Chapter 67 Radiofrequency tonsil reduction: safety, morbidity and efficacy
1 INTRODUCTION
Tonsillectomy remains one of the most popular surgical procedures performed worldwide. Its role as a surgical strategy to widen the pharyngeal space for the treatment of obstructive sleep apnea/hypopnea syndrome (OSAHS) in pediatric patients still remains widely accepted, whereas its utility as a sole procedure for the same purpose in adults is quite limited.1 Tonsillectomy remains, however, an important adjunct procedure and an essential component of uvulopalatopharyngoplasty (UPPP). Over the years, many different techniques besides the classic cold knife dissection have arisen, all with variable results when it comes to decreasing the major morbidities of the procedure, such as pain, reduced activity level, hemorrhage, and postoperative decrease in fluid intake, leading to dehydration.
This mechanism is the rationale for developing techniques aimed at performing tonsil reduction without disrupting the capsule: the concept of subtotal capsule-sparing tonsil reduction. In pediatric patients, subtotal tonsil resection showed an earlier decrease in postoperative pain, decreased pain medication requirements, and an earlier return to diet, when compared to traditional total tonsillectomy.2 More recently, temperature-controlled radiofrequency was introduced as a much more effective and safe device for tonsil reduction. The underlying principle of temperature-controlled radiofrequency is the generation of a plasma field at the probe’s surface, which allows for tissue ablation at relatively low temperatures (40–70°C). This plasma field consists of highly ionized particles that break down the molecular bonds of local tissue with a reduction in heat dissipation to surrounding structures, as opposed to coagulation by diathermic methods, which generates temperatures greater than 500°C. The other advantage of the radiofrequency generator is that it can be used for bipolar coagulation, in order to achieve hemostasis during the procedure. The versatility of this technique consists of the ability to design different wands that can generate varying amounts of energy, depending on the need to ablate, to reduce the volume of tissue, or a combination of both. This is determined by the primary indication for tonsillectomy and the anatomical characteristics of the patient. The device can be used as a cutting tool to dissect along the capsular plane of the tonsil, much like a traditional tonsillectomy. It can also be used to create small channels in the tonsil in order to dissipate ionizing energy to the surrounding tissue, thereby causing tissue death days to weeks later. This then leads to shrinkage and tissue volume reduction due to the ensuing fibrosis. This variant, known as radio-frequency ablation, is not frequently performed any more, due to comparatively better results with coblation techniques. When the objective is to perform subtotal tonsil reduction, the instrument can be used to remove tonsillar tissue layer by layer, beginning at the exposed surface while avoiding the underlying capsule (radiofrequency coblation or cold ablation), thus causing significantly decreased morbidity. The difference between ablation and coblation lies in the mechanism of tissue destruction. Coblation primarily shrinks tissue by molecular disintegration (as opposed to heat-induced necrosis), operates at lower frequencies and voltage, and requires a conductive fluid (isotonic saline), which becomes ionized. Coblation of soft tissue produces immediate results, without the need for resorption of necrotic tissue. For this reason, coblation has largely replaced ablation techniques for the purpose of tonsil reduction.
In this chapter, we describe the techniques of total radio-frequency-assisted tonsillectomy and radiofrequency subtotal (capsule-sparing) tonsillectomy. Radiofrequency tonsillar ablation is also briefly mentioned.3
2 PATIENT SELECTION
In general, indications for tonsillectomy are updated on a regular basis by the American Academy of Otolaryngology – Head and Neck Surgery. The procedure is indicated for the reduction of chronically enlarged tonsils, when they are associated with obstructive sleep disordered breathing, particularly in children with associated failure to thrive.4 Other indications for tonsillectomy include recurrent streptococcal infection, peritonsillar abscess, and chronic cryptic tonsillitis. Relative contraindications for radiofrequency reduction techniques are asymmetrical tonsillar hypertrophy, clinical diagnosis or high suspicion of lymphoma, history of peritonsillar abscess, and repeated streptococcal infections (recurrent infectious tonsillitis). Such patients should undergo traditional total tonsillectomy, due to the need for complete removal of tonsillar tissue. Patients with chronic or recurrent non-streptococcal inflammatory cryptitis may also benefit from subtotal tonsil coblation.
3 SURGICAL TECHNIQUE (OUTLINE OF PROCEDURE)
3.1 TOTAL RADIOFREQUENCY-ASSISTEDTONSILLECTOMY
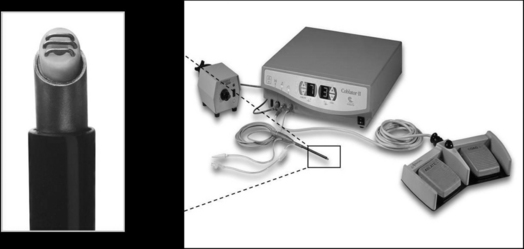
Coblation can be used for the traditional complete excision of the tonsils. Electrolyte solution is not injected, as coblation is a surface technique in which saline irrigation is utilized. Optimal coblation is achieved with an abundant flow of saline solution. The device used by our group is the Coblator II Surgery System with the EVAC™ 70 Plasma Wand (Arthrocare ENT, Sunnyvale, CA) (Fig. 67.1). Small vessels are sealed as the tissue is dissected, so hemostasis is very effective and efficient. More aggressive hemostasis can be performed if necessary, by operating the wand in the cautery mode. The coagulation setting used is usually 3 to 5. If larger vessels are exposed during total subcapsular excision, the conventional monopolar or bipolar cautery can be used, with a significant increase in postoperative pain due to more extensive tissue injury, and a higher risk for postoperative hemorrhage.
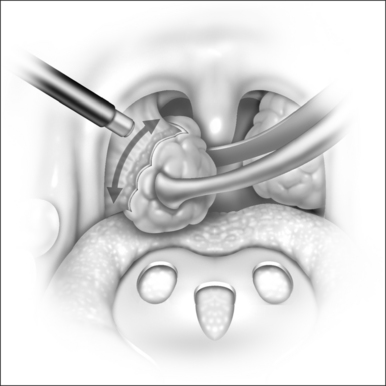
The dissection for total tonsillectomy is similar to the traditional technique. The capsule is identified by blunt dissection. The tonsil is retracted inferiorly and medially with an Allis clamp, and once the capsule is exposed, the wand is used to dissect it from the tonsillar fossa musculature in a superior-to-inferior and a lateral-to-medial direction (Fig. 67.2). Dissection is facilitated by retracting the tonsil inferomedially, due to the creation of a plane under tension. The power is set at a moderate coblation level (6 to 7) and the tip of the instrument is directed towards the capsule, leaving a small space over the tissue, which allows a plasma layer to form. As the dissection proceeds, the fibrous tissue will be preferentially excised. Small blood vessels are fused as they are encountered, by applying more pressure with the tip of the wand.
3.2 CAPSULE-SPARING SUBTOTALTONSILLECTOMY
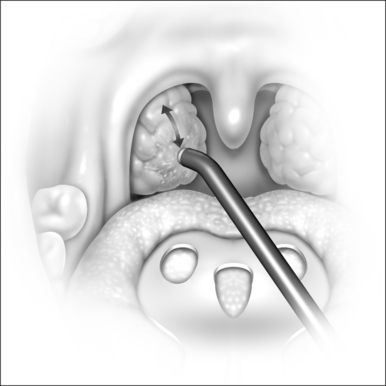
With the subtotal, capsule-sparing technique, about 90–95% of the tonsil can be removed. The tonsillar tissue is ablated from the surface inward with retraction of the pillar, which helps avoid the capsule and the surrounding extratonsillar structures. We use the coblation system by Arthrocare. The highest power settings are used while removing the tissue layer by layer, using brush-like motions (Fig. 67.3). The ensuing tonsillar reduction is immediate. Bleeding is usually controlled with coblation because it comes from small-caliber vessels. Meticulous care in preserving the anterior and posterior pillars is essential in order to achieve the best results. A thin layer of tissue is left in situ, which ensures that the surgeon will avoid penetrating the tonsillar capsule and exposing the underlying pharyngeal muscle. This allows for faster healing, reduced scarring, and a decreased incidence of postoperative bleeding.5 As the surgeon approaches the point where most of the tissue has been removed, the power setting is reduced and careful palpation is performed, in order to determine the need for carefully removing any additional tissue. Penetrating the capsule or injuring the pillars will result in increased bleeding, which might require the use of electrocautery. The electrodes at the tip of the wand should be periodically wiped off, and if the tip of the wand becomes clogged, it should be rinsed in saline solution by dipping it into a basin while activating the pedal to flush the suction port.
4 POSTOPERATIVE MANAGEMENT AND COMPLICATIONS
Radiofrequency-assisted total tonsillectomy can result in significant postoperative pain, swelling, and a delayed return to regular diet, much like traditional, electrocautery-assisted tonsillectomy. The liberal use of electrocautery during the procedure is probably responsible, at least in part, for such comparable morbidity,6 particularly when larger vessels are exposed and more tissue injury is caused by the efforts to achieve hemostasis. Timms and Temple7 demonstrated, however, that by minimizing the use of electrocautery during total, coblation-assisted tonsillectomy in pediatric and adult patients, the mean duration of postoperative pain was 2.4 and 5 days respectively, compared to 7.6 and 9 days for electrocautery-assisted tonsillectomy.
Pediatric patients undergoing capsule-sparing tonsillectomy experience an average intensity of pain of 2.5 (on a scale of 0 to 10) after coblation, with an average duration of 2.7 days postoperatively. Adults experience about 2.5 days at an average pain intensity of 2.8. By postoperative day 3, virtually all patients who undergo subtotal, capsule-sparing tonsil coblation are pain free, which represents a remarkable improvement when compared with classic, cold dissection tonsillectomy, which averages 9–10 days. Narcotics are rarely needed beyond day 1, and a return to normal activity level and regular diet occurs, on average, by postoperative day 2.5 Consistent with these figures, Arya did not find any difference between intra- and subcapsular tonsillectomies when analyzing postoperative pain scores by means of visual analog pain scales in a double-blind, randomized, controlled study.8
Similar morbidity can be described for radiofrequency tonsil ablation, where pediatric patients experience an average 1.5 pain intensity level, for a mean of 1.7 days, and adults complain of 1.6 days of pain, at a mean intensity of 1.5.5
Coblation-assisted total tonsillectomy has been associated with an increased risk of postoperative hemorrhage. In 2003, the National Prospective Tonsillectomy Audit of England and Northern Ireland was initiated in order to determine the magnitude of this increased risk.9,10 After reviewing 11,796 tonsillectomies, we found that 4.4% of the 684 patients who underwent coblation-assisted tonsillectomy had either primary hemorrhage (leading to prolonged hospital stay, blood transfusion, or return to the OR) or secondary hemorrhage (within 28 days, leading to readmission). We concluded that the main factor in this increased risk of hemorrhage, when compared to traditional, cold dissection tonsillectomy (where only 1.28% of 1327 patients had postoperative hemorrhage), was an inappropriate use of coblation and/or electrocautery, in order to stop intraoperative bleeding. Significant thermal damage to the surrounding tissue is likely responsible for delayed-type hemorrhage. A learning curve is therefore crucial in attaining the best results and in minimizing complications when using radiofrequency-assisted total tonsillectomy. Other authors, however, have described a decreased incidence of delayed hemorrhage in patients who underwent coblation tonsillectomy, when compared to blunt dissection or electrocautery diathermy tonsillectomies.11,12
5 SUCCESS RATE OF THE PROCEDURE
The efficacy of radiofrequency tonsil reduction can be compared to classic tonsillectomy in terms of its efficacy, under the assumption that classic tonsillectomy removes 100% of the tonsillar tissue. In a series of adult and pediatric patients published by Friedman et al.,5 it was found that tonsillar ablation achieved a volumetric reduction ranging between 30% and 70%, with a mean reduction of about 51% in pediatric patients, whereas tonsillar radiofrequency coblation achieved shrinkage ranging between 75% and 95%, with a mean of about 86%. Adult patients showed similar results, ranging from 40% to 70% and averaging about 54% for tonsillar ablation, and 75–95% with an average of 90% for tonsillar coblation. The coblation group was statistically more effective in terms of tonsil removal in both patient populations, with the additional advantage of yielding more consistent results.
When coblation is used to perform total tonsillectomy, as opposed to subtotal tonsillectomy, very similar results in terms of morbidity are achieved when compared to classic tonsillectomy. The wand is basically used as a dissection tool that removes the tonsil along the capsular plane, thereby exposing underlying muscle and nerves. The disruption of the capsule underlies the main source of morbidity, which is pain, and in this setting, coblation does not offer a distinct advantage over cold dissection tonsillectomy. As noted earlier, the key and common mistakes that can increase morbidity of the subcapsular technique are the inadvertent contact of the active wand with the oropharyngeal mucosa, overly aggressive tonsil coblation that exposes muscle and causes potential bleeding, and incomplete coblation of tissue that leaves more than 10% of the tonsil intact. Subtotal tonsillectomy should not be performed on patients undergoing classic uvulopalatopharyngoplasty, since tonsillar tissue would be buried under the pillars after closure.
6 CONCLUSION
Tonsillectomy, either alone or, most frequently, in combination with other procedures, remains one of the most common surgical procedures performed for the management of OSAHS, in both the pediatric and adult population. Subcapsular radiofrequency coblation shows distinct advantages over classic tonsillectomy, including early elimination of pain, early return to normal diet and activity, and precise removal of tonsillar tissue. This technique is ideal for hypertrophic tonsils in the context of airway obstruction in sleep apnea.
Table 67.1 Causes of sleep-related breathing disorders in children
| Neonates and infants |
| Nasal aplasia, stenosis, or atresia |
| Nasal or nasopharyngeal masses |
| Craniofacial anomalies |
| Hypoplastic mandible (Pierre Robin, Nager’s, Treacher Collins) |
| Hypoplastic maxilla (Apert’s, Crouzon’s) |
| Macroglossia (Beckwith-Wiedemann) |
| Vascular malformations of tongue and pharynx |
| Congenital cysts of the vallecula and tongue |
| Neuromuscular disorders |
| Toddlers and older children |
| Rhinitis, nasal polyposis, septal deviation |
| Syndromic narrowing of nasopharynx (Hunter’s, Hurler’s, Down’s, achondroplasia) |
| Adenotonsillar hyperplasia |
| Obesity |
| Macroglossia (Down’s) |
| Vascular malformations of tongue and pharynx |
| Neuromuscular disorders |
| Iatrogenic |
| Nasopharyngeal stenosis |
1. Sher AE, Schechtman KB, Piccirillo JF. The efficacy of surgical modifications of the upper airway in adults with obstructive sleep apnea syndrome. Sleep. 1996;19:156-177.
2. Hultcrantz E, Linder A, Markstrom A. Tonsillectomy or tonsillotomy? A randomized study comparing postoperative pain and long-term effects. Int J Pediatr Otorhinolaryngol. 1999;51:171-176.
3. Morris L, Lee K. Coblation techniques for sleep disordered breathing. In: Terris D, Goode R, eds. Surgical Management of Sleep Apnea and Snoring. Location?: Informa Healthcare; 2005.
4. Darrow D, Siemens C. Indications for tonsillectomy and adenoidectomy. Laryngoscope. 2002;112:6-10.
5. Friedman M, LoSavio P, Ibrahim H, et al. Radiofrequency tonsil reduction: safety, morbidity, and efficacy. Laryngoscope. 2003;113:882-887.
6. Bäck L, Paloheimo M, Ylikoski J. Traditional tonsillectomy compared with bipolar radiofrequency thermal ablation tonsillectomy in adults: a pilot study. Arch Otolaryngol Head Neck Surg. 2001;127:1106-1112.
7. Timms M, Temple R. Coblation tonsillectomy: a double blind randomized controlled study. J Laryngol Otol. 2002;116:450-452.
8. Arya A, Donne A, Nigam A. Double-blind randomized controlled study of coblation tonsillotomy versus coblation tonsillectomy on postoperative pain in children. Clin Otolaryngol. 2005;30:226-229.
9. Lowe D, van der Meulen J, Cromwell D, et al. Key messages from the National Prospective Tonsillectomy Audit. Laryngoscope. 2007;117:717-724.
10. Hopkins C, Ajulo P, Krywawych M, et al. The impact of the interim report of the National Prospective Tonsillectomy Audit. Clin Otolaryngol. 2005;30:475-476.
11. Belloso A, Chidambaram A, Morar P, et al. Coblation tonsillectomy versus dissection tonsillectomy: postoperative hemorrhage. Laryngoscope. 2003;113:2010-2013.
12. Divi V, Benninger M. Postoperative tonsillectomy bleed: coblation versus noncoblation. Laryngoscope. 2005;115:31-33.