Chapter 3 Radiologic Anatomy of the Spine
The cervical spine
Atlas (C1)
The lateral masses consist of superior and inferior articular facets and transverse processes. The superior articular facets are concave and ovoid, and they face upward and inward as shallow foveae for articulation with the occipital condyles. Nutatory movements of the head mainly occur at these atlantooccipital joints. The inferior articular facets are concave and face downward, slightly medially, and backward; they articulate with the superior articular facets of the axis. The relative horizontal orientation of the atlantoaxial facet joints allows rotation at the expense of bony stability. The paired alar ligaments, running from the posterolateral aspects of the odontoid process to the occipital condyles, prevent excessive rotation [1]. The transverse processes are each pierced by a foramen for the vertebral artery. On coronal CT scans, the occipitoatlas and the atlantoaxial joints resemble a capital X.
C3 to C7 Vertebrae
Vertebral Bodies
The vertebral bodies in the cervical spine are ladder-like in cross section; they are broader in the transverse diameter than in the anteroposterior (AP) dimension, and their end plates are parallel (Fig. 3-1). The cervical vertebral bodies are smaller than those of the other movable vertebrae and increase in size from C3 downward. The vertebrae are connected by the anterior and posterior longitudinal ligaments. Each ligament’s fibers diverge at each disc level and blend with the anulus fibrosus and the adjacent margins of the vertebral bodies. At the mid-vertebral level, the posterior longitudinal ligament is narrower and lies behind the body, posterior to the retrovertebral venous plexus.
Joints of von Luschka
The upper and lateral edges of the superior surface project upward and have sagittal ridges that form the uncinate processes. Together with corresponding notches in lower end plates of the vertebra above, they form the uncovertebral joints of von Luschka (Fig. 3-2).
Transverse Foramen
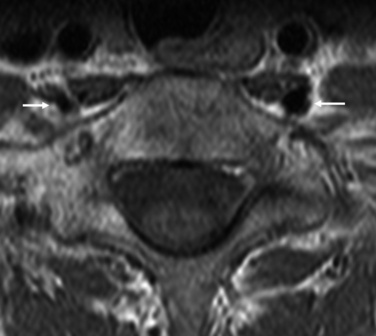
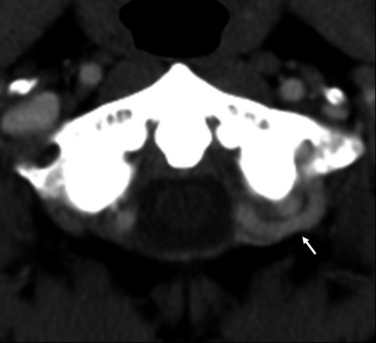
The transverse foramen, a characteristic feature of the cervical spine, houses the vertebral artery, veins, and sympathetic nerves in the deep cranial groove of the transverse process. The spinal nerves and ganglia cross the dorsal border of the artery along with segmental vessels. The transverse foramen of the seventh cervical vertebra contains only vertebral veins, not the vertebral artery (Figs. 3-3 and 3-4).
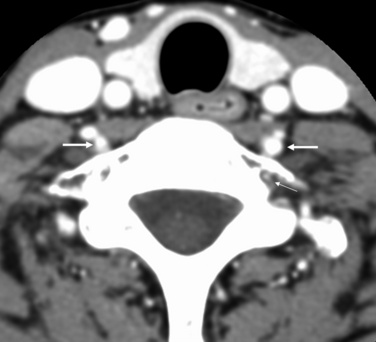
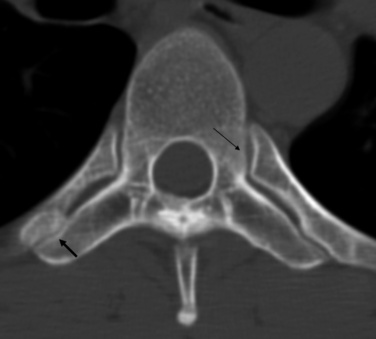
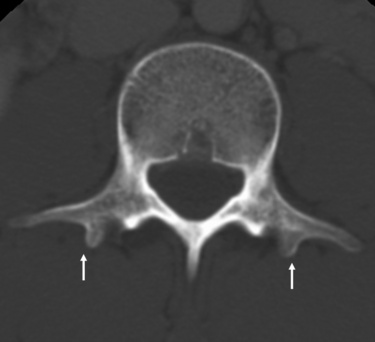
Figure 3–3 Axial CT scan of the seventh cervical vertebra. The transverse foramen of the seventh cervical vertebra contains only vertebral veins (thin arrow), not the vertebral artery (thick arrows). However, the other cervical vertebrae contain the vertebral artery within their transverse foramina. See also Fig. 3-4.
Articular Processes
The superior and inferior articular processes of adjacent neural arches form the facet joints. These structures are more oblique in the cervical level than in other levels of the spine. Each joint surface is lined with articular cartilage, and menisci cushion the cervical facets. Surrounding each joint is a fibrous capsule with a synovial membrane on its inner aspect; this capsule is relaxed to allow a gliding motion. Anteriorly, the superior articular facet is rounded in its anterior aspect; its articular surface faces posteriorly and is flat. Posteriorly, the inferior articular facet of the vertebra above has a flat anterior articular surface and a convex posterior aspect (Fig. 3-5).
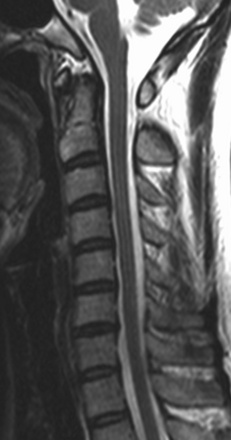
Spinal Canals
The spinal canals are relatively large in order to house the cervical enlargement of the spinal cord. The spinal canal is triangular with the apex of the triangle posterior. The canal decreases in size from vertebra C1 through vertebra C3 and has a fairly uniform dimension from C3 through C7. C7 is a transitional vertebra, whose spinous process is longer and thicker and has a more inferior tilt than the more rostral cervical spinous processes of C3 to C6. On a T1-weighted MR image, the exact size of the subarachnoid space is difficult to assess because of its low signal intensity, and it may be confused with the posterior longitudinal ligament and the cortical bone (Fig. 3-6).
Epidural Space
The epidural space that surrounds the dural sac contains neurovascular and connective tissue elements that are more clearly seen on MRI and CT after intravenous injection of a contrast agent. There is only a small amount of epidural fat tissue, and sinuses are formed in this fat tissue by the wide venous plexuses that surround roots and nerves as they leave the intervertebral foramina in the lateral parts of the epidural space (Fig. 3-7). The scarcity of revised epidural fat in the cervical canal in comparison with that in the lumbar canal makes it more difficult to differentiate between the soft tissue structures in the cervical spinal canal on a noncontrast CT scan. On MRI, the high signal intensity in the anterior lateral aspect of the cervical canal represents the epidural venous plexus. The epidural venous plexuses produce high signal intensity in the anterior epidural space, which should not be confused with epidural fat; epidural fat is virtually absent at the cervical level.
Cervical Discs
The cervical intervertebral discs are smaller than the discs of other regions of the spine. The uncinate processes on the upper end plate limit lateral extension of the discs. These discs are wedge-shaped, the greater width being anterior, corresponding to the cervical lordosis [2]. The intervertebral discs do not extend anteriorly or posteriorly beyond the level of the vertebral body in younger people. The nucleus pulposus cannot be differentiated from the anulus fibrosus, but the periphery of the disc is less intense than its central portion. (Figs. 3-6 and 3-8).
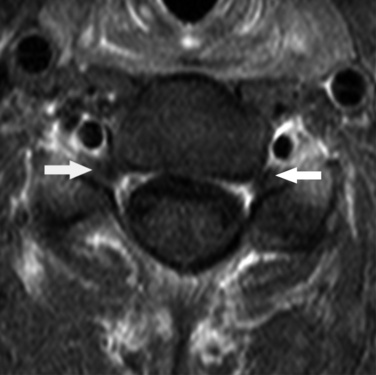
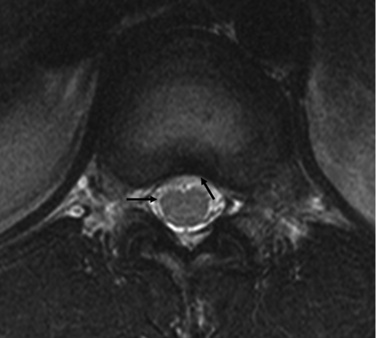
Nerves of the Cervical Cord
Spinal nerves arise from the cervical cord. Each nerve consists of a dorsal sensory root and a ventral motor root. The nerve roots join just lateral to the dural sheath to form the spinal nerves. The dorsal root ganglion is located in the neural foramen just proximal to the point of union of the dorsal and ventral roots. The roots of each spinal nerve from C1 through C7 leave the spinal canal through the intervertebral foramina above the corresponding vertebra. The eighth cervical nerve passes through the foramen between C7 and T1. The spinal ganglion, located outside and below the neural foramen, is clearly seen posterior to the vertebral artery on MRI as a structure of intermediate signal intensity. On contrast-enhanced MR images, the spinal ganglion appears as a mildly enhancing ovoid structure posterior to the vertebral artery (Fig. 3-9).
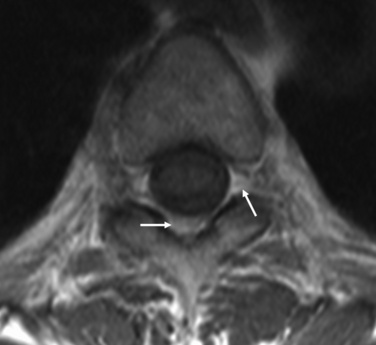
Vertebral Arteries
The vertebral arteries usually enter the foramina at the C6 level but may enter at C5 or C7, and they exit the foramina in the area of the transverse process of the atlas; they wind around the lateral masses, passing in a group just posterior to the superior articular facet, from the cranial surface to the posterior arch [3]. The two vertebral arteries penetrate the dura and are well demonstrated on each side of the medulla on contrast-enhanced CT. Within the transverse foramen (Fig. 3-10), the vertebral artery is of low signal intensity (Fig. 3-11), and the vertebral vein of high signal intensity, on MRI. The vertebral vein surrounds the vertebral artery.
Venous Plexus
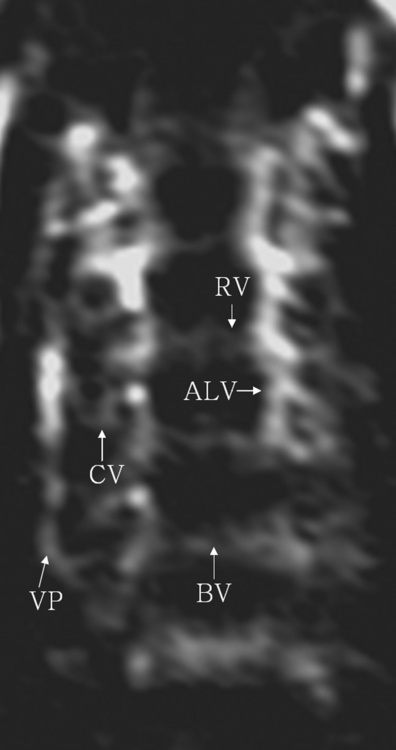
The cervical epidural venous plexus is an extensive sinusoidal network in the cervical epidural space; it consists of medial and lateral longitudinal channels in the anterolateral portion of the epidural space. The medial and lateral longitudinal channels are connected behind each vertebral body by retrocorporeal veins that communicate with the basivertebral venous system at the midportion of each vertebral body, as follows (Fig. 3-12):
This system is an intricate, lattice-like network composed of slowly flowing blood [3]. The veins can be seen on both sagittal and axial MR images as areas of increased signal intensity. Parasagittal views demonstrate them best in the anterolateral recess of the cervical spinal canal. Increased intensity denotes slow to stagnant venous flow. Axial images show these segmented longitudinal bandlike channels as areas of high signal intensity in the anterolateral recess of the spinal canal. Though often seen on noncontrast studies, the epidural venous plexus can be unclear, depending on the direction and velocity of blood flow. It is more consistently and accurately depicted after the administration of gadolinium-DTPA, which produces a uniformly high signal intensity of the epidural venous structures outside the extradural space, along the anterolateral aspects of the spinal canal and neural foramina.
The thoracic spine
The 12 thoracic vertebrae are intermediate in size between the smaller cervical and larger lumbar vertebrae. The vertebral bodies and their discs have an inverted heart shape in cross section. The end plates of the vertebral bodies are flat, and the nuclei pulposi are more centrally located than in the lumbar discs. The thickness and the horizontal dimensions of the thoracic discs increase caudally. Although the thoracic discs are of larger volume than the cervical discs, they are thinner vertically than cervical and lumbar discs (Fig. 3-13). The thoracic vertebrae are characterized by costal facets on both sides of the bodies and on all the transverse processes except those of the 11th and 12th thoracic vertebrae, which articulate with facets on the heads and tubercles, respectively, of the corresponding ribs (Fig. 3-14).
Pedicles
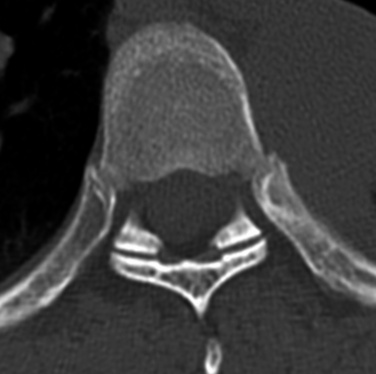
The stout pedicles of a thoracic vertebra arise from the upper half on the dorsum of the body and pass posterolaterally and slightly inferiorly to the articular pillar and posterior neural arch. On axial MR images or CT scans, the facet joints demonstrate a coronal orientation (Fig. 3-15).
Laminae
The laminae are short and relatively thick. They pass from the articular pillars in a medial and posterior direction. They partly overlap each other from T1 downward (see Fig. 3-14).
Intervertebral Foramen
The intervertebral foramen, smaller and more rounded than in the cervical region, is directed laterally at the inferior half of the vertebral body. Its margins are formed by the pedicles superiorly and inferiorly, the vertebral body anteriorly, the neck of the rib anterolaterally, and the facet joints posteriorly. The nerve roots, surrounded by the abundant foraminal fat, are of intermediate signal intensity (Fig. 3-16).
Spinal Canal
The spinal canal is ovoid in cross section, with a relatively large anteroposterior diameter. Epidural fat is abundant posteriorly between the neural arch and the dura, and laterally in the intervertebral foramen. It is, however, less abundant in the anterior half of the epidural space than in the lumbosacral region. The posterior epidural fat demonstrates high signal intensity on T1-weighted and T2-weighted MR images (Figs. 3-17 to 3-19). The posterior longitudinal ligament is difficult to differentiate from the dural sac. Venous sinuses widely occupy the lateral recesses and intervertebral foramina.
The lumbar spine
Transverse and Accessory Processes
The flat transverse processes run laterally and slightly posteriorly from the junction of the pedicle (Fig. 3-20). The thick, rounded fifth transverse process sometimes articulates with the iliac bones but also can be fused with the ilium.
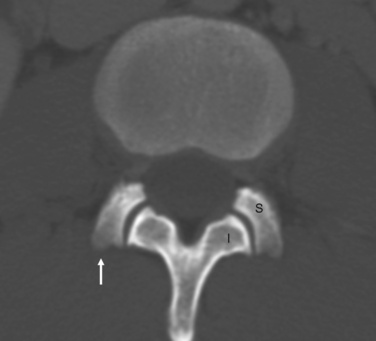
Articular and Mammillary Processes
The superior articular processes project vertically upward from the articular pillars between the pedicles and the laminae. The concave facet of each superior articular process faces dorsomedially to the inferior articular facets of the vertebra above it (Fig. 3-21). At the inferior aspect of the intervertebral foramen, the superior articular facet becomes contiguous with the pedicle below to form the posterior border of the lateral recess. At this point, the traversing nerve root lies medial to the pedicle, anterior to the superior articular facet, and posterior to the vertebral body and disc [4,5]. The inferior articular processes run downward and slightly laterally from the laminae. Their articular surfaces face ventrolaterally to the superior articular facets of the vertebrae below them. The articular plane is curvilinear.
The mammillary processes project backward from the superior articular process and are short and round for the attachment of muscles (see Fig. 3-21).
Intervertebral Foramina
The intervertebral foramina are defined anteriorly by the posterior vertebral bodies and disc, superiorly and inferiorly by the pedicles, and posteriorly by the articular processes. The intervertebral foramina are the largest in the lumbar area. The spinal ganglia, the spinal branch of the segmental artery, and the sinuvertebral nerve are located in the upper portion of each intervertebral foramen, and the intervertebral veins in the lower portion (Figs. 3-22 and 3-23).
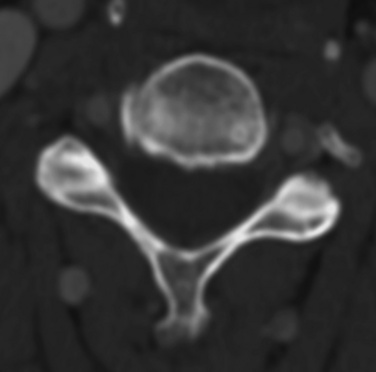
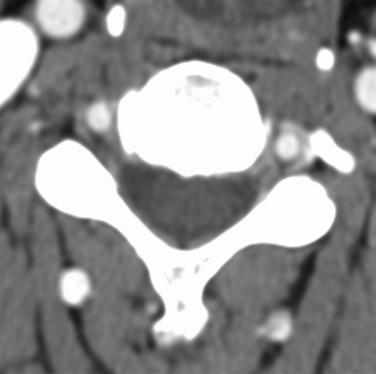
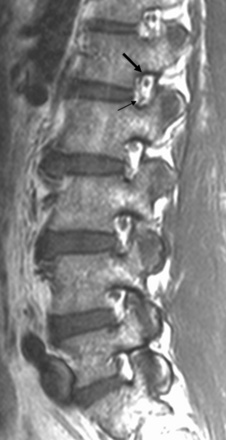
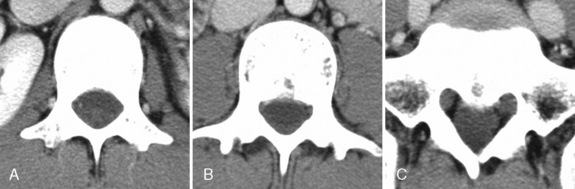
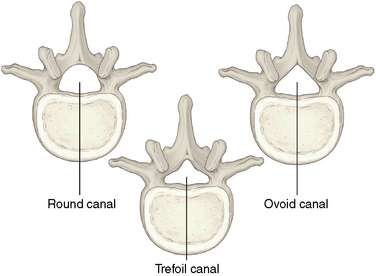
Spinal Canal
The spinal canal, which is round or oval at L1, is increasingly triangular toward the lower lumbar vertebrae. It takes on a V shape at the S1 level (Fig. 3-24, 3-25).
Epidural Space
The epidural space between the dura and the bones of the spinal canal contains epidural fat, spinal nerves, blood vessels, and ligaments. The epidural fat space is prominent ventral to the dura at the mid-body level of the lumbar vertebrae, especially L5-S1 (Fig. 3-26). The abundant epidural fat makes it easy to differentiate other structures, such as the nerve roots, the venous plexus, and the margin of the discs, on CT and MRI.
Ligaments of the Lumbar Spine
The posterior longitudinal ligament covers the posterior vertebral bodies with some space for the vascular structures. At the level of the intervertebral discs, it attaches tightly to the posterior surface of the anuli of the discs. The ligamentum flavum is 5 mm thick and extends from the anteroinferior border of the lamina above to the upper posterior border of the lamina below. The ligamentum flavum is hyperintense to the bony cortex of the lamina on T1-weighted MR images (Fig. 3-27). Laterally its fibers blend with the thick medial and superior portions of the facet capsule. The anterolateral extension of the ligamentum flavum fuses laterally with the medial portion of the facet joint capsule to reinforce the capsule [6].
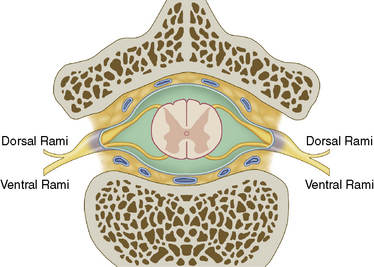
Nerves of the Lumbar Spine
The lumbar spinal nerve roots lie in the lateral recess and extend to the medial border of the superior articular facet at the lower portion of the vertebral foramen of the level above. The nerves then pass laterally below the pedicle and enlarge to form the dorsal ganglion (see Fig. 3-27). From the ganglion, the peripheral nerves exit laterally out the vertebral foramen.
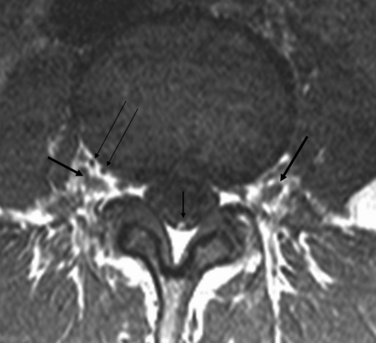
The nerve roots, which are smaller ventrally and larger dorsally, exit through an intervertebral foramen. The dorsal root becomes the spinal ganglion in the lateral portion of the intervertebral foramen (see Fig. 3-27). Lying together, they pierce the dura and unite to form a spinal nerve. The spinal nerves are interconnected with adjacent sympathetic trunk ganglia by rami communicantes, providing an explanation for the mutual overlapping of segmental sensory nerve distribution. Small recurrent meningeal branches originate from the spinal nerves shortly after emerging from the intervertebral foramina, and they innervate the meninges and their vessels. Then the spinal nerves divide into the ventral and dorsal rami. The ventral rami supply the anterior and lateral parts of the trunk. The dorsal rami turn backwards to supply the cutaneous and muscular regions and the facet joints (Fig. 3-28).
Lumbar Venous Plexus
The epidural venous plexus appears as punctuate foci of low signal intensity within the hyperintense epidural fat (see Fig. 3-27).
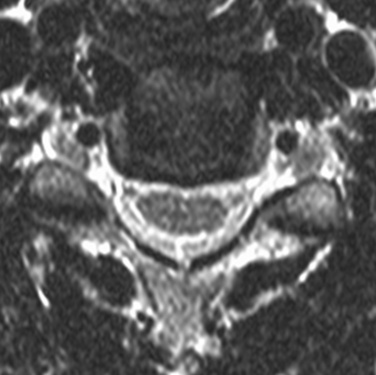
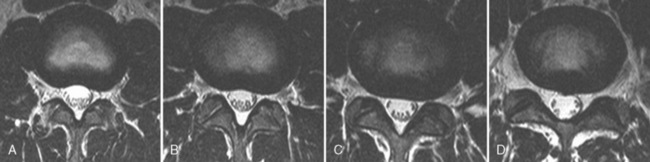
Lumbar Disc
The intervertebral disc in the lumbar region has three parts: the cartilaginous end plate, the anulus fibrosus, and the nucleus pulposus [7]. The intervertebral discs are thickest in the lumbar region. Lumbar lordosis is due to the increase in differential between the anterior and posterior thicknesses of the discs, a situation that makes the lumbosacral disc the most wedge shaped [8]. On axial sections, the upper four lumbar discs have a slightly concave or flat posterior border, conforming to the adjacent V-shaped bodies. The fifth lumbar disc, however, has a flatter, slightly convex posterior border (Fig. 3-29).
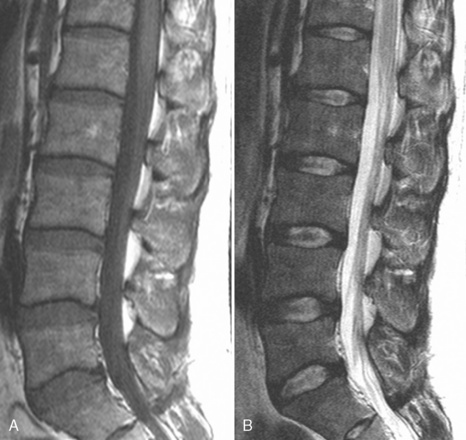
The nucleus pulposus is composed of very hydrated and loose fibrous strands with the consistency of a gel. The nucleus pulposus usually blends with the anulus fibrosus without demarcation between the two. The nucleus consists of 85% to 90% water, and the anulus 80% water [9]. On T1-weighted MR images, the nucleus pulposus and the anulus fibrosus show slightly lower signal intensity and they cannot be separated (Fig. 3-30). On T2-weighted MR images, however, the nucleus pulposus demonstrates high signal intensity and the anulus demonstrates low signal intensity. However, the central cleft is low in intensity on T2-weighted MR images owing to the abundance of collagen fiber.
The cortical bone shows markedly low signal intensity and is easy to differentiate from the hyperintense bone marrow. The disc is hyperdense to the psoas muscle on CT (see Fig. 3-26).
1 Fielding J.W., Hawkins R.J. Atlanto-axial rotatory fixation. J Bone Joint Surg Am. 1977;59:37-44.
2 Parke W.W., Schiff D.C.M. The applied anatomy of the intervertebral disc. Orthop Clin North Am. 1971;2:309-324.
3 Flannigan B.D., Lufkin R.B., McGlade C., et al. MR imaging of the cervical spine: Neurovascular anatomy. AJR Am J Roentgenol. 1987;148:785-790.
4 Dorwart R.H., Sauerland E.K., Haughton V.M., et al. Normal lumbar spine. In: Newton T.H., Potts D.G., editors. Computed Tomography of the Spine and Spinal Cord. San Anselmo, CA: Clavadel; 1983:93-114.
5 Schnitzlein H.N., Murtagh F.R. Imaging Anatomy of the Head and Spine. Baltimore: Urban & Schwarzenberg, 1985.
6 Grenier N., Kressel H.Y., Schiebler M.L., et al. Normal and degenerative posterior spinal structures: MR imaging. Radiology. 1987;165:517-525.
7 Coventry M.B. Anatomy of the intervertebral disc. Clin Orthop Relat Res. 1969;67:9-15.
8 Parke W.W., Schiff D.C.M. The applied anatomy of the intervertebral disc. Orthop Clin North Am. 1971;2:309-324.
9 White A.A., Gordon S.L. Synapsis: Workshop on idiopathic low-back pain. Spine. 1982;7:141-149.