Range of movement
How do I assess range of movement?
AROM
AROM should be assessed before the PROM is explored.
Therapist
The therapist will already have observed the patient’s general AROM during the performance of functional activities (S3.18). However, as function involves the combined movement of many joints, a more specific assessment of the individual segments involved may be required. Assessment of all the cardinal planes of movement should be considered although clinical judgement should be used as to whether it is necessary to assess every joint and every direction. For example, at the hip the cardinal planes are flexion, extension, abduction, adduction and medial/lateral rotation.
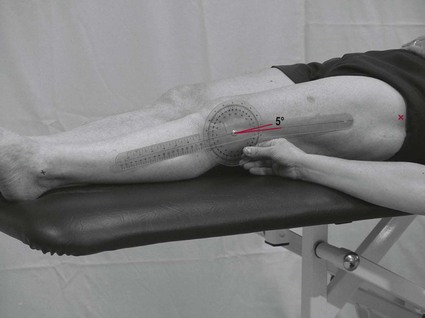
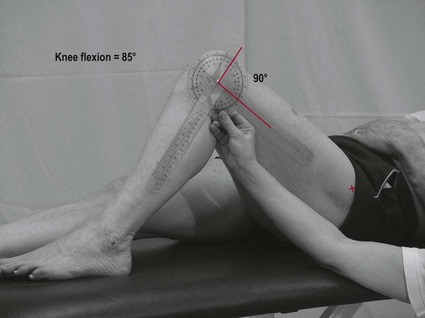
Limb testing
1. Stand-by assistance or a plinth alongside the patient may be necessary during assessment of the lower limb.
2. The test should be carried out one limb at a time (the unaffected limb first if this is relevant) and measurements taken using a universal goniometer.
3. Choose the appropriate size goniometer for the joint being measured.
4. Demonstrate the movement to ensure the movement is performed correctly.
5. Position the patient to allow FROM.
6. In the start position, place the axis of the goniometer (centre of protractor) over the joint (Fig. 28.1).
7. Line up the stationary arm of the goniometer with a proximal bony landmark that will not move during the limb movement (Fig. 28.1).
8. Line up the moveable arm with a bony landmark on the limb that will be moving (Fig. 28.1).
9. Ask the patient to perform the limb movement.
10. At the limit of the patient’s ROM, move the moveable arm to line up with the original bony landmark and take the reading (Fig. 28.2).
11. Be sure to read the correct scale from the protractor.
12. The therapist may choose to carry out a repeated movement if the test range is reduced. This may elicit a change in the AROM, an increase as they warm up or a decrease as they fatigue.
Spinal joint testing
1. The patient starts in neutral standing.
2. Make three marks (Fig. 28.3):
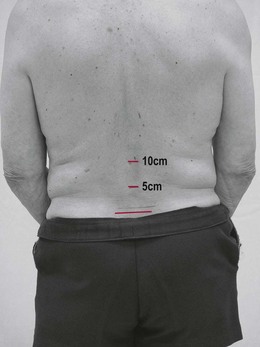
Figure 28.3 Measuring spinal joint ROM: start position.
3. Ask the patient to move to the finish position (e.g. spinal flexion).
4. At the finish position, re-measure the distances from the posterior superior iliac spine/s (PSIS) level and record (Fig. 28.4).

Figure 28.4 Measuring spinal joint ROM: finish position.
5. The same procedure can be repeated for extension and side flexion.
Note: Spinal measurements can also be taken from the tip of the third finger to the floor.
Does the patient achieve full active range of movement? This requires the therapist to know the normal values for full AROM of all joints.
Is the AROM excessive or reduced from normal limits?
Is the movement pattern normal? Gross movement patterns may indicate spasticity (S3.21).
Is there any evidence of pain behaviour prior to, during or after the movement? Nociceptive pain may present as avoidance in all or part of the range, facial grimace or verbalization of pain. Neurogenic pain may show no particular link to movement (S3.29).
Are there any compensatory movements used to achieve the range of movement? Compensatory activity may be used in circumstances where the usual muscle/s is/are unable to complete the task (hypotonia, hypertonia, weakness) or the range of the joint is altered (soft tissue adaptation).
PROM
Therapist
Limb testing
1. The therapist should explain that the movement is to be performed entirely by the therapist.
2. Hold the limb firmly and confidently to allow the patient to relax fully.
3. The therapist should move each segment through the full available ROM.
4. Once the therapist considers they have reached the limit of the patient’s ROM, a measurement should be taken accurately and objectively using a universal goniometer. However, more experienced therapists do use visual estimation. Instructions for the correct use of a goniometer are as for AROM.
Can the therapist achieve full passive range of movement? This requires the therapist to know the normal values for full PROM for all joints.
Is the range of PROM different to that of the AROM? Yes. See analysis section.
Is there any evidence of pain behaviour prior to, during or after the movement? Nociceptive pain may present with guarding/muscle spasm during the testing of PROM. Neurogenic pain may show no particular link to movement (S3.29).
End feel
1. At the end of the available range the therapist should apply overpressure to the joint in the same direction as the test movement.
2. This additional force must be applied slowly, smoothly and accurately.
3. The therapist should compare the end feel with what they understand to be the normal end feel for that joint. The normal end feels are different according to the structures limiting the joint (Magee 2006).
Analysis
The therapist’s analysis of ROM will inform other areas of the objective assessment. For example, reduced AROM of the ankle dorsiflexors may explain abnormal gait and poor balance. The aim of this assessment tool is to establish the patient’s ROM and to begin hypothesizing about any possible limiting factors. In the case of a reduced ROM, this can be achieved by comparing the findings from both AROM and PROM assessments. For example, if PROM is greater than AROM then a deficit of muscle contraction should be suspected. This could be caused by muscle weakness, hypotonia, hypertonia or sensory loss. However, if both PROM and AROM are reduced, the limit is more likely to be linked with a soft tissue adaptation. Note: Pain could be a causal factor in both these scenarios and needs further investigation (S3.29).
References and Further Reading
Fox, J, Day, R. A physiotherapist’s guide to clinical measurement. Edinburgh: Churchill Livingstone/Elsevier; 2009.
Magee, DJ. Orthopaedic physical assessment, ed 4. Canada: Elsevier Sciences; 2006.
Petty, NJ. Neuromusculoskeletal examination and assessment: a handbook for therapists. Edinburgh: Churchill Livingstone; 2006.