Chapter 40 Radiofrequency tongue base reduction in sleep-disordered breathing
1 INTRODUCTION
1.1 PREOPERATIVE EVALUATION
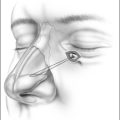
Sleep-disordered breathing is caused by collapse or obstruction of the upper airway during sleep. This obstruction may occur at any site along the upper airway passages to include the nasal cavity, oropharynx, hypopharynx and larynx. Once the presence of sleep-disordered breathing is documented by a nocturnal polysomnogram and the patient is intolerant of medical therapy, the presurgical evaluation preceeds. The preoperative evaluation includes a comprehensive head and neck physical examination, fiberoptic nasopharyngoscopy and an optional lateral cephalometric radiograph to determine the site or sites of upper airway obstruction. Other diagnostic avenues, such as sleep endoscopy, may also be performed by the surgeon in directing surgical therapy in a site-specific approach. If the base of tongue is determined to be a causative factor in the upper airway collapse, then adding radiofrequency tongue base reduction to the therapeutic regime is contemplated. Numerous surgical procedures have been developed to address each of the sites of obstruction and have offered the surgeon an armamentarium of options, each with its own set of advantages, disadvantages and success rates.
3 OUTLINE OF PROCEDURE: TONGUE BASE RADIOFREQUENCY
The technique can be performed as an outpatient or as an inpatient. Depending on the severity of the patient’s sleep-disordered breathing, post-treatment airway monitoring and/or protection with nasal continuous positive airway pressure (CPAP) or a tracheotomy may be considered.
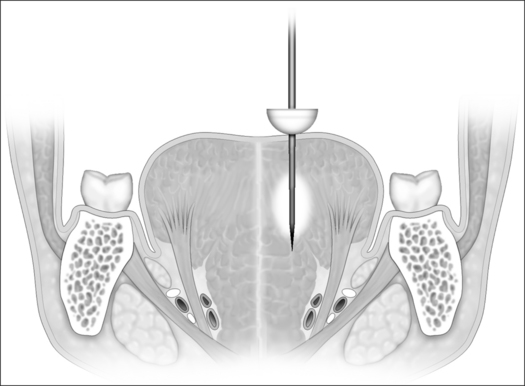
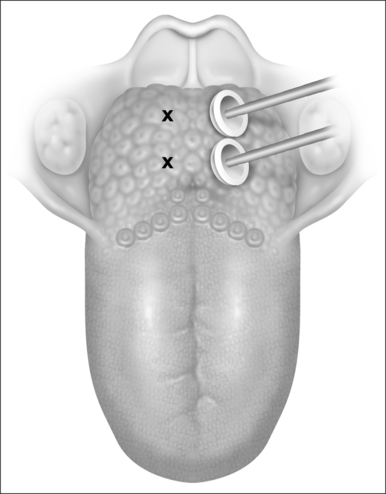
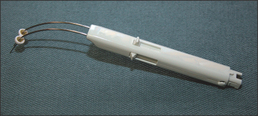
Currently, a dual 22-gauge RF needle electrode with a10 mm active length and a 10 mm protective sheath in a custom-fabricated device allows placement of the electrode under the superficial tongue musculature in the area selected for treatment. Potential sites of treatment include the midline and paramedian dorsal base of tongue areas and the anterior ventral tongue areas (Figs 40.1 and 40.2). Treatment sites should be spaced a minimum of 1.5 cm apart if a single needle probe is used or at least 2.5 cm using the dual needle probe device (Fig. 40.3). Continual pressure on the electrode and visualization that the insulation sheath is not retracting out of the tongue tissue reduce the risk of superficial tissue injury. Using the most current Gyrus radio frequency generator machines and a dual probe at 85°C, 600 joules (J) of rapid energy radiofrequency is delivered to two base of tongue sites with a total of 1200 J delivered. Treatment sessions may be repeated every 4–6 weeks.
4 POSTOPERATIVE MANAGEMENT AND COMPLICATIONS
To diminish the risk of infection in patients undergoing tongue base radiofrequency, a number of precautions and directions can be followed (Table 40.1). The incidence of tongue abscess formation in nearly every study ranges from 0 to 1.5%. Following the recommendations inTable 40.1 may limit the incidence of tongue superficial ulcerations and infection.
Table 40.1 Technical factors to decrease the risk of infection
| 1. Give prophylactic oral antibiotics. |
| 2.Recommend 0.12% oral chlorhexidine (Peridex) gargle prior to treatment. |
| 3.Use sterile technique. |
| 4.Use a new sterile needle for each local anesthetic injection site. |
| 5.Avoid corticosteroids. |
| 6.Ensure the electrode is seated into the tongue to prevent a superficial ulceration. |
| 7.Do not deliver more than 600 J of rapid energy per treatment site with the dual probe. |
| 8.Consider other treatment alternatives in diabetic mellitus patients. |
To avoid hypoglossal nerve injury, it is best to limit the ablation sites to no more than 2 cm lateral to midline. The neurovascular bundle is approximately 2–3 cm from the surface epithelium and approximately 2–3 cm lateral from midline in a normal sized tongue (Figs 40.1 and 40.2).
5 TONGUE BASE RADIOFREQUENCY RESULTS
In the first published study evaluating RF for sleep-disordered breathing, a porcine study1 evaluated the relationship of lesion size to total RF energy delivery and subsequent tissue volume reduction. The study showed that tongue musculature volume could be safely reduced using RF energy in a precise and controlled manner with minimal risk of mucosal injury or infection. As the total energy delivered increased from 500 to 2400 J the lesion cross-sectional area increased from 0.7 cm2 to 1.4 cm2. After 3 weeks of scar formation and subsequent contraction the overall tissue volume reduced by 26.3%.
The first human tongue pilot study2 investigated the feasibility, safety, and possible efficacy in the treatment of sleep-disordered breathing. Eighteen patients were enrolled in the study. These patients were incompletely treated with upper airway reconstruction procedures, all of which underwent at least an uvulopalatopharyngoplasty. The mean preoperative Apnea/Hypopnea Index (AHI) of 39.6 improved to a mean of 17.8 (55%) post treatment; the mean Apnea Index (AI) of 22.1 improved to a mean of 4.1 (80%); and the mean preoperative SAO2 nadir of 81.9% improved to 88.3% (12%) post treatment. The mean energy delivery per treatment session was 1543 J for a mean total energy delivery of 8490 J. Magnetic resonance imaging revealed a tongue volume reduction of 17% with an improvement of the posterior airway space by 15%. Speech and swallowing evaluated by VAS scores were unchanged. The only complication was one tongue abscess in 181 treatment sessions, which resolved after incision and drainage.
A long-term follow-up study3 on the patients in the initial human study revealed 16 patients completed the follow-up at a mean of 28 months after the initial treatment. Sleep studies were performed using a new nasal cannula by Sleep Solutions (Redwood City, CA), which can quantitate airflow. This technology is thought to be more accurate in identifying hypopneas. The follow-up data revealed that the AI remained the same at 5.4, but the overall AHI relapsed to 28.7. The SAO2 nadir relapsed to 85.8%. There were no changes in the quality of life scale (SF36), Epworth Sleepiness Scale, speech or swallowing VAS scores. The conclusion of the authors was that the success of tongue base RF may reduce with time with the primary relapse in the AHI. The limitation of the study was the use of different monitoring devices to document hypopneas.
A prospective, non-randomized study4 evaluated 10 patients who underwent uvulopalatopharyngoplasty (UPPP), nasal surgery and tongue base RF as an inpatient. Two additional RF sessions were performed postoperatively in an outpatient setting. Nine of the ten patients received a cumulative dose of approximately 12,000 J.Five of these patients were successfully treated, defined as an AHI <20 with at least a 50% reduction in AHI. The mean preoperative AHI of 29.5 ±14.8 improved to a mean AHI 18.8 ± 14.6 and the mean AI of 8.7 ± 6.4 improved to a mean AI of 3.7 ± 4.9.
Another study5 compared the results of treatment with UPPP alone compared to tongue RF along with UPPP showing that the combined approach significantly improved the success rate in patients with level II and III sites of upper airway obstruction. The success rate increased in level II patients by 17.2% (37.9% vs. 55.1%) and in level III patients by 24.9% (8.1% vs. 33.0%) with the addition of tongue base RF to the UPPP procedure.
A multi-institutional study6 evaluated 73 patients with underlying obstructive sleep apnea; 56 (76.7%) of these patients completed tongue base RF and follow-up polysomnography. Sixty-five (92.9%) had prior pharyngeal surgery. A mean of 5.4± 1.8 treatment sessions were performed with a mean of 3.1 ± 0.9 lesions per treatment session and an overall energy delivery of 13,394± 5459 J.The mean AHI of 40.5 ± 21.5 decreased to a mean of 32.8±22.6 post treatment. The authors concluded that RF diminishes the severity of obstructive sleep apnea with subjective outcomes comparable to nasal CPAP.
In an investigation to utilize higher energy levels, 20 patients under local anesthesia were treated with two treatment sessions delivering 2800 J per session (700 J to each of four tongue base sites) for a total of 5600 J.7 The results revealed a reduction of the mean AHI of 27.7 to 22.6 and showed a 45% success rate, defined as an AHI less than 20 with at least a 50% improvement. A subsequent study by the same authors using 2800 J per treatment session and a mean number of 3.4 treatment sessions revealed a mean reduction of the AHI from 32.1 to 24.9 and a 33% success rate.8
Steward9 evaluated 22 patients who underwent both palatal and tongue RF treatments (mean 4.8 tongue and 1.8 palate sessions) and revealed statistical improvement in daytime sleepiness, and a significant improvement in the AHI from 31.0 to 18.7. The surgical success was 59% defined as an AHI less than 20 with at least a 50% improvement. There were no significant postoperative complications.
Twenty-six patients with mild to moderate sleep apnea were randomized to RF therapy for three tongue treatments and then two additional tongue and palate treatments.10 The initial three tongue treatments significantly improved the quality of life and the additional two tongue and palate RF treatments further significantly improved the quality of life as determined by the Functional Outcomes of Sleep Questionnaire (FOSQ), daytime sleepiness and reaction times.
A study evaluating the efficacy of ventral tongue probe placement combined with dorsal RF delivery in 20 patients revealed no significant complications and a mean AHI decreased from 35.1 ± 18.1 to 15.1 ± 17.4.11 The authors noted the limitations of the study with lack of a control group, small sample size and short-term follow-up, but had significant results of the combined treatment of the ventral and dorsal surfaces of the tongue.
A randomized trial compared tongue and palatal RF and nasal CPAP to sham-placebo. Both nasal CPAP and multi-level RF revealed improvement in quality of life parameters as compared to placebo and there were no differences between the RF and nasal CPAP groups.12
Tongue base radiofrequency has been shown to improve the amount of obstructions in patients with sleep-disordered breathing. The technique can be performed as an outpatient or inpatient, under local or general anesthesia with minimal risks of complications and minimal quality of life changes. Tongue radiofrequency volumetric tissue reduction yields improvement in the AHI of obstructive sleep apnea patients in all studies to date and is usually a low-risk procedure; however, following the preceding recommendations will aid in minimizing possible complications.13 If there is persistent obstructive sleep apnea confirmed by a postoperative sleep study, other stand-alone surgical procedures or in combination with tongue RF may be considered.
1. Powell NB, Riley RW, Troell RJ, et al. Radiofrequency volumetric reduction of the tongue: a porcine pilot study for the treatment of obstructive sleep apnea syndrome. Chest. 1997;111:1348-1355.
2. Powell NB, Riley RW. Guilleminault C. Radiofrequency tongue base reduction in sleep-disordered breathing: a pilot study. Otolaryngol Head Neck Surg. 1999;120:656-664.
3. Li KK, Powell NB, Riley RW, et al. Temperature-controlled radiofrequency tongue base reduction for sleep-disordered breathing: long-term outcomes. Otolaryngol Head Neck Surg. 2002;127(3):230-234.
4. Nelson LM. Combined temperature-controlled radiofrequency tongue reduction and UPPP in apnea surgery. ENT J. 2001;80(9):640-644.
5. Friedman M. Combined UPPP and radiofrequency tongue base reduction for treatment of OSAHS. Otolaryngol Head Neck Surg. 2003;129(6):611-621.
6. Woodson BT, Nelson L, Mickelson S, et al. A multi-institutional study of radiofrequency volumetric tissue reduction for OSAS. Otolaryngol Head Neck Surg. 2001;125(4):303-311.
7. Stuck BA, Maurer JT, Horman. Tongue base reduction with radiofrequency tissue ablation: preliminary results after two treatment sessions. Sleep Breath. 2000;4(4):155-162.
8. Stuck BA, Maurer JT, Verse T, et al. Tongue base reduction with temperature-controlled radiofrequency volumetric tissue reduction for treatment of obstructive sleep apnea syndrome. Acta Otolaryngol. 2002;122:531-536.
9. Steward DL. Effectiveness of multilevel (tongue and palate) radiofrequency tissue ablation for patients with obstructive sleep apnea syndrome. Laryngoscope. 2004;114:2073-2084.
10. Steward DL, Weaver EM, Woodson BT. A comparison of radiofrequency treatment schemes for obstructive sleep apnea syndrome. Otolaryngol Head Neck Surg. 2004;130(5):579-585.
11. Riley RW, Powell NB, Li KK, et al. An adjuvant method of radiofrequency volumetric tissue reduction of the tongue for OSAS. Otolaryngol Head Neck Surg. 2003;129(1):37-42.
12. Woodson BT, Steward DL, Weaver EM, et al. A randomized trial of temperature-controlled radiofrequency, continuous positive airway pressure, and placebo for obstructive sleep apnea syndrome. Otolaryngol Head Neck Surg. 2003;128(6):848-861.
13. Pazos G, Mair EA. Complications of radiofrequency ablation in the treatment of sleep-disordered breathing. Otolaryngol Head Neck Surg. 2001;125(5):462-467.