Excessive range of movement
Instability of the shoulder
Definition
Glenohumeral instability is defined as ‘the inability to maintain the humeral head centred in the glenoid fossa’.1 Recurrent instability may be characterized as dislocation, subluxation or apprehension. Dislocation is the complete separation of the articular surfaces without spontaneous relocation. Subluxation is defined as symptomatic translation of the humeral head without complete separation of the articular surfaces. Apprehension refers to the fear that the shoulder will subluxate. Instability can also be characterized according to the direction of the (sub)luxation: anterior, posterior, inferior and superior. Subluxations can also be classified according to their cause: they may be traumatic, atraumatic or voluntary. Around 95% of (sub)luxations are anterior. Most have a traumatic origin, although instability can also result from relatively small but repeated movements of the arm as may occur in swimmers, volleyball players or baseball pitchers.2 Derangement of the labrum, intracapsular ligaments or joint capsule are regarded as the main underlying causes of chronic instability.3 Exceptionally, osseous changes such as a fracture of the glenoid are found.
Factors in glenohumeral stability
A considerable range of mobility is essential at the glenohumeral joint. As a consequence, the shoulder has less bony and ligamentous stability than any other diarthrodial joint. There is a considerable incongruence between the two articulating surfaces with only 25–30% of the humeral head being covered by the glenoid fossa. This enables a wide range of positions without neck-rim contact.4 Furthermore, the glenohumeral joint does not have strong isometric articular ligaments that provide stability while the joint is flexed around a defined anatomical axis as is the case in knee, elbow and ankle joints. Instead, the glenohumeral ligaments have a stabilizing function only at the extremes of motion and play no part in most functional positions of the joint.5
In spite of all this, the normal shoulder joint is quite stable and able to centre the humeral head in the glenoid cavity throughout most of the arc of movement.6 This is achieved by a set of mechanisms which classically are divided into static factors (those that do not require the expenditure of energy by muscles) and dynamic factors (requiring muscle energy).
Static factors
Joint surfaces
Recent studies have demonstrated that, although the bony surfaces of the joint are largely incongruent (flat glenoid and round humerus), congruence is restored by the difference in thickness of cartilage. Glenoid cartilage was found to be the thickest at the periphery and thinnest centrally, whereas humeral articular cartilage was thickest centrally and thinnest peripherally (Fig. 1). This leads to a merely uniform contact between humeral head and glenoid surface throughout shoulder motion.7
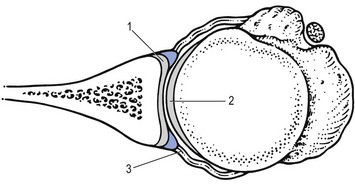
Fig 1 Glenoid cartilage is thickest at the periphery (1); humeral cartilage is thickest centrally (2). The glenoid labrum increases the depth of the glenoid socket and the surface area for the humeral head (3).
The glenoid labrum contributes to stability by increasing the depth of the glenoid socket (Fig. 1) and so increasing the surface area for the humeral head.8,9
Cohesion–adhesion forces
Joint surfaces, wet with joint fluid, are held together by the molecular attraction of the fluid to itself and to the joint surfaces. This is called the adhesion–cohesion mechanism (compare with two wet microscope slides pressed together) and is a very strong stabilizing factor in the glenohumeral joint.
Negative pressure
There is minimal (less than 1 cc) free fluid in the normal shoulder joint. The normal shoulder is sealed by the capsule so that external fluid cannot enter it. Osmotic action by the synovium removes free fluid, keeping a slightly negative pressure within the normal joint. The negative intra-articular pressure creates a vacuum that pulls the humerus against the glenoid.10 The limited joint volume effect is reduced if the joint is ‘vented’ (opened to the atmosphere) or when the capsular boundaries of the joint are very compliant.11 This will lead to the production of a ‘sulcus sign’ (see below): under attempted traction on the arm, the flexible capsule is dragged into the joint.
Capsule and ligaments
The joint capsule is large, loose and redundant (the capacity of the glenohumeral joint capsule is larger than that of the humeral head). Capsule and ligaments alone cannot prevent glenohumeral translation when the joint is in most of its range of movement. Recent studies show that the main importance of the capsule for stability lies in the feedback mechanism of the proprioceptive innervation and contraction of the rotator cuff.12,13
Dynamic factors
Both shoulder girdle and rotator cuff muscles contribute to ‘dynamic’ glenohumeral stability. The muscles of the shoulder girdle (trapezius, rhomboideus, latissimus dorsi, serratus anterior and levator scapulae) stabilize the scapula as a firm platform for movement of the humeral head.14 The ‘rotator cuff’ (supraspinatus, infraspinatus, subscapularis and the long head of the biceps) serves three stabilizing functions:
• Dynamic ligaments. By virtue of the blending of their tendons with the glenohumeral capsule and ligaments, selective contraction of the cuff muscles can adjust the tension in these structures, producing dynamic ligaments.15,16
• By contracting together, the rotator cuff muscles and the biceps press the humeral head into the glenoid fossa (Fig. 2), locking it into position and thus providing a secure scapulohumeral link for upper extremity function.17
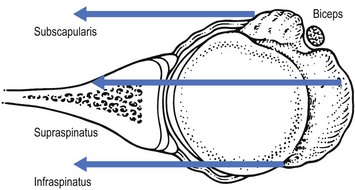
Fig 2 By contracting together the rotator cuff muscles and the biceps press the humeral head into the glenoid fossa, locking it in position.
• By contracting selectively, the rotator cuff muscles can resist displacing forces resulting from contraction of the principal shoulder motors.18 For example, when the pectoralis major and anterior deltoid muscles elevate and flex the shoulder, they tend to push the humeral head out the back of the glenoid fossa; this displacement is resisted by contraction of the subscapularis, infraspinatus and teres minor (Fig. 3). When the lateral deltoid initiates shoulder abduction, the supraspinatus and the long head of the biceps actively resist upward displacement of the humeral head relative to the glenoid fossa.
Fig 3 By contracting selectively the rotator cuff muscles can resist the displacing forces of the principal shoulder motors.
History
The history and detailed physical examination are both very important for diagnosis. Unfortunately symptoms are often vague and clinical findings subtle.19,20 The majority of patients mention a previous injury, usually a fall onto the outstretched arm in lateral rotation and abduction, which resulted in a luxation of the humeral head.21 However, it should not be assumed that there is also a record of manipulative reduction at that time because in most cases the humeral head only subluxates and immediately reduces spontaneously. The earlier in life this happens, the more likely is future transient subluxation.22 Sometimes, patients are encountered without a history of earlier displacement. This situation is called atraumatic instability and is more likely to be multidirectional. Atraumatic instability is more a syndrome that may arise from a set of pathogenic disorders: a flat glenoid, compliant capsule or weak neuromuscular control. It is often referred to as the AMBRII syndrome: Atraumatic, Multidirectional, Bilateral, with Rehabilitation directed at restoring neuromuscular control, as the most important therapeutic measure; in case surgery is necessary, it should include reconstruction of the rotator Interval and tightening of the Inferior capsule.23–25
An attack of subluxation is usually described as follows: the patient experiences a sudden paralysing pain and weakness of the arm during activity. Whatever is held may be dropped. Very often the pain is brought on by unguarded movements such as raising the arm during throwing, swimming or serving at tennis. The pain is only momentary and disappears spontaneously after a few moments, after which the patient is usually able to return to activities without much pain or problem. In advanced cases, however, and after repeated attacks, the shoulder may be felt to slip out and clunk back into place with increasing ease and in an increasing number of activities.26 Finally the shoulder may become uncomfortable even with the arm at rest and by then the acute symptoms are brought about with less forceful activities such as turning the steering wheel of a car or when the patient puts the arm in the sleeve of a coat.27
Functional examination
The basic functional examination may show some abnormal findings, typical for a possible minor instability: an enlarged range of movement (ROM) and a loose end-feel. Momentary subluxation can also appear as a kind of painful arc.28 During active elevation of the arm, the humeral head subluxates to a certain extent, blocks the movement for a while and slips back into place as the movement is continued. Recently it has been shown that a real painful arc, caused by impingement, may coexist in subluxation of the shoulder as a secondary phenomenon to the instability.29,30 An overlap seems to exist in the concepts of instability and impingement and for this reason when a painful arc is present minor shoulder instability must always be kept in mind.31,32 On passive lateral rotation, when performed firmly, a different type of end-feel may be encountered. First resistance is felt, which then is overcome and finally gives rise to a new ligamentous end-feel. When the arm is brought back to neutral position a click is often felt. This sequence of sensation – although not necessarily painful – may indicate anterior instability. The same occurs in posterior instability for passive medial rotation.
Accessory tests
If a minor instability is suggested after the history and the basic functional examination, the classic stress tests to challenge the stability of the joint in various directions must be performed. During these tests, both apprehension and palpable subluxations are sought. To differentiate normal laxity from pathological instability, both shoulders should be compared. The uninvolved arm is always examined first.
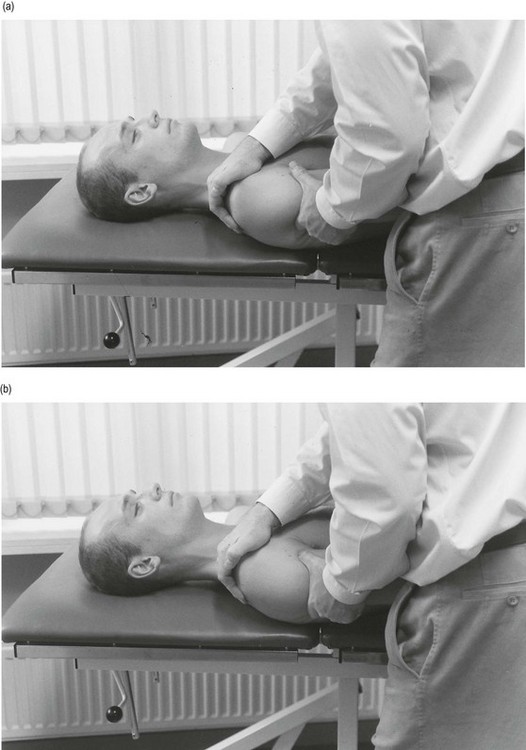
Apprehension test for recurrent anterior dislocation (Fig. 4)
This test can be performed with the patient either standing or supine. The fingers of the contralateral hand are placed on the anterior aspect of the humeral head, the thumb posteriorly. With the other hand the examiner brings the arm into full lateral rotation. In this position, anteriorly directed pressure is applied with the thumb to the posterior part of the humeral head.33 The test can be repeated with increasing degrees of abduction varying from 90° to full elevation. The test is regarded as positive if the patient judges that it provokes the same impression as the one felt when the shoulder moves out of place. Pain alone is not regarded as a positive apprehension sign. The examiner must be able to feel the humeral head subluxating or the patient looks and feels apprehensive and resists further motion. Thus, the apprehension is greater than the pain.34
Relocation test (Fig. 5)
If, with the arm still in full lateral rotation, a posteriorly directed force is applied to the anterior aspect of the humerus, it relocates the head of the humerus within the glenoid fossa. The patient loses the apprehension, the pain decreases and further lateral rotation is possible. This ‘relocation test’ is very valuable in differentiating a simple impingement from a real anterior subluxation.35,36
Apprehension test for recurrent posterior dislocation (Fig. 6)
The patient lies supine, with the arm abducted to 90° and the elbow flexed to a right angle. The examiner places the contralateral hand under the glenohumeral joint. The shoulder is then brought very gently into medial rotation – if the test is done too quickly, the humerus might subluxate. A positive test for posterior instability is indicated by a feeling of apprehension and the patient’s resistance to further motion. The patient may also state that the feeling at the end of the test is what was felt when the shoulder was previously dislocated.
Load-and-shift manūuvres (anterior and posterior drawer) (Fig. 7)
These tests are performed with the patient in the supine position, lying with the scapula on the couch, but with the humerus beyond the edge. The contralateral hand fixates the scapula with the thumb or thenar placed on the coracoid process and the fingers on the acromion. Before assessing the amount of translation it is important that the humeral head is brought initially into its neutral position in the glenoid fossa (i.e. ‘loaded’). This is achieved by placing the shoulder in a position of neutral rotation: the humerus in approximately 20° of abduction and forward flexion. The elbow is flexed and the arm directed upwards. The ipsilateral hand grasps the patient’s humerus in the axilla and the shift manūuvres are performed by moving both hands in opposite directions: the anterior shift by translating the humerus anteriorly, the posterior shift by moving the humerus posteriorly in relation to the scapula. Translation of up to 25% of the humeral head diameter both anteriorly and posteriorly are considered normal,37 although some authors state that anterior translation is less than posterior translation.38
Sulcus sign
With the arm hanging down and maximally relaxed, traction (Fig. 8) may provoke inferior subluxation of the head of the humerus. An increase of the space between humerus and acromion is shown in the skin being pulled towards the bone (i.e. sulcus sign).39 When present it points towards inferior subluxation of the humeral head which is usually part of a multidirectional instability.40
Diagnosis
Instability tests are performed only if the patient gives a history of shoulder instability. In other conditions, for example shoulder arthritis or bursitis, these tests would be very painful. In anterior instability the apprehension and relocation tests as well as the anterior load-and-shift manūuvre are usually positive, although sometimes very subtle.41,42 If the sulcus sign is also found, multidirectional instability is present.43
Diagnosis of posterior instability is based on the patient’s ability to reproduce the subluxation by arm positioning in flexion and medial rotation. Posterior apprehension is usually absent and posterior translation of the humeral head on the glenoid may provide the only clue to the diagnosis of posterior instability.44,45
If inferior instability is also present, distal traction may reproduce the symptoms, suggesting multidirectional instability.46 It has been reported that the best position to test for inferior instability is at 20 to 30° of abduction.47
Since a momentary subluxation of the humeral head on elevation can give rise to the impression of a painful arc, all other lesions causing a painful arc must also be included in the differential diagnosis. None of these lesions, however, provokes the sensation of instability. In the assessment of chronic instability of the shoulder, special X-ray views may be helpful to determine bony anatomy and pathological change.48 CT scan, MRI and arthrography seem to have limited application in the routine roentgenographic diagnosis of the unstable shoulder.49
Treatment
Initial treatment for minor instability is conservative50 and banks on three pillars:
• Strengthening of the periscapular muscles
• Training of the antagonists of the deltoid
• Training of the neuromuscular control of the rotator cuff muscles.
Provide a firm base
Fixation of the scapula must be optimal. Therefore, the scapular rotators (trapezius, levator scapulae, serratus anterior, rhomboids and pectoralis minor) must be trained to provide a stable platform for the humeral head.51
At first only isometric exercises should be given; later isotonic contractions are added to the training session. It is important, however, not to use long levers; only the muscles of the shoulder girdle are trained and the humerus stays alongside the trunk because long-lever exercises may put excessive strain on the rotator cuff and shoulder ligaments.
Train strength and propriocepsis of the antagonists of the deltoid: the latissimus dorsi and the pectoralis major muscles. To start with, only isometric exercises from 90° of abduction are given. The purpose is to train the muscular feeling and active relaxation of the deltoid. A caudal movement of the humeral head is encouraged. Later on isotonic exercises are added. These consist of active adduction movements, using weights and a pulley – in the beginning only with a short lever, later with the use of the stretched arm. Finally, coordination exercises complete the session: training of contractions of the antagonists during active elevation of the arm – this in an attempt to pull the head of the humerus in a caudal direction during active abduction of the arm.
Proprioceptive exercises for the rotator cuff muscles
It has been demonstrated that the muscles of the rotator cuff serve a complementary function to adjust tension in the capsuloligamentous system.51 The simultaneous contraction of rotator cuff and biceps causes the humeral head to be compressed into the glenoid. Furthermore, selective muscular contraction of the subscapularis plays an important role in limiting anterior translation,52,53 whereas teres minor and infraspinatus have a similar function with regard to posterior instability.54 The purpose is to train the muscular response to the capsular neuroreceptor input. This is mainly done under eccentric conditions: the muscle is activated while being stretched. Acceleration and deceleration movements are performed under high speed while using small weights.
In practice the training consists of three exercises:
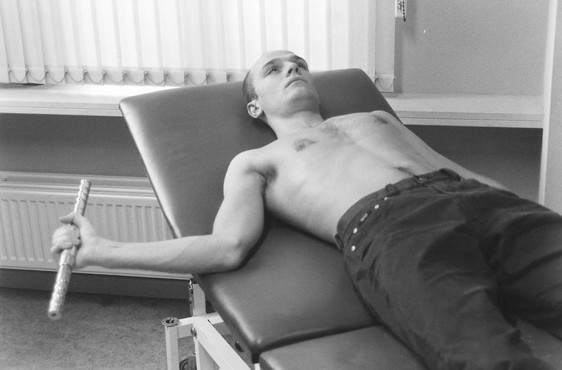
• In supine lying: the elbow is held close to the body. A small weight (+/− 1 kg) is rotated towards and away from the trunk. The speed of rotation will change from one cycle/3–4 seconds to one cycle/second. This movement trains capsular feedback for the infraspinatus and subscapularis muscles (Fig. 9).
• In side lying: the shoulder is slightly flexed and in medial rotation. A small weight (0.5 kg) is lifted and brought back. The arm remains stretched and the movement is repeated, first slowly (one cycle/3 seconds) and gradually speeding to one cycle/second. This movement trains capsular feedback for the supraspinatus muscle (Fig. 10).
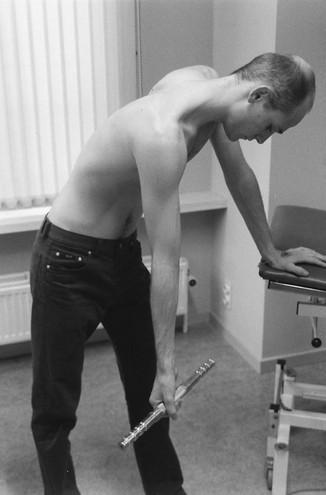
• Standing: the trunk is slightly flexed, the arm hanging by the side. A weight of about 2–3 kg is used. The patient is asked to let the arm hang down and to relax the deltoid muscle as much as possible. Maximal internal and external rotations are now performed. First slowly, to the very end of range, then more quickly. These acceleration–deceleration exercises, with increasing velocity, train the capsular feedback for subscapularis, infraspinatus and teres minor. The deltoid should be maximally relaxed (Fig. 11).
Surgery
When surgery is called for, it is extremely important that the differentiation between a posterior, anterior and multidirectional displacement is clear. If not, the operation will make the condition worse. The indications for operation depend on various factors such as disability during daily activities, pain and frequency of dislocations. Operative results are fairly good in anterior instability55 depending on the type of surgical procedure56,57 but results are less good in posterior instability in which a 40% failure rate exists.58 Multidirectional instability is also not conducive to a good outcome.59
References
1. Matsen FA, III., Fu FH, Hawkins RJ, eds. The Shoulder: A Balance of Mobility and Stability. Rosemont, IL: American Academy of Orthopaedic Surgeons, 1993.
2. Schwartz, E, Warren, R, O’Brien, S, Fronek, J, Posterior shoulder instability. Orthop Clin North Am. 1987;18(3):409–419. ![]()
3. Schewelies, S. Die habituelle Schulterluxation. Physiotherapie. 1979; 6:507–509.
4. Turkel, SJ, Panio, MW, Marshall, JL, Girgis, FG, Stabilizing mechanisms preventing anterior dislocation of the glenohumeral joint. J Bone Joint Surg 1981; 63A:1208–1217. ![]()
5. Warner, JJ, Deng, XH, Warren, RF, Torzill, PA, Static capsuloligamentous restraints to superior–inferior translation of the glenohumeral joint. Am J Sports Med 1992; 20:675–685. ![]()
6. Howell, SM, Galinat, BJ, Renzi, AJ, Marone, PJ, Normal and abnormal mechanisms of the glenohumeral joint in the horizontal plane. J Bone Joint Surg 1988; 701:227–232. ![]()
7. Soslowski, LJ, Bigliani, LU, Flatow, EL, et al, Articular geometry of the glenohumeral joint. Clin Orthop 1992; 285:181–190. ![]()
8. Howell, SM, Galinat, BJ, The glenoid–labral socket: a constrained articular surface. Clin Orthop 1989; 243:122–125. ![]()
9. Bowen, MK, Deng, XH, Hannafin, JA, et al. An analysis of the patterns of glenohumeral joint contact and their relationship to the glenoid ‘bare area’. Trans Orthop Res Soc. 1992; 17:496.
10. Levick, JR. Joint pressure–volume studies: their importance, design and interpretation. J Rheumatol. 1983; 10:353–357.
11. Gibb, TD, Harryman, DT, II., Sidles, JA, et al, The effect of capsular venting on glenohumeral laxity. Clin Orthop 1991; 268:120–127. ![]()
12. Jerosch, J, Steinbeck, J, Clahsen, H, Schmitz-Nahrath, M, Grosse-Hackmann, A, Function of the glenohumeral ligaments in active stabilisation of the shoulder joint. Knee Surg Sports Traumatol Arthrosc. 1993;1(3–4):152–158. ![]()
13. Wülker, M, Rossig, S, Korell, M, Thren, K. Dynamic stability of the glenohumeral joint. A biomechanical study. Sportverletz Sportschaden. 1995; 9:11–18.
14. Kronberg, M, Nemeth, G, Brostrom, LA, Muscle activity and coordination in the normal shoulder: An electromyographic study. Clin Orthop 1990; 257:76–85. ![]()
15. Terry, GC, Hammon, D, France, P, Norwood, L, The stabilizing function of passive shoulder restraints. Am J Sports Med 1991; 19:26–34. ![]()
16. Warner, JJ, Lephart, S, Fu, FH, Role of proprioception in pathoetiology of shoulder instability. Clin Orthop 1996; 330:35–39. ![]()
17. Howell, SM, Galinat, BJ, The glenoid–labral socket. A constrained articular surface. Clin Orthop 1988; 243:122. ![]()
18. Loehr, JF, Helmig, P, Sojbjerg, JO, Jung, A, Shoulder instability caused by rotator cuff lesions. An in vitro study. Clin Orthop 1994; 304:84–90. ![]()
19. Mizuno, K, Nabeshima, Y, Hirohata, K, Analysis of Bankart lesion in the recurrent dislocation or subluxation of the shoulder. Clin Orthop Rel Res 1993; 288:158–165. ![]()
20. Kvitne, R, Jobe, F, The diagnosis and treatment of anterior instability in the throwing athlete. Clin Orthop Rel Res 1993; 291:107–123. ![]()
21. Dalton, S, Snyder, S, Glenohumeral instability. Baillière’s Clin Rheumatol. 1989;3(3):511–534. ![]()
22. Schwartz, E, Warren, R, O’Brien, S, Fronelk, J, Posterior shoulder instability. Orthop Clin North Am. 1987;18(3):409–419. ![]()
23. Lippit, SB, Harryman, DT, II., Sidles, JA, Matsen, FA, III. Diagnosis of management of AMBRII syndrome techniques. Techniques Orthop. 1991; 6:66–73.
24. O’Driscoll, SW. Atraumatic instability: pathology and pathogenesis. In: Matsen FA, III., Fu FH, Hawkins RJ, eds. The Shoulder: A Balance of Mobility and Stability. Rosemont, IL: American Academy of Orthopaedic Surgeons; 1993:305–308.
25. Te Slaa, R, Lim, T. Multidirectioneie instabiliteit van de schouder; een nieuwe vorm van chronische schouderinstabiliteit. Ned Tijdschr Geneeskd. 1992; 136(32):1560–1563.
26. Rowe, CR, Recurrent transient anterior subluxation of the shoulder. The dead arm syndrome. Clin Orthop Rel Res 1987; 223:11–19. ![]()
27. Glousman, R, Instability versus impingement syndrome in the throwing athlete. Orthop Clin North Am. 1993;24(1):89–99. ![]()
28. Fu, F, Harner, C, Klein, A, Shoulder impingement syndrome. Clin Orthop Rel Res 1991; 269:162–173. ![]()
29. Schenk, TJ, Brems, JJ, Multidirectional instability of the shoulder: pathophysiology, diagnosis, and management. J Am Acad Orthop Surg. 1998;6(1):65–72. ![]()
30. Jobe, F, Giangarra, C, Kvitne, R, Anterior capsullabral reconstruction of the shoulder in athletes in overhand sports. Am J Sports Med 1991; 19:428–434. ![]()
31. Neviaser, R, Neviaser, T, Neviaser, J, Anterior dislocation of the shoulder and rotator cuff rupture. Clin Orthop Rel Res 1993; 291:103–106. ![]()
32. Silliman, J, Hawkins, R, Classification and physical diagnosis of instability of the shoulder. Clin Orthop Rel Res 1993; 291:7–19. ![]()
33. Kvitne, RS, Jobe, FW, The diagnosis and treatment of anterior instability in the throwing athlete. Clin Orthop 1993; 291:107–123. ![]()
34. Hawkins, RJ, Bokor, DJ, Clinical evaluation of shoulder problemsRockwood CA, Matsen FA, eds. The Shoulder. WB Saunders: Philadelphia, 1990. ![]()
35. Hamner, DL, Pink, MM, Jobe, FW, A modification of the relocation test: arthroscopic findings associated with a positive test. J Shoulder Elbow Surg 2000; 9:263–267. ![]()
36. Burkhart, SS, Morgan, CD, Kibler, WB, The disabled throwing shoulder: spectrum of pathology, part two: evaluation and treatment of SLAP lesions in throwers. Arthroscopy 2003; 19:531–539. ![]()
37. Sauers, EL, Borsa, PA, Herling, DE, et al, Instrumented measurement of glenohumeral joint laxity and its relationship to passive range of motion and generalized joint laxity. Am J Sports Med 2001; 29:143–150. ![]()
38. Harryman, DT, Sidles, JA, Harris, SL, et al, Laxity of the normal glenohumeral joint: a quantitative in vivo assessment. J Shoulder Elbow Surg 1992; 1:66–76. ![]()
39. Gerber, C, Ganz, R, Clinical assessment of instability of the shoulder. J Bone Joint Surg Br 1984; 66:551–556. ![]()
40. Matsen, FA, III., Lippitt, SB, Sidles, JA, Harryman, DT, II. Practical Evaluation and Management of the Shoulder. Philadelphia: Saunders; 1994.
41. Zarins, B, McMahon, M, Rowe, C, Diagnosis and treatment of traumatic anterior instability of the shoulder. Clin Orthop Rel Res 1993; 291:75–84. ![]()
42. Magarey, M, Jones, M. Clinical diagnosis and management of minor shoulder instability. Aust Physio. 1992; 38(4):269–280.
43. Altchek, DW, Warren, RF, Skyhar, MJ, et al, T-plasty modification of the Bankart procedure for multidirectional instability of the anterior and inferior types. J Bone Joint Surg. 1991;73(1):105–112. ![]()
44. Czitfer, E, Habel, T, Kepes, P, Posterior shoulder dislocation: pitfalls and perils. Orthopedics. 1993;16(1):97–99. ![]()
45. Pollock, R, Bigliani, L, Recurrent posterior shoulder instability. Clin Orthop Rel Res 1993; 291:85–96. ![]()
46. An, YH, Friedman, RJ, Multidirectional instability of the glenohumeral joint. Orthop Clin North Am. 2000;31(2):275–285. ![]()
47. Helmig, P, Sojbjerg, J, Kjaersgaard-Andersen, P, et al, Distal humeral migration as a component of multidirectional shoulder instability. Clin Orthop 1990; 252:139–143. ![]()
48. Rokous, JR, Feagin, JA, Abbott, HG, Modified axillary roentgenogram: a useful adjunct in the diagnosis of recurrent instability of the shoulder. Clin Orthop 1972; 82:84–86. ![]()
49. Engebretsen, L, Craig, L, Radiologic features of shoulder instability. Clin Orthop Rel Res 1993; 291:29–44. ![]()
50. Burkhead, WZ, Jr., Rockwood, CA, Jr., Treatment of instability of the shoulder with an exercise program. J Bone Joint Surg. 1992;74A(6):890–896. ![]()
51. Kamkar, A, Irrgan, JJ, Whitney, SL, Nonoperative management of secondary shoulder impingement syndrome. J Orthop Sports Physical Therapy 1993; 17:212–224. ![]()
52. Terry, GC, Hanimon, D, France, P, Norwood, L, The stabilizing function of passive shoulder restraints. Am J Sports Med 1991; 19:26–34. ![]()
53. Jobe, F, Moynes, D, Brewster, C, Rehabilitation of shoulder joint instabilities. Orthop Clin North Am. 1987;18(3):473–482. ![]()
54. Oveson, J, Nielsen, S, Anterior and posterior instability: a cadaver study. Acta Orthop Scand 1985; 57:324–327. ![]()
55. Oveson, J, Nielsen, S, Posterior instability of the shoulder: a cadaver study. Acta Orthop Scand 1985; 57:436–439. ![]()
56. Miniaci, A, MacDonald, P, Open surgical techniques in the athlete’s shoulder. Clin Sports Med. 1991;1O(4):929–954. ![]()
57. O’Driscoll, S, Evans, D, Long-term results of staple capsulorrhaphy for anterior instability of the shoulder. J Bone Joint Surg. 1993;75A(2):249–258. ![]()
58. Roberts, SN, Taylor, DE, Brown, JN, Hayes, MG, Saies, A, Open and arthroscopic techniques for the treatment of traumatic anterior shoulder instability in Australian rules football players. J Shoulder Elbow Surg. 1999;8(5):403–409. ![]()
59. Tibone, J, Bradley, J, The treatment of posterior subluxation in athletes. Clin Orthop Rel Res 1993; 291:124–137. ![]()