philtrum or to the labial relaxed skin tension lines.

FIGURE 19-3 Aesthetic borders of lips marked by melolabial and labiomandibular creases on either side and mental crease inferiorly. Rhytids of lips parallel relaxed skin tension lines, which display radiant pattern about oral stoma.
The lips exhibit multiple motor functions, which include various facial expressions, oral retention of food and liquids, articulation of speech, and the acts of whistling and kissing. The lips also have important sensory functions of touch, pain, and temperature perception, which enable the monitoring of materials that enter the mouth and provide some pleasures. The most ideal lip reconstructions are those that best preserve or restore these different functions. Restoration of the orbicularis muscle sphincter is highly desirable, particularly of the lower lip. As a general rule, it is best if reconstruction of the lip is accomplished from within the lip complex, except when that would result in excessive microstomia. In most cases, reconstruction of slightly more than half of either lip can be accomplished by use of tissue from within the respective aesthetic region of the lips. When additional tissue is required, most reconstructions involve the use of local flaps harvested from the adjacent regions of the cheek or chin. With current designs, any flap harvested from outside the lip complex to repair full-thickness lip defects fails to restore a complete functional orbicularis muscle sphincter. To a limited degree, tightness in a reconstructed lip may help compensate for deficiency of the muscle sphincter.
Vermilion Reconstruction
Mucosal Advancement Flaps
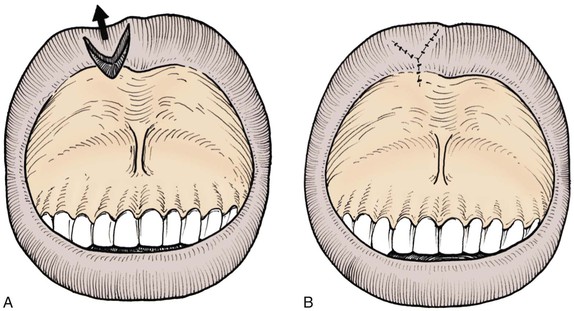
The most favored method of restoration of the vermilion is anterior advancement of the mucosa that lines the inner surface of the lip (Fig. 19-4). A mucosal flap is created by undermining beneath the labial mucosa in a plane that is deep to the minor salivary glands and superficial to the posterior surface of the orbicularis oris. If necessary, dissection may extend the entire vertical height of the lip to the apex of the gingivolabial sulcus. The flap is advanced forward over the free margin of the lip to the desired point, which is usually the anterior vermilion line. Because the vermilion is actually a modified mucosal surface, reconstruction with labial mucosa offers a close substitute. In most cases, a slight prominence of the soft tissue at the mucocutaneous junction is considered to be a favorable feature of lip contour. However, it is difficult to restore this fullness in areas reconstructed by mucosal advancement flaps. This may be related to contraction of the mucosal flap as the wound heals. There is less flap retraction when dissection of the flap requires limited undermining of the mucosa of the lip.

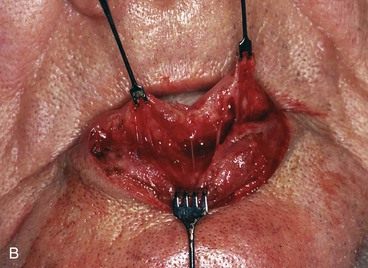
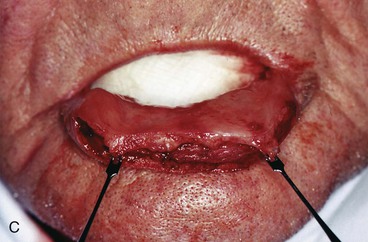

FIGURE 19-4 A, A 4 × 1-cm defect of lower lip vermilion and skin. B, Labial mucosal advancement flap dissected deep to minor salivary glands and immediately superficial to orbicularis muscle. C, Flap advanced. Margin of skin defect not dissected. Skin margin left to migrate cephalically by scar contraction. D, Anterior vermilion line in acceptable position. Continued scar maturation will reduce scar thickness.
Reconstruction of the vermilion with a mucosal advancement flap may produce a pleasing aesthetic restoration of either lip. However, several difficulties may be encountered with this technique. An early difficulty is restoration of accurate positioning of the anterior vermilion line when there is an adjacent skin defect at the lip margin. In such instances, wound contraction inherent to wound maturation may influence the position of the vermilion line. If distortion or displacement of the anterior vermilion line occurs, repositioning of the reconstructed line may be possible with revision surgery. Another difficulty encountered with mucosal advancement flaps is that the flaps tend to display a slightly deeper red color than that of the natural vermilion, especially in those with more “weathered” lips. In some cases, the darker red color can impart a slightly feminine appearance to the reconstructed vermilion, particularly when the flap covers a large surface area (Fig. 19-5).
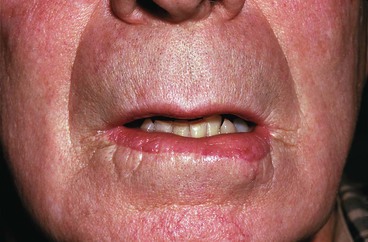
FIGURE 19-5 Mucosal advancement flap used to reconstruct inferior vermilion. Color is darker red than natural vermilion.
Whereas a majority of patients regain some degree of touch, pain, and temperature sensation to the reconstructed vermilion within a matter of several months after the employment of mucosal advancement flaps, there are individuals in whom sensory return is inadequate. Influenced by Karapandzic’s concept of lip flap design, this author performs dissections with a selective spreading technique in an attempt to preserve the small neural and vascular structures that are encountered as the mucosal advancement flap is dissected (see Fig. 19-4B).1,5,6 These neurovascular structures are then gently stretched forward with advancement of the mucosal flap.
Mucosal V-Y Island Advancement Flaps
In some cases, small volume deficiencies of the vermilion may be restored with V-Y advancement flaps of labial or buccal mucosa (Fig. 19-6). The advancement flap is created by a V-shaped incision with the apex of the incision positioned toward the gingivolabial sulcus. Mucosal V-Y advancement flaps may also be created as island flaps to repair small adjacent vermilion defects. Incisions are made to the level of the orbicularis oris, creating an island flap that is pedicled on the underlying deep tissue. The triangle-shaped island is advanced into the adjacent recipient site, maintaining sufficient deep tissue attachments to ensure its viability. The donor site is closed primarily by direct approximation of the adjacent wound margins, resulting in a Y configuration to the wound closure. Closure of the donor site assists with securing the position of the advancement flap. Most V-Y island advancement flaps of the lip are designed to advance in a vertical or near-vertical orientation. There are some cases in which horizontal tissue movement is employed, with use of either a single island flap or bilateral opposing island flaps. Mucosal V-Y island advancement flaps are best suited for repair of small defects of the vermilion.
Mucosal Cross-Lip Flaps
A vermilion defect may in some cases be restored with an interpolated cross-lip transfer of labial mucosa or vermilion along with some underlying soft tissue (Fig. 19-7). Cross-lip transfer may be accomplished with a single-pedicle flap for small defects or a bipedicle flap (“bucket handle”) for wider defects that extend horizontally across the lip (Fig. 19-8). A cross-lip mucosal flap is typically designed as a linear band of mucosa, harvested from the region immediately posterior to the posterior vermilion line of the donor lip. The width of the band is determined by the width of the vermilion defect and by what will allow donor site wound closure. The mucosal flap is most often elevated in the plane immediately superficial to the orbicularis muscle, although some muscle may be included in the flap when it is necessary to fill a soft tissue defect of the recipient lip. The labial artery may be incorporated into larger flaps, providing an axial circulation and ensuring a greater likelihood of flap viability. Once it is dissected, the flap is transferred across the oral aperture to the vermilion defect and sutured in place (Fig. 19-9). The donor site is closed primarily. Division of the pedicle and flap inset are performed 3 weeks later as a second-stage procedure.
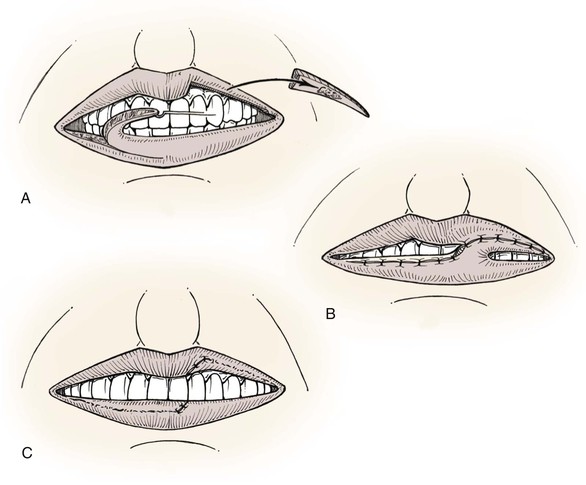
FIGURE 19-7 A, B, Interpolated cross-lip vermilion flap used to reconstruct vermilion defect of upper lip. Donor site repaired by advancing labial mucosa. C, Division of pedicle and flap inset.
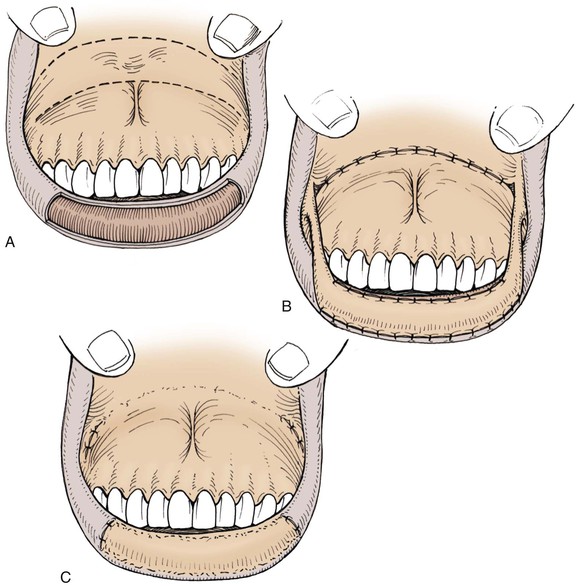
FIGURE 19-8 A, Large defect of lower lip vermilion. Broken lines indicate incisions to create interpolated bipedicle labial mucosal flap. B, Flap transferred to lower lip. Donor site repaired by labial mucosal advancement. C, Pedicles divided and flap inset.



FIGURE 19-9 A, Loss of vermilion of right lateral aesthetic unit of upper lip. B, Unipedicle interpolated cross-lip vermilion flap transferred from lower lip to upper lip. Pedicle must be adequate to accommodate repeated motion of lip during first stage. C, After vermilion cross-lip flap inset to restore vermilion and full-thickness skin graft to replace missing skin of lip.
An alternative design of a cross-lip mucosal flap that does not require an axial pattern vascular supply is a broad flap pedicled on the free margin of the donor lip that can be separated after 16 days.7 Use of this flap causes greater restriction of mouth opening while the pedicle is in place.
Tongue Flaps
Portions of the mucosal surface of the anterior tongue may be transferred to the lip to repair a vermilion defect. A mucosal flap in the form of an interpolated tongue flap is constructed for this purpose (Fig. 19-10).8,9 Mucosa transferred to the lip from the dorsal surface of the tongue will maintain the many fine filiform papillae that are characteristic of the glossal surface. Use of a tongue flap to restore the vermilion will likely create a red vermilion that can be surprisingly satisfactory. A glossal flap is usually harvested from the ventral surface of the tongue for lower lip repair and from the dorsal surface of the tongue for repair of the upper lip. It is also possible to design a flap from the lateral margin of the tongue. In nearly all cases, the pedicle is created at or near the free margin of the tongue. The leading edge of the flap is sutured to the anterior border of the vermilion defect in the best possible manner, anticipating that there will be considerable pulling with tongue movements. Attachment of the flap to the posterior border of the defect is accomplished at a second stage after division of the pedicle and flap inset. The second stage is usually performed 3 weeks after initial flap transfer. The tongue donor site wound may be closed partially or allowed to granulate while the pedicle of the flap remains attached to the recipient lip. Tongue flaps are awkward and difficult for the patient. For this reason, tongue flaps are not considered a first choice for vermilion reconstruction.
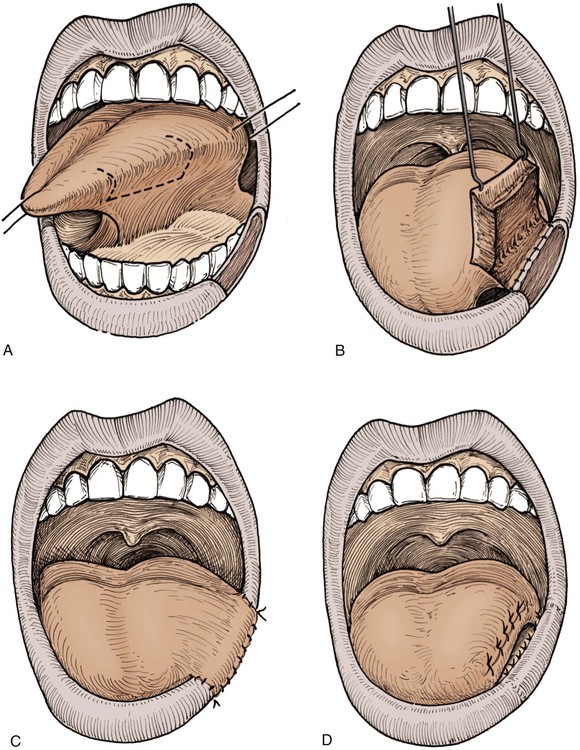
FIGURE 19-10 A, Defect of lower lip vermilion and outline of superiorly based tongue flap. B, Inferior margin of tongue donor site anchored to inner margin of lip defect. C, Tongue flap transferred to vermilion defect. D, Three weeks later, pedicle divided and flap inset, completing reconstruction of vermilion.
Vermilion Advancement Flaps
A full-thickness loss of vermilion and immediate underlying muscle may be a difficult defect to reconstruct. If the defect involves less than one-third of the width of the lip vermilion, it is possible to repair the defect by creating an advancement flap of the remaining vermilion (Fig. 19-11).2,10 A full-thickness incision is made along the anterior vermilion line inferior to the labial artery. The flap includes the vermilion portion of the orbicularis muscle. Flap dissection may require a lengthy incision to allow adequate stretch. A meticulous wound closure is necessary to minimize visible scars in this aesthetically sensitive region.
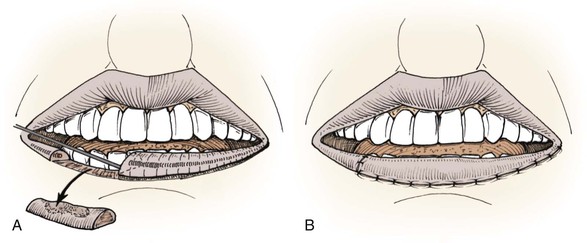
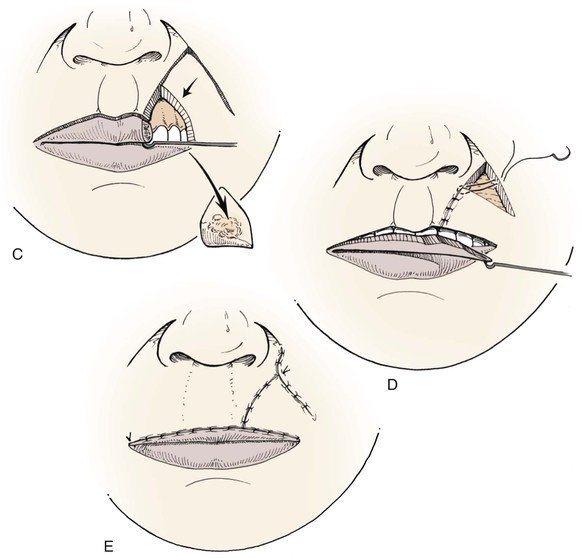
FIGURE 19-11 A, Full-thickness vermilion defect. Full-thickness vermilion advancement flap incised. Bilateral opposing vermilion advancement flaps may also be used. B, Vermilion flap advanced and wound repaired. C, Full-thickness defect of vermilion and adjacent lip. Full-thickness transposition flap and vermilion advancement flap incised. D, Flaps transferred to recipient sites. E, Two flaps in place and wounds repaired.
Cutaneous Reconstruction
The principles of cutaneous lip flap designs are similar to those applicable to other cutaneous surfaces. In reconstruction of the lip, it is preferable to confine tissue movement within the aesthetic region of the lips unless this causes excessive distortion of adjacent structures, such as the melolabial crease. Limitations are imposed on transfer of tissue within the lip complex because of the oral aperture and nasal base. In some cases of reconstruction of the cutaneous lip, it is necessary to include skin from the adjacent cheek or chin. Designing local flaps compatible with relaxed skin tension lines and borders of facial aesthetic regions can provide maximum aesthetic results.
Fusiform Repair
The preferred method for dealing with most cutaneous tumors of the lip remains fusiform excision and primary wound repair. When possible, the fusiform excision is oriented with its long axis parallel to relaxed skin tension lines of that region of the lip. From an aesthetic viewpoint, it is preferable that fusiform excisions be confined within the boundaries of the lip, avoiding extension beyond the melolabial or mental crease lines. An M-plasty at the end of the excision line may be useful in avoiding the need to extend an incision beyond the aesthetic borders of the lips or into the vermilion (Fig. 19-12). This will require closure of two small and slightly diverging incision lines near the involved end. M-plasty may also reduce tissue redundancies, particularly near the free margin of the lip.
Intralabial and Perilabial Flaps
Chin and Submandibular Transposition Flaps
Cutaneous transposition flaps may be transferred to the lips from the chin, submandibular area, or medial cheek. Flaps of the chin may be designed as a single or bilobe flap and may recruit skin from the submental region (Fig. 19-13). The chin is a distinct facial aesthetic region and a highly visible facial feature. Careful planning is important in designing a flap in this region, anticipating exactly what changes will occur in the appearance of the chin after flap transfer. Secondary procedures may be required to restore normal contours, particularly in the region of the mental crease.
Labial Rotation and Advancement Flaps
Labial cutaneous rotation and advancement flaps are used to repair skin defects of either lip. Flaps are designed to move skin medially from the area immediately lateral to the defect. Transfer of such flaps often involves moving skin around the oral commissure in a manner that employs variable degrees of rotation and advancement. The nature of the tissue movement is dependent on the exact location, size, and shape of the defect. Defects located laterally require flaps that are transferred to the recipient site with greater pivotal movement (Fig. 19-14). Defects located medially require flaps that are transferred primarily by advancement. For laterally located upper lip skin defects, rotation flaps are designed so that the lateral border of the flap is in or parallel to the melolabial crease. Flaps may extend inferiorly below the level of the oral commissure on the involved side (Fig. 19-15). Because the distance between the melolabial crease and vermilion diminishes near the oral commissure, the peripheral border of the flap is extended lateral to the crease into the cheek as necessary to achieve adequate flap width. Careful flap design is required to ensure that the width of the flap provides adequate vertical height to the reconstructed lip.
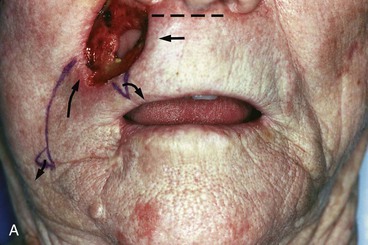


FIGURE 19-14 A, Full-thickness upper lip defect. Mucosal defect closed primarily. Majority of orbicularis muscle sphincter remained intact. Large rotation flap designed for repair. Broken line indicates additional small advancement flap from central region of lip used to lessen wound closure tension. Small curved arrows indicate excision of standing cutaneous deformity of upper lip and an equalizing Burow triangle of cheek skin. B, Wound repaired. Note elevation of right oral commissure resulting from transfer of lateral lip flap. C, One month postoperatively. Commissure in favorable position because of pull of facial musculature. Melolabial crease on surgical side is more lateral in position compared with its counterpart. Appearance of lip is relatively natural.
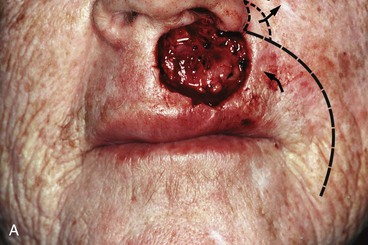


FIGURE 19-15 A, A 3 × 3-cm cutaneous defect of upper lip. Curved broken line indicates incision to create rotation advancement flap used to reconstruct defect. Triangle in alar-facial sulcus indicates excision of an equalizing Burow triangle of skin. B, Flap in place. C, One year postoperatively. No revision surgery performed. Care is taken with this surgical approach to minimize distortion of philtrum and nasal base.
Dissection of labial rotation and advancement flaps is in the subcutaneous tissue plane superficial to the level of the orbicularis and facial muscles. For rotation flaps, a longer wound border is expected in the cheek lateral to the flap. This disparity in wound length can usually be accommodated by equally dividing the skin redundancy during wound closure. If necessary, a small equalizing Burow triangle of skin is excised from the cheek opposite the most inferior portion of the flap or in the alar-facial sulcus.11
Cutaneous lip rotation flaps are most frequently employed to repair defects involving the more lateral portion of lip skin (see Fig. 19-14). In contrast, advancement flaps are most commonly used to repair centrally located cutaneous defects. As the flap is advanced medially, its base often overlaps the oral commissure. This redundancy of skin at the commissure may require excision. In more extreme cases, the oral commissure may be pulled superiorly or inferiorly with medial advancement of the flap. This may be self-correcting as the natural pulling of the lip musculature causes a corrective adjustment over time (see Figs. 19-14 and 19-15).
Melolabial Flaps
Melolabial cutaneous transposition flaps may be designed with a pedicle that is either superiorly or inferiorly based. A flap with a superiorly based pedicle is commonly used to reconstruct defects of the central upper lip. A flap with an inferiorly based pedicle is often used to reconstruct defects involving more lateral portions of the upper or lower lip. Use of melolabial flaps to repair the lips incurs some degree of flattening of the melolabial folds. Flaps with a superiorly based pedicle produce the greatest degree of distortion of the melolabial fold as they extend across the most defined and visible portion of the fold. A second surgical stage involving revision of the pedicle to align scars parallel to the melolabial crease is frequently indicated in cases in which a melolabial transposition flap is used to reconstruct the upper lip.
Distortion of the melolabial fold and crease, alteration in the orientation of facial hair growth pattern, and tendency toward development of trap-door deformity are reasons that melolabial cutaneous transposition flaps are not frequently used to repair skin defects of the lips. Cutaneous defects in the central portion of the lip are often best reconstructed with bilateral advancement flaps. Larger (≥2 cm) central defects usually are converted to full-thickness defects and closed primarily (Fig. 19-16). Similar to centrally located defects, small laterally located cutaneous defects of the lip can be closed with bilateral advancement flaps, often in the form of an A-T plasty (Fig. 19-17). Larger (≥2 cm) laterally located cutaneous defects of the upper lip are effectively reconstructed with V-Y subcutaneous tissue pedicled melolabial advancement island flaps (see Chapter 12) (Fig. 19-18). The flap is freed from its orbicularis muscle attachments near the commissure and is based solely on the abundant subcutaneous fat located just lateral to the commissure. This is only when the flap is sufficiently large to necessitate the incorporation of skin of the melolabial fold into the flap.

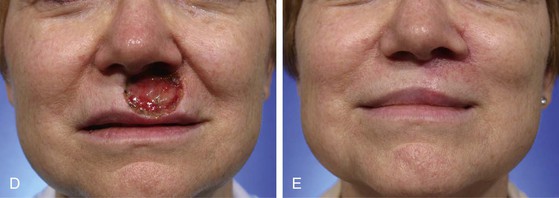
FIGURE 19-16 A, A 2 × 2-cm skin defect of upper lip. B, C, Defect converted to full thickness, sparing most of the exposed muscle, and wound closed primarily. D, E, Preoperative and 1-year postoperative views. No revision surgery performed. (Courtesy of Shan R. Baker, MD.)
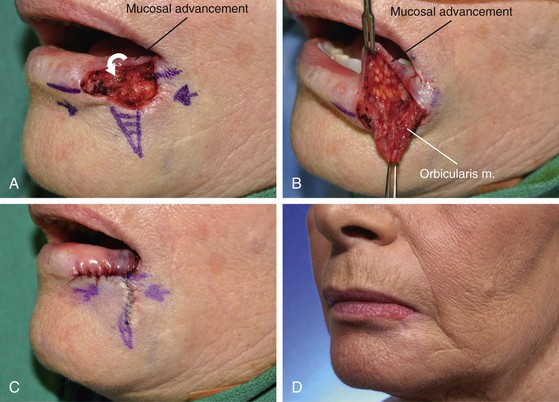
FIGURE 19-17 A-C, A 1 × 1.5-cm skin and vermilion defect. Bilateral advancement flaps (A-T plasty) designed to repair cutaneous component of defect. Mucosa advanced to reconstruct vermilion (arrow). D, Postoperative result at 10 months. No revision surgery performed. (Courtesy of Shan R. Baker, MD.)
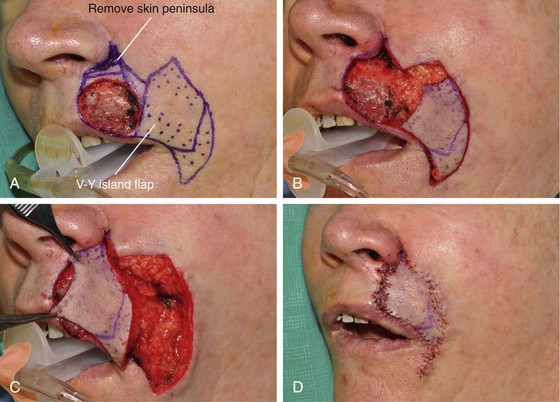

FIGURE 19-18 A, A 2 × 2.1-cm skin and vermilion defect of lip. V-Y subcutaneous tissue pedicled lip advancement island flap designed for repair. Flap designed to recruit medial cheek skin. Non-stippled area represents subcutaneous vascular pedicle on which flap is based. Peninsula of skin in alar-facial sulcus replaced with flap to maximize scar camouflage. B, In situ flap incised. C, D, Flap advanced to recipient site. E-G, Preoperative and 5-month postoperative views. No revision surgery performed. (Courtesy of Shan R. Baker, MD.)
For sizable (2-3 cm) lip skin defects adjacent to the inferior border of the ala, it may be beneficial to excise the small peninsula of skin between the ala and melolabial fold in the process of enlarging the defect so that the defect extends to an aesthetic boundary.8 The peninsula is then reconstructed by appropriately designing the island flap so that the superior portion of the flap replaces the peninsula (Figs. 19-18 and 19-19). This technique provides the best camouflage because the superior border of the flap is positioned within the aesthetic boundaries of the alar-facial sulcus and melolabial crease. When this peninsula is not replaced, the flap must cross the base of the peninsula and may mar an otherwise excellent result.
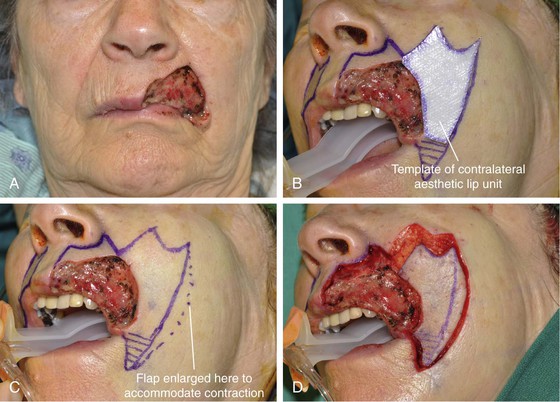

FIGURE 19-19 A, A 3.8 × 2.8-cm defect of skin, vermilion, and muscle of lip. B, Excision of remaining skin of lateral aesthetic unit planned. Template of contralateral aesthetic lip unit used to design V-Y subcutaneous tissue pedicled melolabial rotation advancement island flap. C, Flap width enlarged 1 cm to accommodate scar contracture and subsequent diminution of vertical height of reconstructed lip. D-F, Flap transferred to recipient site. Labial mucosa advanced outward to reconstruct vermilion. G, H, Eight months after reconstruction and 2 months after contouring of flap and Z-plasty scar revision. (Courtesy of Shan R. Baker, MD.)
The major advantage of subcutaneous tissue pedicled melolabial advancement flaps used to repair sizable cutaneous defects of the upper lip is that there is no need to resect standing cutaneous deformities because these do not develop with this flap. For this reason, they are particularly advantageous compared with transposition and cutaneous pedicled advancement flaps, which often have sizable deformities that must be resected and discarded. There is no wasted skin with the island flap. Another important advantage of the island flap is that there is considerably less dead space beneath the flap as well as beneath skin surrounding the donor defect compared with use of cutaneous pedicled flaps. Less dead space means less space available for collection of blood and serum. Therefore, there is less risk for development of a hematoma compared with use of other types of flaps.
Full-Thickness Reconstructions
Primary Repair
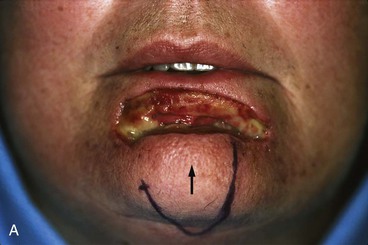
Primary repair of either lip provides satisfactory results for full-thickness defects of as much as one-third the width of the lip. Wedge or V-shaped full-thickness lip excision and primary wound closure have long been the most common method of treatment of most malignant neoplasms of the lip (see Fig. 19-20). Closure of the V-shaped defect is oriented parallel to relaxed skin tension lines of the lip. In the central portion of the lip, the V-shaped excision is oriented vertically, with equal length given to the two borders of the V (Fig. 19-20). In more lateral regions of the lip, the V is skewed to produce a more angulated wound closure line matching the natural relaxed skin tension lines of the lateral lip (Fig. 19-21).


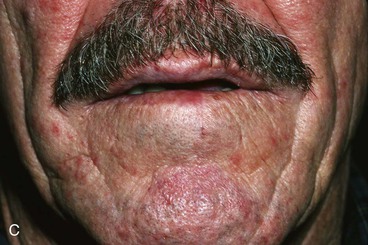
FIGURE 19-20 A, Lip marked for V-shaped full-thickness excision of lip malignant neoplasm. B, Immediately after excision and multilayer wound repair. C, Postoperative result at 6 months. Scar is flat, and notching of vermilion border is not observed.

FIGURE 19-21 Lip marked for V-shaped excision. V is skewed to accommodate slanted relaxed skin tension lines in lateral region of lip.
Optimal primary repair of full-thickness lip defects requires approximation of at least four tissue layers: mucosa, muscle, subcutaneous tissue including deep dermis, and epithelium of the skin. The tendency toward development of a retracted and depressed lip scar is appreciably reduced when the wound is repaired with accurate approximation of the lip muscle. Precise approximation of the subcutaneous tissue layer is accomplished with sutures that are adjacent to or include the deep portion of the reticular dermis. The epithelium of the skin is closed in a manner that ensures a slight eversion of the skin edges. Attention to detail throughout wound closure will achieve an optimal scar that is narrow and flush with adjacent lip tissue.
A W-shaped excision is another way of achieving greater resection of lip tissue without extending the apex of the excision beyond the mental or melolabial crease (Fig. 19-22). The apexes of the three points of the W usually remain within the confines of the lip aesthetic region. When the points must extend beyond the aesthetic region of the lip, consideration is given to placing the apex of the central point of the W at the mental or melolabial crease, depending on the location of the excision. This design provides a natural break between the single vertical scar line of the lip and the diverging distal scar lines required for closure of the more peripheral wound (see Fig. 19-22). In some situations, designing the two angles of the W with dissimilar sizes can achieve a more natural appearing scar, particularly for excision of tumors of the lateral lip. W-shaped excisions of lateral portions of the lip are best accomplished by designing a smaller angle of the W medially and a larger angle laterally (Fig. 19-23).
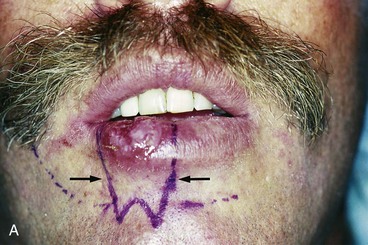

FIGURE 19-22 A, Lip marked for W-shaped full-thickness excision of lip malignant neoplasm. Tip of central angle of W positioned at mental crease. Broken lines indicate alternative plan for repair with bilateral advancement flaps. B, Primary wound closure of full-thickness W-shaped lip excision. Untied suture placed at anterior vermilion line as reference for aligning lip repair.


FIGURE 19-23 A, Atrophy of lower lip from radiotherapy in childhood for hemangioma of lip. Persistent hemangioma is present. Lip marked for W-shaped excision. W has angles of different sizes for scar to parallel relaxed skin tension lines of lateral lip. B, Postoperative result at 6 months. Slight asymmetry of lower lip present.
Bilateral Lip Advancement Flaps
Reconstruction of rectangular full-thickness defects of either lip may be achieved with bilateral advancements of the remaining lip segments (Figs. 19-24 and 19-25). Bilateral advancement flaps of the lower lip are created with release of the remaining lip segments by incisions along the mental crease. Incisions are curved gently downward at each end of the crease to follow the superior margin of the aesthetic border of the chin. Incisions may be full thickness or partial thickness as required by the situation. Although it is not necessary, dissection through the subcutaneous tissue and muscle layer of the flaps may be performed in the fashion described by Karapandzic, which attempts to preserve neural and vascular structures to offer optimal preservation of sensory function and tissue vascularity (see later section on Karapandzic flaps).1,5,6 Because of the elasticity of mucosa, the mucosal portion of full-thickness incisions is not carried as far laterally as that of the skin and muscle. Approximation of the two flaps is accomplished in a fashion similar to that described for full-thickness primary lip repair. For full-thickness defects of the lower lip repaired with bilateral advancement flaps, accommodation is made for tissue redundancy along the superior margin of the chin as the lip flaps are advanced. This is accomplished by performing bilateral excisions of equalizing Burow triangles of skin from the chin side of the incision.1,11,12


FIGURE 19-24 A, Full-thickness rectangular excision of central lower lip. Bilateral opposing advancement flaps designed for repair. Flaps created by single opposing incisions marked in mental crease. B, Flaps apposed and wound closure in progress. Such wounds can frequently be repaired with limited releasing incisions along mental crease.
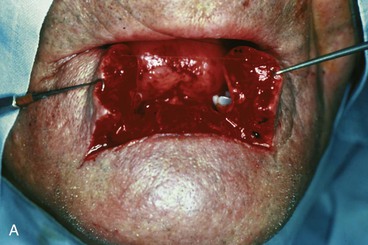

FIGURE 19-25 A, Bilateral labial flaps created by full-thickness incisions along mental crease after full-thickness excision of central lip. The author prefers to dissect deeper layers by Karapandzic type of dissection to preserve as much lip sensory function as possible.5,6 B, Postoperative result at 5 years. Patient exhibited excellent lip function.
A variation for designing bilateral advancement flaps to repair full-thickness defects of the lower lip advocated by Isaksson and Johanson uses a stair-step design (Fig. 19-26).13,14 The lip tumor is removed by a rectangular excision. To create the advancement flaps, a series of bilateral square or rectangular incisions are made that connect in a downward diagonal fashion following the aesthetic border of the chin. At the termination of the incisions, bilateral small triangles of skin are excised. As the lip segments are advanced for wound closure, the series of rectangles and terminal triangles are closed, creating a stair-step wound closure line that is intended to minimize the effects of scar contracture. Although this is a functional and novel method of repair, it creates a scar that is not as natural to the lower face as one placed directly in the mental crease.
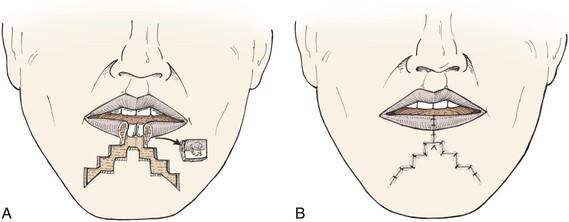
FIGURE 19-26 A, Rectangular excision of central lower lip. Bilateral full-thickness opposing stair-step advancement flaps used for reconstruction. B, Wound closure has stair-step configuration.
Bilateral advancement flaps may also be used for reconstruction of full-thickness defects of the upper lip. To facilitate medial advancement of lip tissue, excision of crescent-shaped segments of skin from the cheek in the region immediately lateral to the nasal alae is usually required (Figs. 19-27 and 19-28). The perialar crescent excisions are of skin only, with care taken to minimize disruption of sensory nerve fibers to the upper lip. For centrally located upper lip defects, advancement flaps do not provide restoration of the philtrum. A vague semblance of the philtrum is provided by the central vertically oriented scar. Lack of an actual philtrum tends to be less obvious in older patients.
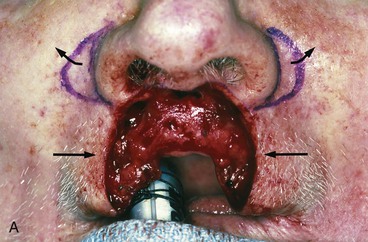



FIGURE 19-27 A, Full-thickness tissue loss of central upper lip. Advancement of remaining lip segments is planned. Anticipated bilateral standing cutaneous deformities resulting from advancement of lip segments marked for excision in alar-facial sulci. Excision of deformities facilitates advancement of flaps. B, Deformities excised, with care taken to preserve larger neural and vascular structures. C, Flaps advanced and wound repaired. D, Postoperative result at 6 months. In this case, lack of philtrum does not cause marked deformity.

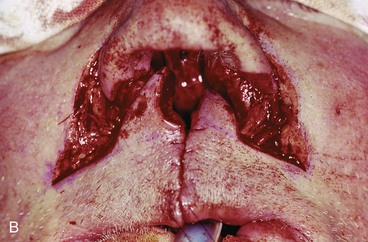

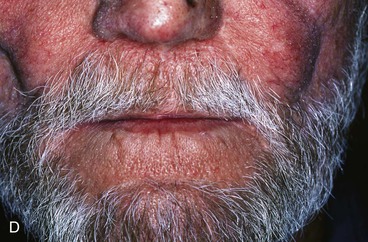
FIGURE 19-28 A, Full-thickness defect of central lip and columella. Bilateral opposing advancement lip flaps marked for repair. Anticipated standing cutaneous deformities resulting from advancement marked in alar-facial sulci. B, Lip flaps apposed in midline. Crescent-shaped deformities preserved and transferred with flap to assist with repair of anterior floor of nose. C, Flaps sutured in place. Some exposed surfaces within nasal passage left to heal by secondary intention. D, Postoperative result at 2 years. No revision surgery performed.
Circumoral Full-Thickness Rotation Advancement Flaps
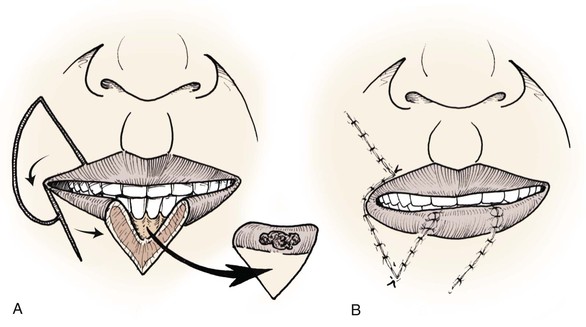
Full-thickness composite lip flaps can be transferred around the oral commissure as either single or bilateral opposing flaps. This method of reconstruction, first described in 1857 by von Bruns, is intended to restore a complete and functional muscle sphincter (Fig. 19-29).1,15 Flap movement employs both rotation and advancement as the flap is transferred around the oral commissure to close the defect. This method of reconstruction is more commonly employed for reconstruction of full-thickness defects of the lower lip but may be reversed for upper lip repair as well. Flaps are designed to optimize preservation and function of the remaining orbicularis muscle.
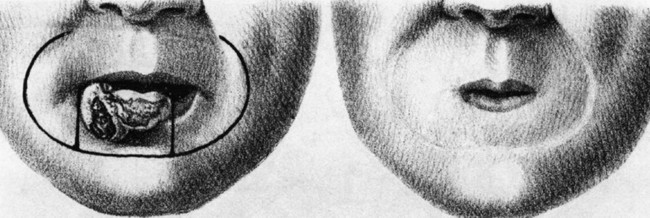
FIGURE 19-29 Reconstruction of lip with full-thickness circumoral rotation advancement flaps, as originally described by von Bruns in 1857. (From von Bruns V: Chirurgischer Atlas: Bildliche Darstellung der chirurgischen Krankheiten und der zu ihrer Heilung erforderlichen Instrumente, Bandagen, und Operationen, II Abt, Kau- und Geschmaks-Organ, Tubingen,1857/1860, Laupp.)
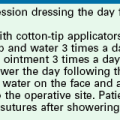
Karapandzic Flaps
A significant modification of the full-thickness circumoral composite rotation advancement lip flap was described by Karapandzic in 1974. This modification preserves most of the neural and vascular structures entering the flap (Fig. 19-30).1,5,6 The technique typically involves the creation of bilateral opposing flaps that may be of different lengths, depending on the circumstances. Unique to the Karapandzic technique is making incisions for the flaps that are not full thickness. Incisions are made through the skin of the flaps and separate incisions through the mucosa on the deep surface of the flaps. Dissection of the flaps is performed with an attempt to identify and to preserve as many neural and vascular structures as possible. Separation of the subcutaneous tissue and muscle of the flaps from the adjacent facial tissues is performed bluntly with scissors to gently spread the tissue apart to avoid cutting through any neural or vascular structures unless necessary (see Fig. 19-30B). Neural and vascular structures are dissected sufficiently to allow them to be stretched and carried along with the transfer of the flaps without the need to cut the structures. This approach maximizes vascular supply and preserves optimal motor and sensory function to the reconstructed lip, minimizing the need for reinnervation.

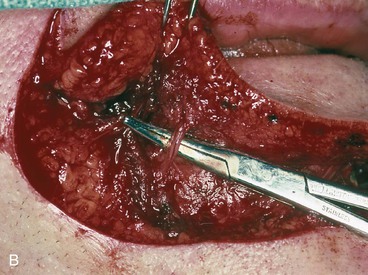
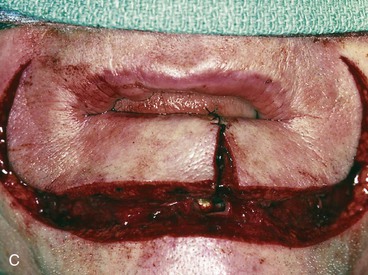

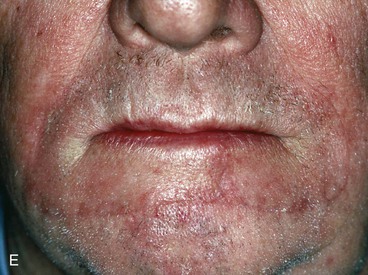

FIGURE 19-30 A, Full-thickness defect of lower lip. Bilateral Karapandzic flaps incised. B, Demonstration of vessels preserved with Karapandzic technique of dissection. Compared with central lip, identification of peripheral margin of orbicularis muscle in vicinity of commissures is more difficult. Release of facial muscle attachments to orbicularis muscle may be performed lateral to actual peripheral margin of orbicularis muscle near commissures to ensure consistency of thickness of muscle layer of flaps. C, Flaps approximated. D, For proper lip height, flaps are designed with uniform width throughout length of flaps. For this reason, it is necessary to design flaps lateral to melolabial crease near commissure. E, Postoperative result at 6 months. F, Postoperative result at 1 year. Reconstructed lip has tightened from scar contraction. Such long-term changes are common.
An incision to create a Karapandzic flap is made parallel to the free margin of the lips, creating a flap with a uniform width throughout. To optimize aesthetic results in reconstruction of the lower lip, an incision is made along the course of the mental crease as far as possible and then carried around the oral commissure and into the melolabial crease (Fig. 19-31). Flap design is modified but is similar for reconstruction of upper lip defects (Fig. 19-32). Bilateral flaps are designed so that their width remains nearly uniform, with a tolerance for variation that is only gradual when attempts are made to accommodate the natural facial features at the periphery of the flaps.


FIGURE 19-31 A, Lip cancer marked for excision. Reconstruction planned with bilateral Karapandzic flaps. Outline of flaps is marked in mental crease as far laterally as possible and then transitions into melolabial creases. B, Cancer excised and flaps apposed.



FIGURE 19-32 A, Bilateral Karapandzic flaps marked for reconstruction of central upper lip deficiency. B, Flaps apposed. C, Patient experienced difficulty in passing oversize denture through oral stoma required to obturate palatal defect after reconstruction. Mouth expanded during interval of several weeks with graduated lip-stretching device. Soft tissue deficiency in superior region of upper lip subsequently reconstructed with melolabial transposition flap.
A helpful feature in restoration of central full-thickness defects of either lip is to design bilateral flaps of similar size (mirror image), which ensures symmetry. In reconstruction of the lateral portion of the lower lip, bilateral flaps are commonly designed of different lengths, with a preference to create longer flaps from the contralateral lower lip (Fig. 19-33). This approach may avoid distortion of the central region of the upper lip.






FIGURE 19-33 A, Malignant neoplasm of left lower lip. B, Same patient shown in A with full-thickness defect of half of lower lip after excision of cancer. Defect involves commissure. Bilateral Karapandzic flaps of unequal length designed for reconstruction. C, D, Flaps of unequal length have been dissected. Lower lip flap provides majority of tissue for restoration of defect. Anterior vermilion line approximated first. E, Lip anastomosis performed before reattachment of surrounding facial musculature in anatomically correct orientation. F, Postoperative result at 6 months. Small oral stoma acceptable. Accommodation for dentures is an important consideration in selection of this method of repair.
For repair of centrally located lower lip defects, bilateral flaps are created by making incisions from the defect that extend laterally and superiorly around the oral commissure into the melolabial creases. The incisions typically end at the level of the nasal alae. This provides composite flaps that offer symmetry with respect to the nasal base and the reconstructed oral stoma. Once the flaps have been dissected, it is best to first secure together the two opposing borders and then to adjust the remaining wound closure to the surrounding facial tissues (see Fig. 19-33E). Care is taken to reattach the various muscles of facial expression to the orbicularis muscle in anatomically appropriate orientation and location, although to a large extent this occurs naturally as the wound margins heal. Failure to perform a meticulous layered wound closure can result in a scar that has a “clown-like” appearance as it encircles the lips. Some degree of distortion of the oral commissure is inevitable, causing the commissures to be more rounded. In the majority of cases, the position of the commissure is unchanged but the shape is blunted and pulled slightly in the direction of flap transfer. Bilateral commissure distortion tends to be less apparent than unilateral distortion.
In some patients, the Karapandzic technique may be used to repair a defect as large as two-thirds of the width of either lip (Fig. 19-34). However, there is variability among patients as to how well lip tissue will stretch without excessive distortion of the commissures or creation of limiting microstomia. Lip tissue of older patients is more redundant and tolerant to stretching. A smaller mouth opening may not be acceptable for patients who wear dentures and must be able to pass dentures in and out of the mouth with relative ease. However, the oral aperture can be made larger over time with persistent stretching of the lips by either repeated manual manipulation or insertion of an adjustable lip-stretching mouth appliance.
Transoral Cross-Lip Flaps
Abbe (Sabattini) Flap
Sabattini appears to have been the first to describe cross-lip transfer of full-thickness lip tissue in 1838.1,16 By the turn of the 19th century, several modifications of design of cross-lip flaps had been reported.1,17–19 Flap design described by Sabattini and later by Abbe in 1898 involved transfer of a triangular full-thickness segment of lip tissue from the lower lip to a full-thickness upper lip defect. The flap was designed slightly smaller in width compared with the defect (Fig. 19-35).16,19 More often, there is need to transfer a flap from the upper lip to reconstruct a defect of the lower lip, where cancer occurs with greater frequency. The labial artery is preserved on one side to serve as the pedicle of the interpolated flap (Fig. 19-36). Venous drainage of the flap is provided by small veins that approximately parallel the course of the artery. The flap is pivoted nearly 180° on its pedicle as it is inserted into the opposing lip defect and sutured into place. The flap donor site is closed primarily. In approximately 3 weeks, the pedicle is divided and the flap inset. While the pedicle is in place, patients may take an oral diet best limited to liquids and soft foods that require minimal biting and chewing.
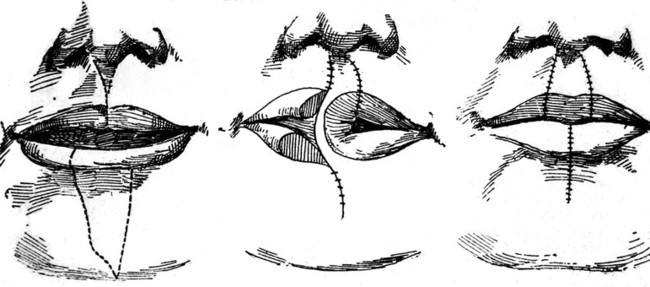
FIGURE 19-35 Illustration of cross-lip flap reconstruction as reported by Abbe. (From Abbe R: A new plastic operation for the relief of deformity due to double harelip. Med Rec 53:477, 1898.)

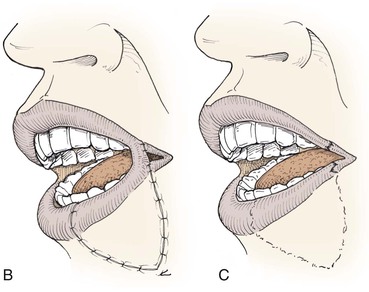
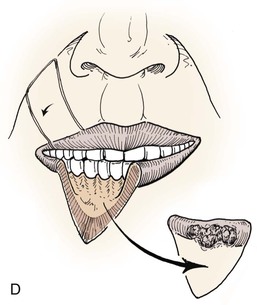
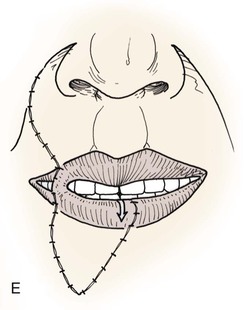
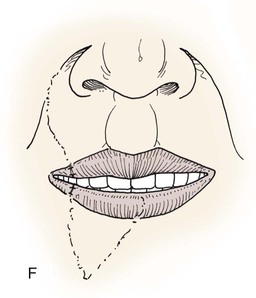
FIGURE 19-36 A, Incised Abbe flap pedicled medially on upper lip. B, Cross-lip flap at end of first stage. Donor site closure not illustrated. C, Pedicle divided and flap inset at second stage. D, E, Cross-lip flap used to repair right lower lip defect. Vermilion of flap advanced to match width of vermilion at recipient site. F, Division of pedicle and flap inset.
After study of the complex vascular distribution of the lower lip and chin, Kriet et al4 described the design and use of an extended cross-lip flap that included a portion of tissue from the chin to repair a large defect of the upper lip and adjacent cheek (Fig. 19-37). More standard cross-lip flaps may be designed with variations of V, W, rectangular, or other configurations, depending on the particular requirements of a given reconstructive situation (Fig. 19-38).20–22 Similar to the orientation of V-shaped and W-shaped full-thickness lip excisions that are closed primarily, cross-lip flaps are designed so that their axes parallel relaxed skin tension lines. The size of cross-lip flaps may vary from one that is the size of a given defect to one that fills only a small portion of the defect. In this circumstance, a greater concomitant advancement of lip segments on either side of the defect is required. Likewise, when there is a major tissue loss, a cross-lip flap can in some cases be combined with unilateral or bilateral horizontally oriented advancement flaps to collectively achieve lip reconstruction. On occasion, a second flap in addition to the cross-lip flap is employed. In most cases, the height of the cross-lip flap is designed to match that of the recipient site. The size of the two lips remains proportionally similar if the width of the flap is designed to be half the width of the defect. For upper lip defects of an entire aesthetic unit, such as the philtrum or lateral aesthetic unit, consideration is given to transfer of a flap from the lower lip that is the same size as the defect so that the flap will restore the complete aesthetic unit of the lip.22
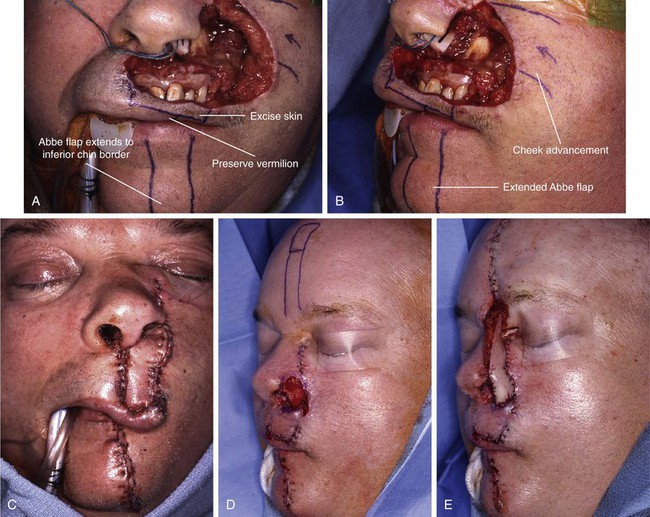

FIGURE 19-37 A, B, Large full-thickness defect of lip and ala with extension to medial cheek. Extended Abbe flap designed for repair of lip defect. Cheek advancement flap designed for repair of cheek component of defect. C, Flaps in place. Extended Abbe flap used to line anterior floor of nose. Vermilion of left upper lip preserved. D, E, Abbe flap inset. Ala reconstructed with mucoperichondrial flap hinged on caudal septum, auricular cartilage framework graft, and interpolated paramedian forehead flap. F-I, Preoperative and 1-year postoperative views. Upper and lower lip scars revised 6 months after inset of paramedian forehead flap. (Courtesy of Shan R. Baker, MD.)

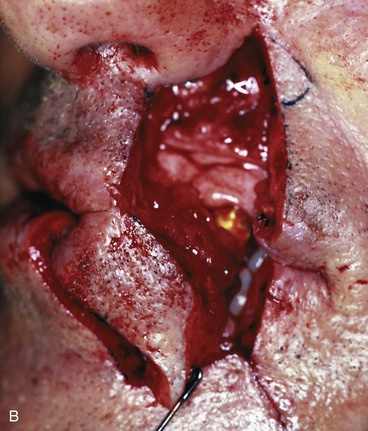


FIGURE 19-38 A, Full-thickness W-shaped excision of lower lip. Cross-lip flap designed for reconstruction. Perialar skin included in flap design will lengthen flap, transfer larger skin surface area to recipient site, and facilitate donor site closure. B, Medial pedicled flap transferred to recipient site. C, Flap in place. Donor site closed. D, Several months after pedicle division and flap inset. Flap displays trap-door deformity.
Cross-lip flaps may be pedicled medially or laterally, except when the defect involves the more lateral portion of the lip. For extreme laterally located defects, the flap is based medially. In all other circumstances, a decision pertaining to the location of the pedicle is influenced by which side will allow an easier flap transfer and inset with respect to the oral commissure. The labial artery courses between the labial mucosa and orbicularis oris muscle, just deep to the posterior vermilion line. It has a tendency to lie slightly higher in the central region of the upper lip, making a lateral pedicle slightly safer to use when the flap is harvested from the upper lip.
The cross-lip flap pedicle necessarily includes the labial artery and a small cuff of surrounding tissue at the free margin of the lip. A tradeoff is made between having sufficient soft tissue in the pedicle to ensure adequate venous drainage and having a more bulky pedicle that causes greater difficulty in accurately approximating the flap donor site on the pedicled side (Fig. 19-39). The labial artery lies posterior to the orbicularis muscle, so the skin incision used to create the flap may extend a limited distance through the anterior portion of the vermilion if necessary for optimal transfer of the flap to the recipient lip.






FIGURE 19-39 A, Abbe flap designed for repair of defect. B, Flap incised. C, Flap turned upward based on narrow pedicle consisting of vermilion muscle. D, Preoperative view. Full-thickness defect of central lip after resection of lip cancer. E, One week after flap transfer. F, Six months after flap inset. No revision surgery performed. (Courtesy of Shan R. Baker, MD.)
Cross-lip flap reconstruction involves transfer of full-thickness lip tissue, so there is restoration of the orbicularis oris sphincter (Fig. 19-40). The first signs of motor reinnervation begin to appear a few months after flap transfer and are demonstrated by irregular, single, low-amplitude motor unit potentials. Studies by Smith23 and Thompson and Pollard24 show that single and polyphasic motor unit potentials are detected with voluntary effort, develop greater amplitude, and appear increasingly normal during the first year after transfer of cross-lip flaps (Figs. 19-41 and 19-42). The quality of muscle movement that returns to cross-lip flap tissue is variable. Many patients eventually display adequate motor function within the flap tissue; others demonstrate some degree of persistent motor weakness. This may result in some deficiency of oral continence, particularly with liquids. Problems with oral continence appear to be more likely in patients of advanced age and in patients who are edentulous.
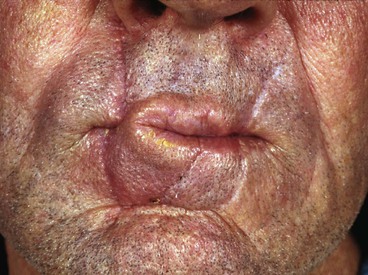
FIGURE 19-40 Cross-lip flap with wide pedicle. Labial artery is located immediately deep to posterior vermilion line, so incision to create flap may extend through anterior portion of vermilion.


FIGURE 19-41 A, Lips in repose 1 year after cross-lip flap reconstruction of lower lip. B, Pursing of lips activates contraction of muscle within flap tissue.

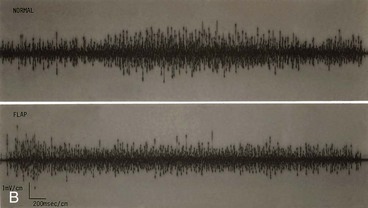
FIGURE 19-42 A, Patient undergoing electromyographic analysis 5 years after cross-lip flap reconstruction of lower lip. B, Electromyography recording comparing motor activity in region of lip that was not operated on (top) with activity found within cross-lip flap (bottom).
Cross-lip flaps sustain at least temporary loss of sensation as they are dissected and transferred. A partial return of sensory function is typically first observed several months after flap transfer. Sensory function returns in the order of pain, touch, and temperature (cold, then hot). In studies of denervated cross-lip flaps by Smith,23 return of pain sensation could be detected 2 months after flap transfer, followed by tactile sensation at 3 months, cold at 6 months, and warmth at 9 months. Smith determined that by 1 year after flap transfer, pain, touch, and sweating of the flap are nearly normal, whereas temperature detection tends to remain slightly impaired.23 This author has observed that some patients may notice a slight dysesthesia or hypersensitivity of the flap to stimuli such as cold during the first year or two after reconstruction. However, this phenomenon appears to dissipate over time.
There is a strong tendency for cross-lip flaps to appear thickened, even after many years, resulting in a trap-door deformity (Fig. 19-43). The flap may appear thin and well matched to the adjacent lip tissue when it is stretched in activities such as smiling but then appears excessively thick when relaxed. Unfortunately, the scar that surrounds a cross-lip flap cannot completely match the elasticity of natural lip tissue and is the likely cause of the thickened appearance of the flap. The scar is full thickness and completely encircles the flap except along the free margin of the lip. Lymphatic drainage from cross-lip flaps is restricted because of the scar. An additional factor that may contribute to trap-door deformity of the flap may be related to wound closure techniques. If all tissue layers and particularly the muscle layer are not carefully approximated, there is a greater tendency for scar contraction, resulting in a depressed scar about the borders of the flap that enhances trap-door deformity.


FIGURE 19-43 A, Same patient shown in Figure 19-38D 1 year after cross-lip flap reconstruction of lower lip. Scar lines are ideal, and there is minimal trap-door deformity. B, Same patient 5 years later. Recipient lip has “aged.” Scars are more apparent, and flap displays greater trap-door deformity.
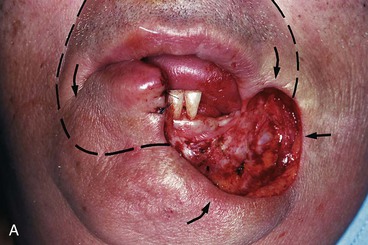
Estlander Flap
In 1872, Estlander was first to describe a cross-lip flap repair that involved transfer of a full-thickness lip flap with a pedicle that was incorporated into the reconstructed ipsilateral oral commissure (Fig. 19-44).1,25 Similar to other cross-lip flaps, the Estlander flap is typically designed to harvest tissue from the opposing lip to help restore approximately half or more of a given lip defect. The flap is transposed around the oral commissure on a small vascular pedicle containing the labial artery. The Estlander cross-lip flap is performed as a one-stage reconstruction (Fig. 19-45). The Estlander cross-lip flap is suited for repair only of a defect involving the lateral portion of either lip. Baker26,27 has suggested a modification of the design of superiorly based Estlander flaps that places the donor site scar within the melolabial crease (Fig. 19-46). The greatest disadvantage of this flap is that it creates fullness or blunting of the involved oral commissure. Whereas this deformity may not be readily seen when the lips are closed, it is often obvious when the mouth is held open and the two commissures are seen simultaneously (Fig. 19-47). Several techniques are described for a second-stage revision of the distorted oral commissure; however, none appears to completely restore a natural appearance (see section on commissureplasty).
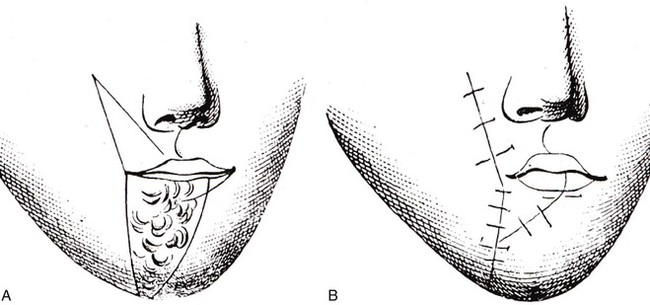
FIGURE 19-44 A, B, Original illustrations. (From Estlander JA: Eine Methode aus der einen Lippe Substanzverluste der anderen zu ersetzen. Arch Klin Chir 14:622, 1872.)


FIGURE 19-45 A, Estlander cross-lip flap attached to donor lip by pedicle. B, Flap secured in recipient site.
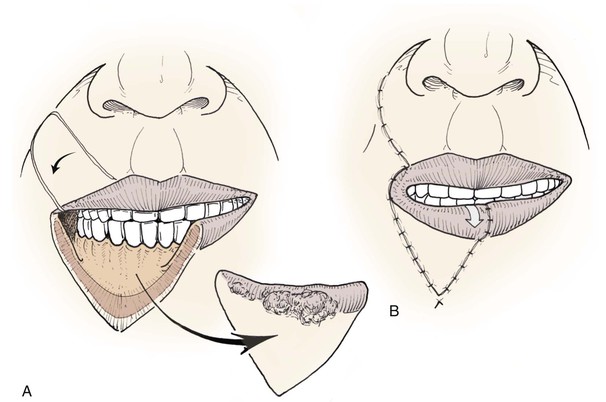
FIGURE 19-46 A, Estlander cross-lip flap with rounded apex for donor site scar to lie in melolabial crease. B, Vermilion of flap advanced anteriorly to match width of recipient lip vermilion.



FIGURE 19-47 A, Traumatic partial avulsion of upper lip and cheek soft tissue. B, C, Wound repaired. Lateral portion of right upper lip necrosed, resulting in scarring and destruction of commissure. D-G, Loss of lateral lip segment reconstructed with Estlander flap. H-K, Six months after Estlander flap, commissureplasty performed. L, M, Six months after commissureplasty, Z-plasties and additional refinement of commissure performed. N, O, Six months after Z-plasties. (Courtesy of Shan R. Baker, MD.)
Double Lip Flap Repair
Several authors have described cross-lip transfer with two flaps to repair a large defect of the opposing lip. In 1848, Stein first described the simultaneous use of small bilateral laterally based cross-lip flaps harvested from the philtrum and used to reconstruct a large defect of the central lower lip.17 Although it is clearly more complicated to work with two flaps and their pedicles, this design maintained symmetry within the donor lip. Kazanjian later modified Stein’s design to preserve the central philtrum by harvesting flaps from either side of the philtrum.28 In most situations, preference is given to use of a single flap to limit the number of scars and anastomotic connections of lip segments. Martin29 in 1932 and Murray30 in 1972 reported on the use of large bilateral Estlander flaps to reconstruct full-thickness defects of the entire lower lip. Despite the consequent reduction in size of the oral stoma, both authors reported that lip symmetry and function were satisfactory and acceptable, considering the magnitude of such reconstruction.
In 1876, Buck described a two-flap reconstruction involving one cross-lip flap and one transposition flap to reconstruct a full-thickness defect of the central region of the lower lip (Fig. 19-48).18 The transposition flap moved the remaining lip segment medially on the ipsilateral side of the lip defect. A releasing incision extended inferiorly from the oral commissure to create the full-thickness transposition flap so that the flap could be sutured to the opposite border of the lip defect. The donor defect created by the transposition flap was repaired with an Estlander cross-lip flap. This and other two-flap methods are more complicated and result in three scar lines in the reconstructed lip; they also result in greater denervation of the reconstructed lip compared with use of single cross-lip flap techniques. Consequently, two-flap techniques are not generally favored methods of lip reconstruction.
Gilles Fan Flap
Gilles described a method of lip reconstruction that employs lip tissue movement in a manner similar to that accomplished by the two-flap method described by Buck but with a single flap (Fig. 19-49A, B).31 The flap is a composite flap created by full-thickness lip incisions and is designed to transfer the remaining lip segment from one side of a defect together with lip tissue from the lateral portion of the opposing lip. The flap is designed to have a narrow pedicle that incorporates the ipsilateral oral commissure. The flap is pivoted about the commissure toward the defect. Movement of the flap around the oral commissure has often been compared with that observed with opening of an old-fashioned collapsible hand-held fan. Thus, this method of reconstructing the lip has commonly been referred to as a fan flap. The feature that most distinguishes this method of repair from the circumoral rotation advancement flaps of von Bruns and Karapandzic is the near-vertical full-thickness incision made in the opposing lip. This incision is similar to the medial incision of an Estlander flap. Transfer of the flap causes blunting of the commissure, similar to that created with use of an Estlander flap. Gilles flaps may be used bilaterally when necessary to restore large full-thickness lip defects of the central lower lip (Fig. 19-50A). The primary limitation of this approach is the resulting microstomia.
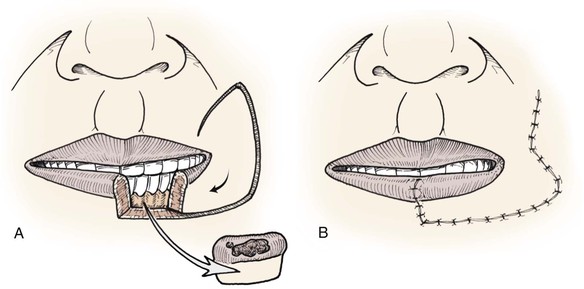
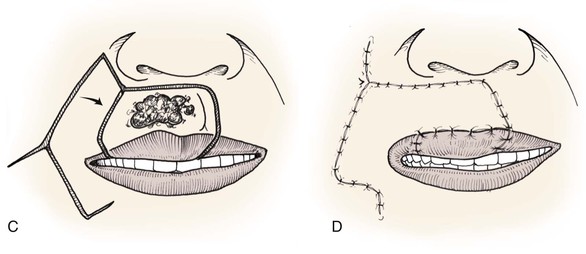
FIGURE 19-49 A, B, Gilles fan flap for reconstruction of lower lip. C, D, McGregor modification of Gilles flap for reconstruction of upper lip. Both designs were described with full-thickness lip incisions.
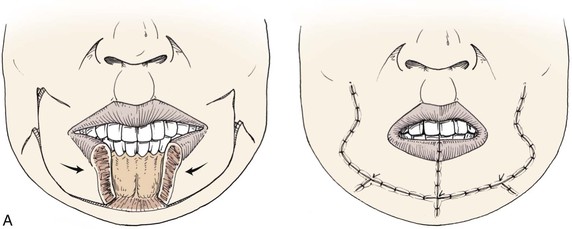
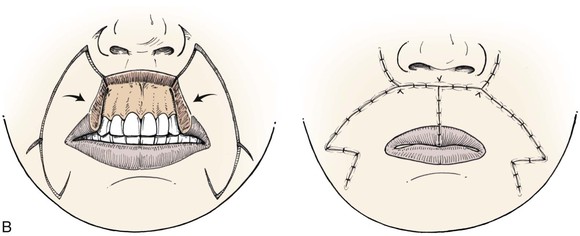
FIGURE 19-50 A, Gilles flaps may be used bilaterally to reconstruct large full-thickness central defects of lower lip. B, McGregor flaps may be used bilaterally to reconstruct large full-thickness central defects of upper lip.
McGregor has described a modification of the Gilles flap that has a similar shape but involves transfer of tissue to a defect of the upper lip from the melolabial region (see Fig. 19-49C, D).22,32 Like the Gilles flap, the McGregor flap is a composite flap created by full-thickness lip incisions. This modified design adds additional tissue about the mouth but fails to restore a complete lip muscle sphincter and does not restore a natural vermilion. Similar to the Gilles flap, the McGregor flap can be used bilaterally to reconstruct large full-thickness lip defects of the central upper lip (see Fig. 19-50B). Depending on the design of the flap, mucosa from the posterior surface of the flap may be available for advancement over the exposed border of the flap to restore the vermilion. Surgeons have used a Z-plasty along the lateral margin of the flap to assist in making the circumoral transfer (see Fig. 19-50B).
Expanded use of the Karapandzic flap has now largely replaced the use of the Gilles and McGregor flaps. However, the McGregor flap offers a reasonable alternative for repair of lateral upper lip defects when there is insufficient remaining tissue to repair the lip without recruitment of cheek skin (Fig. 19-51). When this flap is used, it is necessary to anticipate the degree of flap contraction that is likely to occur, particularly if the flap requires a skin graft on the deep surface for lining and for reconstruction of the vermilion.


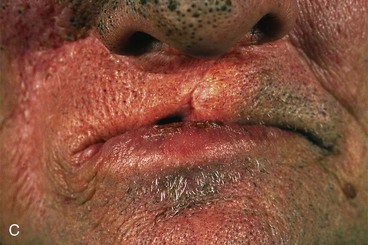
FIGURE 19-51 A, Large defect of upper lip. Bilateral McGregor flaps designed to recruit tissue from cheek for reconstruction. Broken lines indicate incisions for flaps. Skin grafts applied to deep surface and free margin of flaps. B, Flaps in place. C, Postoperative result at 6 months. Vertical height deficiency of reconstructed lip is apparent.
Commissureplasty
A problem inherent to all cross-lip flaps with a pedicle that becomes the oral commissure is blunting and distortion of the involved commissure. A later-stage commissureplasty is often necessary. The simplest method of commissureplasty involves making a horizontal full-thickness incision at the level of the blunted commissure that extends laterally to a point corresponding in position to that of the contralateral normal commissure (Fig. 19-52).33 Labial mucosa is then advanced forward on each side of the incision to restore a vermilion surface. In some cases, it may be helpful to remove a small triangle of skin and subcutaneous tissue from the area of the commissureplasty for a more natural result. This is performed cautiously to avoid oral incontinence.
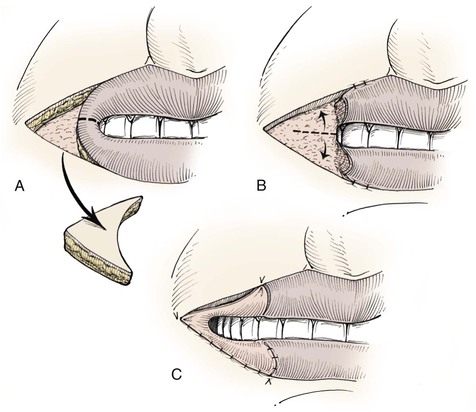
FIGURE 19-52 Commissureplasty. A, Small triangle of skin may or may not be excised lateral to distorted commissure. B, Horizontal incision made through blunted commissure. C, Mucosa advanced superiorly, inferiorly, and laterally to restore vermilion of lips and commissure.
An alternative method of commissureplasty makes use of small flaps of vermilion and orbicularis muscle (Fig. 19-53). A triangle of skin and subcutaneous tissue is excised immediately lateral to the blunted commissure. The apex of the triangle extends to the point of the new commissure. A small vermilion flap is created from one lip and left pedicled on the opposite lip. A horizontal incision is made through the muscle tissue to the point of the new commissure. The vermilion flap is advanced to this point. A small flap is created from the mucosa of the lip serving as the donor for the vermilion flap. The mucosal flap is advanced over the free border to restore the vermilion of the donor lip.
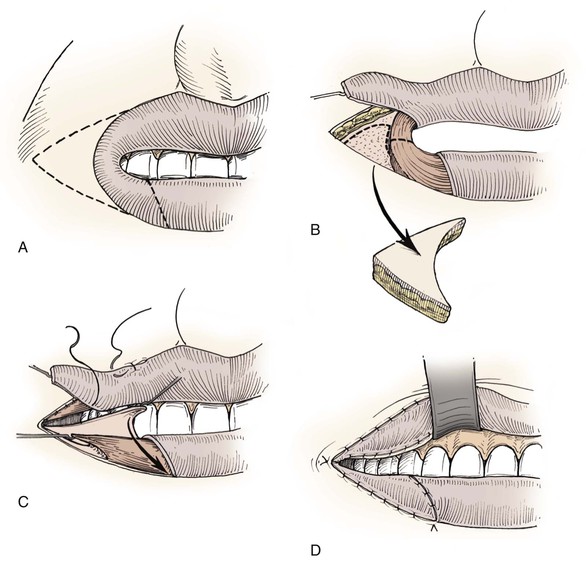
FIGURE 19-53 Commissureplasty. A, Triangle of skin marked for excision to point of new commissure. Vermilion of blunted commissure marked to create flap pedicled on upper lip. B, Skin excised. Broken line indicates planned incision through muscle of blunted commissure to extend commissure laterally and to create inferiorly based mucosal flap. C, Vermilion flap transposed to reconstruct vermilion of superior aspect of commissure. Mucosal flap advanced to reconstruct inferior vermilion of commissure. D, Flaps sutured in place.
Bilateral Cheek Advancement Flaps
Full-thickness lip defects of up to half of the width of either lip can usually be restored satisfactorily with bilateral lip advancement flaps. For larger defects, it is usually best to consider some other method of lip repair that will add more tissue to the reconstructed lip. The elasticity of lip tissue will vary among patients, as does tolerance for microstomia. In some situations, repeated manual stretching or use of a prosthetic lip-stretching appliance may help reduce problems with microstomia. In other cases, it will be necessary to recruit tissue from the adjacent cheek during reconstruction to prevent microstomia. Bernard in 1852 and von Burow in 1853 and 1855 advanced the concept of using tissue from the cheeks to restore major defects or complete loss of the upper or lower lips.1,11,34 Tissue is advanced horizontally from the medial aspect of one or, more commonly, both cheeks in the form of bilateral opposing cheek advancement flaps. This method of lip repair has been referred to as a Bernard cheiloplasty. Standing cutaneous deformities form on either side of the base of each advancement flap and are referred to as Burow triangles.11,34 A major feature of Bernard cheiloplasty is the resection of Burow triangles of skin resulting from the advancement of the cheek flaps. Excision of the triangles facilitates tissue advancement. Reconstruction of the upper lip with bilateral opposing cheek advancement flaps requires excision of four triangles of cheek skin (Fig. 19-54). Bilateral triangles of skin and subcutaneous tissue are removed from the vicinity of the alar-facial sulci superior to the flaps. Additional triangles of skin are removed from the cheek inferior to the flaps and lateral to the oral commissures. When the Bernard cheiloplasty is used to reconstruct full-thickness defects of the lower lip, reconstruction requires excision of three triangles of skin (Fig. 19-55). Triangles are removed bilaterally superior to the oral commissures. A larger triangle of skin is excised in the midline extending inferiorly from the lip defect into the chin as necessary.
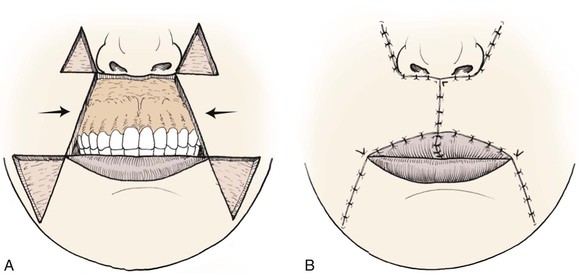
FIGURE 19-54 A, B, Bernard–von Burow opposing cheek advancement flaps for reconstruction of entire upper lip by four triangular skin excisions to facilitate advancement of cheek flaps.
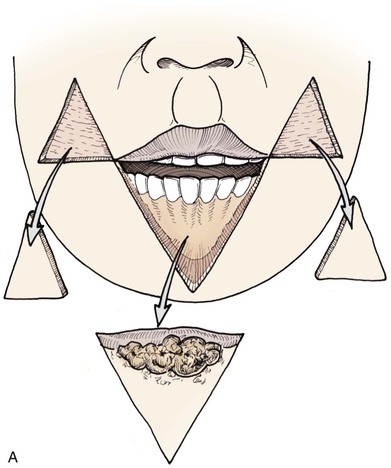
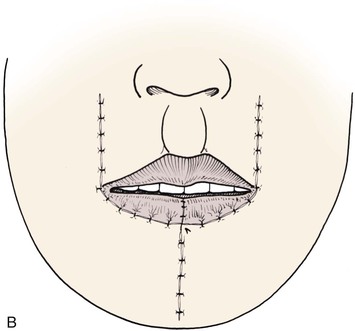
FIGURE 19-55 A, B, Bernard–von Burow opposing cheek advancement flaps for reconstruction of entire lower lip by three triangular skin excisions to facilitate advancement of cheek flaps.
Modifications of the Bernard–von Burow flaps have subsequently been described by several authors.35–37 In 1960, Webster proposed a modified design for lower lip reconstruction that employs a more linear horizontal advancement of cheek tissue compared with the Bernard–von Burow techniques. This modification positions scars in natural facial skin creases and avoids violation of the aesthetic region of the chin (Fig. 19-56).1,35 The Webster design also minimizes the tendency for vertical deficiency in the midline of the reconstructed lower lip (Fig. 19-57).
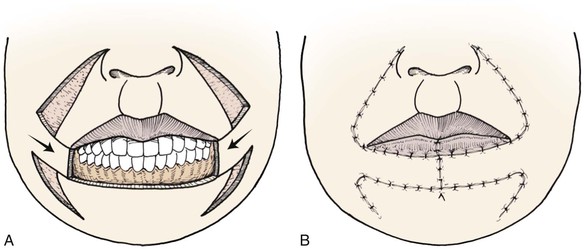
FIGURE 19-56 A, B, Webster modification of Bernard–von Burow opposing cheek advancement flaps for reconstruction of entire lower lip by four triangular skin excisions to facilitate advancement of cheek flaps. This method preserves aesthetic region of chin.
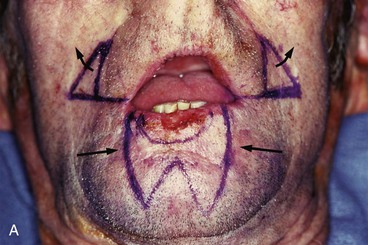





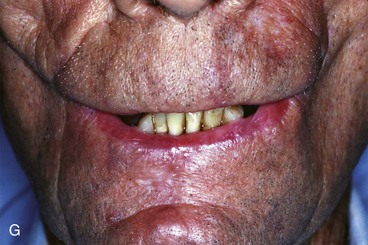
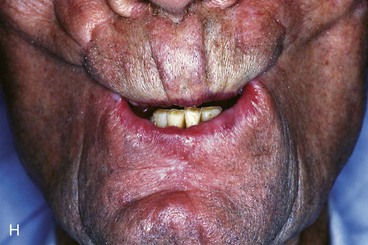
FIGURE 19-57 A, Recurrent cancer of lower lip. Width of lower lip reduced from previous wedge excision. Tumor marked for W-shaped excision. Bilateral opposing cheek advancement flaps marked by use of Webster modification without planned excision of triangles of skin from lower cheeks. B, Alternative configuration of lip excision designed so that aesthetic region of chin is not violated. C, W-shaped excision performed instead of rectangular excision in attempt to preserve sensory fibers of inferior mental nerves. D, One week postoperatively. Full-thickness horizontal incisions were made only through orbicularis muscle. Beyond this point, incisions were only through skin and subcutaneous tissues. Incisions through mucosa were made independent of skin incisions and at slightly superior level so that mucosal flaps could be dissected and advanced over exposed free margins of lateral segments of reconstructed lip. E, F, Postoperative views at 2 months with mouth closed and open. Patient is able to insert upper denture. Tightness of reconstructed lip compensates for lack of motor function of repaired lip. G, Patient cannot smile at this point without opening lips slightly. H, When simulating kissing or whistling, lips do not remain apposed.
These techniques were originally described with use of full-thickness cheek incisions and do not restore the orbicularis muscle sphincter. It is of greater benefit to the patient if flaps can be transferred with minimal violation of the facial musculature by limiting the extent of full-thickness incisions. There is also benefit to the patient if flaps are dissected with minimal violation of the sensory innervation of the flap tissue. Limiting the extent of incisions to create flaps helps preserve sensory innervation to the region. Therefore, a preferred approach for performing the Bernard and Webster cheiloplasties is to make incisions only through the skin and subcutaneous tissue layer. Labial and buccal mucosa incisions are made separate from skin incisions. The mucosal incisions do not usually require extension as far laterally as the skin incisions. Mucosal incisions are typically made at the same level as the skin incisions but may be offset at a slightly superior or inferior level, depending on which lip is reconstructed. The offset provides more mucosa that can be advanced with the flap. This additional mucosa is used to create mucosal flaps that are draped across the free margins of the flaps to restore the vermilion of the lateral portions of the reconstructed lip. What remains of orbicularis muscle is freed up sufficiently to allow flap advancement. Violation of the facial mimetic musculature is minimized by blunt spreading of tissue to enable adequate stretching without separation of the muscle attachments of the cheek flaps. Freeman37 has described a dissection along the orbicularis muscle of the opposite lip in an attempt to advance more of this muscle along with the cheek advancement flaps with the intent of improving lip function. However, this is technically difficult to accomplish.
Reconstruction of full-thickness defects of the lip with opposing cheek advancement flaps is technically difficult and oral functioning is fair at best (see Fig. 19-57). The lack of a functional muscle sphincter is offset in part by the tightness that is inherent to the reconstructed lip by this surgical approach. Whereas basic mouth opening and closing may be acceptable, more specialized lip functions, such as whistling and kissing, tend to be significantly impaired (see Fig. 19-57G, H).
Melolabial Transposition Flaps
Similar to cutaneous melolabial transposition flaps used to reconstruct cutaneous defects of the lip (see section on melolabial flaps for cutaneous repair), a thicker composite melolabial transposition flap consisting of skin and subcutaneous tissue may be used to repair full-thickness lip defects. In such instances, it is necessary to line the deep surface of the flap. This is most commonly achieved with a skin graft (Fig. 19-58). A split-thickness skin graft can be used for this purpose with perhaps an improved survival of the graft compared with use of a full-thickness skin graft. However, full-thickness skin grafts cause less wound contraction. There is considerable tendency for contraction of the melolabial flap and the lining skin graft. For this reason, both graft and flap are designed wider than the vertical height of the lip defect. The skin graft is draped over the free margin of the flap for restoration of the vermilion. A mucosal free graft may subsequently be used to replace the skin graft of the reconstructed vermilion. This is performed as a secondary procedure once the skin graft has completely healed.

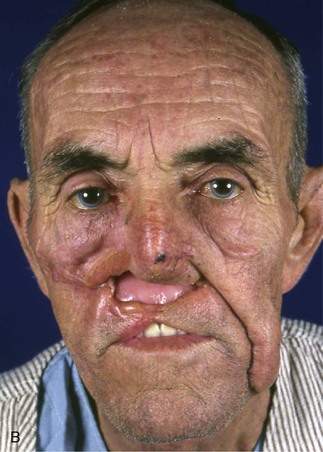


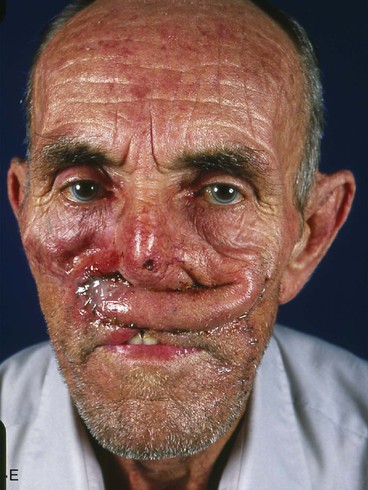
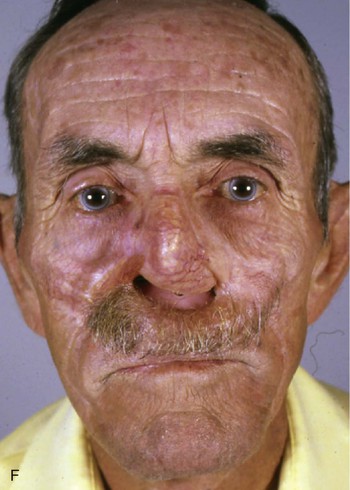
FIGURE 19-58 A, First-stage reconstruction of upper lip by delayed melolabial transposition flap lined with skin graft. Previous attempts to reconstruct upper lip had failed. Patient also smoked tobacco, so delayed flap was constructed as bipedicle flap. B, Remnants of chest flap previously used by another surgeon present in right cheek and upper lip. C, At second stage, inferior pedicle divided and flap prepared for transfer. Healed skin graft observed on deep surface of flap. The author has since observed less inflammation when edges of skin graft are sutured to borders of flap at time of delay. D, Flap transferred to upper lip. Donor cheek wound opened to facilitate cheek repair. E, Large standing cutaneous deformity at base of flap required excision in third surgical stage. F, Several months after third surgical procedure consisting of excision of standing cutaneous deformity and contouring of flap.
Melolabial flaps have a random vascular supply. Thus, they are at greater risk of necrosis when they are long relative to flap width. A greater risk of necrosis is also observed in patients who use tobacco products or have been irradiated. When there is concern for the viability of a melolabial transposition flap, employment of an initial delay may be appropriate, especially if the flap is lengthy (see Fig. 19-58). Whenever flap delay is used, consideration is given to placement of a lining skin graft on the deep surface of the flap at the time of delay. The flap is then transferred to the lip as a composite flap. This approach avoids the difficulty of securing a skin graft to the deep surface of the flap after it has been positioned in the lip recipient site. Less inflammation occurs if the grafted skin is made to extend to at least one of the skin margins along the border of the delayed flap. This provides a portal for drainage of fluid collecting beneath the flap. This maneuver also serves to begin the process of vermilion restoration necessary for the free margin of the reconstructed lip.
The use of skin-lined melolabial transposition flaps to reconstruct full-thickness lip defects will result in a thin adynamic lip segment. Designing the flap with a greater width than the vertical height of the lip defect is advisable so that the reconstructed lip will maintain adequate vertical height after wound contraction and scar maturation (Fig. 19-59). Although the flap should not be subjected to excessive wound closure tension, some tightness of the reconstructed lip can help offset the problems associated with an adynamic lip segment. Bilateral melolabial transposition flaps may be used to reconstruct large full-thickness lip defects or complete absence of the lip; one flap is used for the external lip surface, and the other is turned inward to provide lining for the reconstructed lip. However, this technique requires flaps with extended lengths, and it is technically difficult to inset the flaps while working around the pedicle of the lining flap.
Island Flaps
Several island flaps have been described for use in reconstruction of full-thickness lip defects. McHugh38 has described a horizontally oriented island flap consisting of tissue from the cheek that is transferred to the lower lip by a V-Y advancement. Fugimori39 and Stranc and Robertson40 have described a design for an island flap that employs the transfer of vertically oriented tissue to the lip from the melolabial region. The flap is pedicled on a subcutaneous tissue pedicle and is pivoted 90° and set horizontally into the lower lip. Bilateral island flaps may be used to repair larger lip defects. The island flap is created by making an incision completely around the designed flap. The flap remains pedicled on the subcutaneous tissue immediately beneath the flap. A mucosal advancement flap is draped over the free margin of the newly reconstructed lip to provide a vermilion replacement.
Horizontally oriented V-Y island advancement flaps championed by McHugh require incisions through skin and subcutaneous tissue externally and mucosa internally while maintaining the facial muscle attachments to the flap.38 The flap described by Fugimori39 and Stranc and Robertson40 is also based on the facial musculature and requires a 90° pivot, so a greater dissection within the muscle layer is required to enable flap transfer compared with the McHugh flap. Island flaps have less of a problem with bulkiness of the pedicle than flaps with a cutaneous pedicle do. The pedicle of island flaps must have an adequate random vascular supply or be designed with an axial vascular system based on branches of the facial artery. Concerns with use of island flaps for major lip reconstruction include difficulty with flap mobilization, impairment of facial nerve function, difficulty with orientation of the flap, appearance of scar lines, and viability of the flap. At present, island flaps are not considered a first choice for full-thickness lip reconstruction.
Temporoparietal Scalp Flaps
Interpolated temporoparietal scalp flaps used for lip reconstruction are technically regional flaps. In some situations, the temporoparietal flap may prove to be useful for reconstruction of large full-thickness defects of the upper or lower lip. Description of the flap is included in this chapter because it can offer a reasonably simple functional flap for restoration of a variety of large lip defects without disruption of the opposing lip and adjacent perioral structures. The temporoparietal scalp flap is based on the posterior branch of the superficial temporal artery that travels from the preauricular region superiorly beneath the skin in the plane of the temporoparietal fascia to the midline of the scalp. In many patients, the course of the artery can be detected with gentle palpation and can be mapped out very well with use of a Doppler device. The flap is created by making vertical incisions angled posteriorly on both sides parallel to the course of the posterior branch of the superficial temporal artery (Fig. 19-60). The flap is pedicled on tissue in the immediate preauricular region at the level of the zygoma. Care is taken to avoid injury to the temporal artery and accompanying venous drainage, particularly in the region of the pedicle.


FIGURE 19-60 A, Temporoparietal scalp flap marked. Course of posterior branch of superficial temporal artery marked in center of flap. Course of anterior branch of artery indicated at base of flap. B, Same patient as in A with flap transferred to upper lip.
When full-thickness lip defects are reconstructed with an interpolated temporoparietal scalp flap, the deep surface of the flap is usually covered with either a full-thickness or split-thickness skin graft to provide an intraoral surface lining. Whereas a split-thickness skin graft is relatively easy to harvest and can have a long length to cover a sizable portion of the flap’s undersurface, a full-thickness skin graft offers a more durable tissue surface and is relatively less prone to contraction. It can be challenging to securely attach a skin graft to the deep surface of the temporoparietal scalp flap as the flap is being transferred to the mouth because a bolster dressing to secure the skin graft is awkward and may risk impairment of vascularity to the flap. When possible, it may be preferable to stage the procedure by delaying the flap and placing a skin graft on the ventral surface of the flap (Fig. 19-61). Use of a delayed stage can help “train” the flap tissue to adapt to an alteration in its vascular supply while simultaneously allowing a skin graft to heal to the deep surface of the flap. The second stage is then performed, transferring the composite flap to the recipient lip site. During the delay stage, the distal end of the flap may remain attached to the scalp in the form of a bipedicle flap until the time of actual flap transfer.


FIGURE 19-61 A, Skin graft placed on deep surface of temporoparietal scalp flap at time of flap delay. B, Incisions closed after placement of skin graft.
The temporoparietal scalp flap can be designed for reconstruction of an entire upper or lower lip. It can be designed as a bipedicle flap that is connected across the top of the scalp and transferred to the lip as an interpolated flap in a bucket-handle fashion. Such a flap design is more safely accomplished by use of a delayed stage as circulation across the top of the scalp is random. It is possible to reconstruct an entire lip with use of a single-pedicled temporoparietal flap (Fig. 19-62). In such cases, use of a delayed stage is preferred to ensure the vascularity of the distal end of the flap. Insetting of a single-pedicle flap is much easier than that of a bipedicle flap. A single-pedicle flap also causes less distortion of the scalp. It is also appreciably easier for the patient to deal with a flap pedicled on only one side of the face. The amount of surface contact between the flap and the lip recipient site influences how long the flap remains pedicled to the scalp. In most cases, a period of at least 3 weeks is used between the initial transfer of the flap to the mouth and flap inset, but this interval can be varied. On occasion, division of the pedicle may be performed in stages to reduce the risk of flap necrosis.

FIGURE 19-62 A, Full-thickness defect of entire lower lip. B, C, First-stage reconstruction of same patient as in A with single-pedicle interpolated temporoparietal scalp flap lined with full-thickness skin graft.
Scalp skin has a different character than lip skin (Fig. 19-63). Because the temporoparietal scalp flap is hair bearing, it is more suited to reconstruction of the lip in men. Hair growth on the flap can simulate a moustache or beard and aid in camouflage of the reconstruction (Fig. 19-64). It is important to appreciate that reconstruction with a temporoparietal scalp flap does not restore motor function to the lip but will serve as a static mouth cover. Adynamic reconstruction is better suited to restoration of the upper lip than of the lower lip.




FIGURE 19-63 A, After first-stage interpolated temporoparietal scalp flap to reconstruct upper lip. B, Postoperative view 6 months after division of pedicle and inset of flap. Considerable discrepancy of skin color, texture, and pattern of hair growth exists between flap and native lip skin. Patient considered overall lip function satisfactory and did not wish vermilion reconstruction with mucosal graft. Prosthetic nose in place. C, Large lower lip defect. Previous melolabial transposition flap repair failed. D, Same patient as in C several months after two-stage reconstruction with interpolated temporoparietal scalp flap.

FIGURE 19-64 A, After transfer of interpolated temporoparietal scalp flap to reconstruct upper lip. Note: Local anesthetic containing epinephrine has been infiltrated into the pedicle, causing blanching; distal end of flap continues to demonstrate normal skin color, indicating no impairment of vascularity. B, Same patient as in A after inset of flap. Hair growth on flap simulates moustache and aids in scar camouflage.
Other Flap Reconstructions
A number of additional flaps from regional or distant sites may be used to reconstruct full-thickness defects of the lip. These flaps are beyond the purpose of this chapter and are mentioned only briefly for completeness.41–44 Regional and distant flaps are usually selected for lip reconstruction when there is need for total restoration of either lip. Historically, the most common regional flap used for this purpose consisted of transposition of forehead skin pedicled laterally on the anterior branch of the superficial temporal artery. This flap remains an option for reconstruction of the entire lip; however, it is currently less favored as it requires multiple stages and tends to cause a “skull-like” appearance of the donor forehead, which is covered with a split-thickness skin graft.41,43 The deltopectoral chest flap offers a large quantity of tissue that can be used for reconstruction of major defects of one or both lips.42,43 Whereas the pedicle is based on multiple intercostal perforating arteries from the anterior chest wall, the useable distal portion of the flap has a random circulatory supply, and thus the flap requires delay to ensure its viability. Redundant pedicle tissue of the flap may be folded and used for lip lining. This approach provides improved results compared with use of a skin graft to line the flap.
In addition to the deltopectoral chest flap, other flaps constructed from the platysma and sternocleidomastoid muscles have been used to reconstruct large full-thickness lip defects. These muscle flaps are difficult to dissect and are uncertain in their result. The current trend for total lip reconstruction is immediate single-stage reconstruction with a microsurgical flap. The radial forearm flap is the preferred flap because it offers a relatively thin and pliable skin flap and limited donor site morbidity in most patients.44 Although regional, distant, and microsurgical flaps can transfer large surface areas of skin and soft tissue to the region of the lip, such flaps provide limited or no dynamic motion of the reconstructed lip and show considerable tendency to sag, particularly when they are used to reconstruct the lower lip.
References
1. Mazzola, RF, Lupo, G. Evolving concepts in lip reconstruction. Clin Plast Surg. 1984; 11:583.
2. Zide, BM, Deformities of the lips and cheeks. Plastic surgery. McCarthy, JG, eds. Plastic surgery; vol. 3. WB Saunders, Philadelphia, 1990.
3. Park, C, Lineaweaver, WC, Buncke, HJ. New perioral arterial flaps: anatomic study and clinical application. Plast Reconstr Surg. 1994; 94:268.
4. Kriet, JD, Cupp, CL, Sherris, DA, Murakami, CS. The extended Abbe flap. Laryngoscope. 1995; 105:988.
5. Karapandzic, M. Reconstruction of lip defects by local arterial flaps. Br J Plast Surg. 1974; 27:93.
6. Jabaley, ME, Clement, RL, Orcutt, TW. Myocutaneous flaps in lip reconstruction: application of the Karapandzic principle. Plast Reconstr Surg. 1977; 59:680.
7. Reid, DA. A mucosal cross-lip flap. Br J Plast Surg. 1956; 9:106.
8. McGregor, IA. The tongue flap in lip surgery. Br J Plast Surg. 1966; 19:253.
9. Bakamjian, V. Use of tongue flaps in lower lip reconstruction. Br J Plast Surg. 1964; 17:76.
10. Goldstein, MH. A tissue-expanding vermilion myocutaneous flap for lip repair. Plast Reconstr Surg. 1984; 73:768.
11. von Burow, CA. Beschreibung einer neuen Transplantations-methode (Method der seitlichen Dreiecke) zum Wiederersatz verlorengegangener Teile des Gesichts. Berlin: Nauck; 1855.
12. Szlazak, J. The application of a Burow triangular flap in reconstruction of the lower lip. Br J Plast Surg. 1958–1959; 11:128.
13. Isaksson, I, Johanson, B. Partial reconstruction of the lower lip. Panminerva Med. 1967; 9:420.
14. Johanson, B, Aspelund, E, Breine, U, Holmstrom, H. Surgical treatment of non-traumatic lower lip lesions with special reference to the step technique. Scand J Plast Reconstr Surg. 1974; 8:232.
15. von Bruns, V. Chirurgischer Atlas: Bildliche Darstellung der chirurgischen Krankheiten und der zu ihrer Heilung erforderlichen Instrumente, Bandagen und Operationen, II Abt, Kau- und Geschmaks-Organ. Tubingen: Luupp; 1857.
16. Sabattini, P. Cenno storico dell’origine e progressi della rinoplastica e cheiloplastica. Bologna: Belle Arti; 1838.
17. Stein, SAW. Laebedannelse udført paa en ny methode. Hospitals-Meddelelser. 1848; 1:212.
18. Buck, G. Contributions to reparative surgery: showing its application to the treatment of deformities, produced by destructive disease or injury; congenital defects from arrest or excess of development; and cicatricial contractions from burns. New York: D Appleton; 1876.
19. Abbe, RA. A new plastic operation for the relief of deformity due to double hairlip. Med Rec. 1898; 53:477.
20. Franchebois, P. Improved surgical treatment of cancer of the lower lip. Int Surg. 1975; 60:204.
21. Templer, J, Renner, G, Davis, WE, Thomas, JR. A modification of the Abbe-Estlander flap for defects of the lower lip. Laryngoscope. 1981; 91:153.
22. McCarn, KE, Park, SS. Lip reconstruction. Facial Plast Surg Clin North Am. 2005; 13:301.
23. Smith, JW. The anatomical and physiologic acclimatization of tissue transplanted by the lip switch technique. Plast Reconstr Surg. 1960; 26:40.
24. Thompson, N, Pollard, AC. Motor function in Abbe flaps: a histochemical study of motor reinnervation in transplanted muscle tissue of the lips in man. Br J Plast Surg. 1961; 14:66.
25. Estlander, JA. Eine Methode aus der einen Lippe Substanzverluste der anderen zu ersetzen [reprinted in English translation in Plast Reconstr Surg 42:361, 1968]. Arch Klin Chir. 1872; 14:622.
26. Baker, SR, Swanson, NA. Local flaps in facial reconstruction. St. Louis: Mosby; 1995.
27. Baker, SR, Krause, CJ. Cancer of the lip. In: Suen JY, Myers EN, eds. Cancer of the head and neck. New York: Churchill Livingstone, 1981.
28. Kazanjian, VH, Roopenian, A. The treatment of lip deformities resulting from electric burns. Am J Surg. 1954; 88:884.
29. Martin, HE. Cheiloplasty for advanced carcinoma of the lip. Surg Gynecol Obstet. 1932; 54:914.
30. Murray, JF. Total reconstruction of a lower lip with bilateral Estlander flaps: case report. Plast Reconstr Surg. 1972; 49:658.
31. Gilles, H, Millard, R. The principles and art of plastic surgery. London: Butterworth; 1957.
32. McGregor, IA. Reconstruction of the lower lip. Br J Plast Surg. 1983; 36:40.
33. Anderson, R, Kurtay, M. Reconstruction of the corner of the mouth. Plast Reconstr Surg. 1971; 47:463.
34. Bernard, C. Cancer de la lèvre inférieure: restauration á l’aide de deux lambeaux latéraux quadrilatères: guérison. Bull Mem Soc Chir Paris. 1853; 3:357.
35. Webster, RC, Coffey, RJ, Kelleher, RE. Total and partial reconstruction of the lower lip with innervated muscle-bearing flaps. Plast Reconstr Surg. 1960; 25:360.
36. Webster, JP. Crescentic peri-alar cheek excision for upper lip flap advancement with a short history of upper lip repair. Plast Reconstr Surg. 1955; 16:434.
37. Freeman, BS. Myoplastic modification of the Bernard cheiloplasty. Plast Reconstr Surg. 1958; 21:453.
38. McHugh, M. Reconstruction of the lower lip using a neurovascular island flap. Br J Plast Surg. 1977; 30:316.
39. Fujimori, R. “Gate flap” for the total reconstruction of the lower lip. Br J Plast Surg. 1980; 33:340.
40. Stranc, MF, Robertson, GA. Steeple flap reconstruction of the lower lip. Ann Plast Surg. 1983; 10:4.
41. McGregor, IA, Reconstruction following excision of intraoral and mandibular tumors. Reconstructive plastic surgery. Converse, JM, eds. Reconstructive plastic surgery; vol. 5. WB Saunders, Philadelphia, 1977.
42. Bakamjian, V, Culf, NK, Bales, HW. Versatility of the deltopectoral flap in reconstructions following head and neck cancer surgery. In: Sanvenero-Rosselli G, Boggio-Robutti G, eds. Transaction of the 4th International Congress of Plastic Surgery, Rome. Amsterdam: Excerpta Medica, 1969.
43. Renner, G. Lip reconstruction. In: Day TA, Girod DA, eds. Oral cavity reconstruction. New York: Taylor & Francis, 2006.
44. Sadove, RC, Luce, EA, McGrath, PC. Reconstruction of the lower lip and chin with the composite radial forearm–palmaris longus free flap. Plast Reconstr Surg. 1991; 88:209.