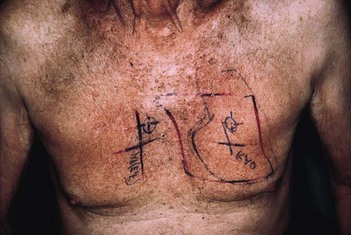
172 Radiotherapy marks
Patient 2
Advanced-level questions
What modalities may be used to minimize the side effects of radiation?
• Rendering the tumour more sensitive to radiotherapy by prior chemotherapy, thereby reducing the dose
• Regional hypothermia (40–42°C), particularly in superficial tumours and relatively bulky non-vascular tumours
• Radiolabelled antibodies, which deliver high levels of radiation locally to the tumour bed.
In which conditions is radiotherapy beneficial?
Malignant conditions
• Radiotherapy as the sole agent with a curative intent in Hodgkin’s disease, some neoplasms of brain and spinal cord, oral cavity, pharynx, oesophagus, laryngeal tumours (permitting cure without loss of voice), tumours of cervix and vagina cavity
• Radiation with surgery in cancers of lung, breast, urinary bladder, seminomas, ovary, uterus, sarcomas of soft tissue and testicular seminomas
• Radiation as adjuvant to chemotherapy in lymphomas, lung cancers and childhood cancers
• Radiation as palliative therapy for pain and or dysfunction in superior vena caval obstruction, dysphagia of terminal illness, upper airway obstruction, spinal cord compression and pericardial tamponade secondary to malignant pericardial tumours.
Non-malignant conditions
• Rheumatoid arthritis (total lymphoid irradiation is an experimental therapeutic procedure)
• Ankylosing spondylitis, where local external irradiation of an involved peripheral joint or injected radiation synovectomy can be valuable in ameliorating pain and allowing mobility. Spinal irradiation is no longer used because of the risk of haematological malignancy.
What are the side effects of radiotherapy?
• Acute toxicity: systemic symptoms including malaise, fatigue, anorexia, nausea and vomiting, diarrhoea and local skin and mucosal changes. Bone marrow suppression may occur following irradiation to the pelvis and long bones
• Long-term toxicity: cutaneous hyperpigmentation, impaired function of irradiated viscera, bone necrosis, myelopathy and secondary malignancies.