Chapter 22 Radiofrequency volumetric reduction for hypertrophic turbinate
1 INTRODUCTION
Inferior turbinate hypertrophy can be caused by generalized nasal mucosal diseases in allergic and vasomotor rhinitis, as well as compensatory enlargement due to a long-standing septal deviation.1–3 Medical treatments such as topical corticosteroid sprays, antihistamines and allergic desensitization are usually the first-line therapy. However, these treatment modalities may be inadequate in achieving significant resolution of nasal obstruction. Surgical reduction of the hypertrophic inferior turbinate has been advocated after failure of medical therapy. The surgical techniques usually involve resection in the form of partial or total turbinectomy with electrocautery, scissors, or laser.4–8 Although successful outcomes following these procedures are often reported, the associated complications including pain, bleeding, crusting, dryness, infection, adhesion, foul odor and the need for nasal packing are also well known. Furthermore, most of these techniques result in mucosal injury, thus potentially affecting the nasal physiology.
Radiofrequency (RF) volumetric reduction uses RF energy to create submucosal tissue injury leading to the reduction of tissue volume. Li et al.9 first reported the use of RF for the treatment of hypertrophic inferior turbinate. This article describes the author’s technique of RF reduction for turbinate hypertrophy.
2 TECHNIQUE
| Candidates: | Any patient with hypertrophic inferior turbinates resulting in nasal obstruction. |
| Diagnosis: | Anterior rhinoscopy and possibly nasal endoscopy. |
| Facility: | Outpatient-office setting. |
| Anesthesia: | Cotton ball (saturated with 2% lidocaine without epinephrine) applied to the anterior aspect of the inferior turbinate for 1 minute followed by a local anesthetic injection (2–3 milliliters of 2% lidocaine without epinephrine). |
| Temperature: | 85 °C. |
| Energy: | 300–600 joules per lesion. |
| Tx site: | Anterior one-third to one-half of the inferior turbinate. |
| Tx number: | 1–2 lesions per turbinate. |
| Post tx: | Cotton ball applied to the puncture site for 2 minutes. |
| Post op: | No restriction, over-the-counter analgesics as needed. |
| Recovery: | Increased nasal obstruction for 2–5 days. |
| Improvement: | 10–14 days following treatment. |
2.1 DESCRIPTION OF TECHNIQUE
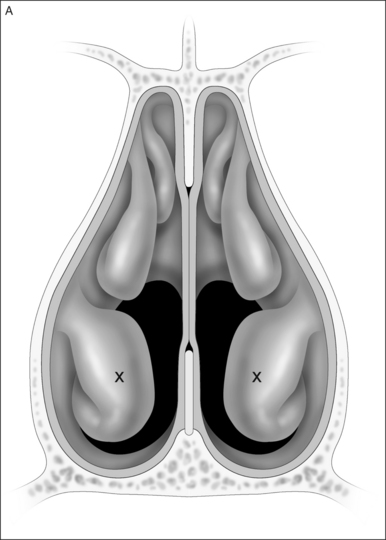
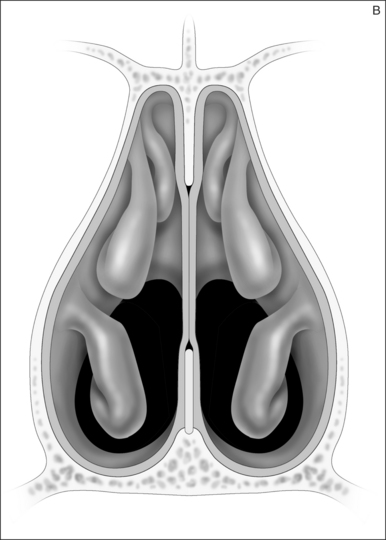
The procedure is routinely performed in an office setting. Treatment begins with topical anesthetic (cotton swab saturated with 2% lidocaine without epinephrine) applied to the anterior aspect of the inferior turbinate for 1 minute followed by a local anesthetic injection (3 milliliters of 2% lidocaine without epinephrine). The RF needle electrode (Gyrus Medical, Minneapolis, MN) containing a 10 mm active length is inserted 12 mm submucosally into the anterior head of the inferior turbinate (Fig. 22.1). Care should be taken not to breach the mucosa posterior to the puncture site. The settings on the RF generator include energy delivery (range 400–700 joules) and temperature (85 °C). In general, only one treatment is required per turbinate and 300–600 joules are delivered. Obviously, the amount of energy delivered is related to the size of the turbinate. Occasionally, if the turbinate is extremely large, two treatments per turbinate can be given. Immediately following the procedure, a cotton ball is applied over the puncture site for 2 minutes, and the patient is discharged without restrictions on normal daily activities. No nasal packing, topical ointment, steroids or nasal spray are required. Occasionally, patients may complain of burning sensation at the treated area. This is well managed with any over-the-counter analgesics.
3 DISCUSSION
RF turbinate reduction has been extensively published. The most widely used RF generator is by Gyrus Medical, which has the most literature support. Turbinate reduction while avoiding mucosal disruption is not a new concept. Submucosal diathermy has been the most commonly used technique. However, submucosal diathermy lacks well-established parameters for the energy requirement, thus could lead to unpredictable results and risks excessive tissue injury with complicatons.10,11 RF volumetric reduction of hypertrophic turbinate results in predictable tissue injury and minimizes potential complications due to the biophysics of RF energy. The controlled submucosal heating by the small turbinate probe reliably avoids mucosal injury, thus minimizing complications while reducing turbinate size.
The anterior third to half of the inferior turbinate was selected as the treatment site because this is the location of the nasal valve. Engorgement of the erectile turbinate tissue in this location significantly increases nasal resistance leading to nasal airway obstruction.12 Although greater improvement may be possible if treatment is extended toward the post-erior, the diminished visibility and increased energy delivery could increase mucosal injury. RF turbinate reduction reduces nasal obstruction and the postoperative discomfort and adverse effects are minimal.13–16 The improvement of nasal breathing appears to last on long-term follow-up.17,18 Furthermore, multiple studies have demonstrated that nasal physiology is unaltered after treatment.19
1. Mabry RL. Surgery of the inferior turbinates: how much and when? Otolaryngol Head Neck Surg. 1984;92:571-576.
2. Lai VWS, Corey JP. The objective assessment of nasal patency. Ear Nose Throat J. 1993;72:395-400.
3. Wood RP, Jafek BW, Eberhard R. Nasal obstruction. In: Bailey BJ, editor. Head and Neck Surgery – Otolaryngology. London: J.B. Lippincott; 1993:303-328.
4. Ophir D, Shapira A, Marshak G. Total inferior turbinectomy for nasal airway obstruction. Arch Otolaryngol Head Neck Surg. 1985;111:93-95.
5. Rejali SD, Upile T, McLellan D, Bingham BJ. Inferior turbinate reduction in children using Holmium YAG laser – a clinical and histological study. Laser Surg Med. 2004;34:310-314.
6. Wexler D, Braverman I. Partial inferior turbinectomy using the microdebrider. J Otolaryngol. 2005;34:189-193.
7. Elwany S, Harrison R. Inferior turbinectomy: comparison of four techniques. J Laryngol Otol. 1990;104:206-209.
8. Gupta A, Mercurio E, Bielamowicz S. Endoscopic inferior turbinate reduction: an outcomes analysis. Laryngoscope. 2001;111:1957-1959.
9. Li KK, Powell NB, Riley RW, Troell RJ, Guilleminault C. Radiofrequency volumetric tissue reduction for treatment of turbinate hypertrophy − a pilot study. Otolaryngol Head Neck Surg. 1998;119:569-573.
10. Woodhead CJ, Wickham MH, Smelt GJC, MacDonald AW. Some observations on submucous diathermy. J Laryngol Otol. 1989;103:1047-1049.
11. Williams HOL, Fisher EW, Holding-Wood DG. ‘Two-stage turbinectomy’: sequestration of the inferior turbinate following submucosal diathermy. J Laryngol Otol. 1991;105:14-16.
12. Haight SJ, Cole PH. The site and function of the nasal valve. Laryngoscope. 1983;93:49-55.
13. Utley DS, Goode RL, Hakim I. Radiofrequency energy tissue ablation for the treatment of nasal obstruction secondary to turbinate hypertrophy. Laryngoscope. 1999;109:683-686.
14. Smith TL, Correa AJ, Kuo T, Reinisch L. Radiofrequency tissue ablation of the inferior turbinates using a thermocouple feedback electrode. Laryngoscope. 1999;109:1760-1765.
15. Fischer Y, Gosepath J, Amedee RG, Mann WJ. Radiofrequency volumetric tissue reduction (RFVTR) of inferior turbinates: a new method in the treatment of chronic nasal obstruction. Am J Rhinol. 2000;14:355-360.
16. Lin HC, Lin PW, Su CY, Chang HW. Radiofrequency for the treatment of allergic rhinitis refractory to medical therapy. Laryngoscope. 2003;113:673-678.
17. Sapci T, Sahin B, Karavus A, Akbulut UG. Comparison of the effects of radiofrequency tissue ablation, CO2 laser ablation, and partial turbinectomy applications on nasal mucociliary functions. Laryngoscope. 2003;113:514-519.
18. Rhee CS, Kim DY, Won TB, et al. Changes of nasal function after temperature-controlled radiofrequency tissue volume reduction for the turbinate. Laryngoscope. 2001;111:153-158.
19. Porter MW, Hales NW, Nease CJ, Krempl GA. Long-term results of inferior turbinate hypertrophy with radiofrequency treatment: a new standard of care? Laryngoscope. 2006;116:554-557.