CHAPTER 10 Radiation Dose Reduction Strategies in Cardiac Computed Tomography
A strategy for reducing radiation dose to the patient undergoing cardiac imaging should be employed particularly for patients at greatest risk for harm from x-ray exposure to the chest, young patients, and female patients.1 This plan should include educating patients on the risks of exposure to ionizing radiation, seeking alternative studies that do not rely on ionizing radiation (e.g., MRI or ultrasonography) when appropriate, assessing the risk/benefit ratio of CT for the individual patient, and applying the as low as reasonably achievable (ALARA) principle to the selection of CT scan parameters.
TECHNIQUE TO REDUCE X-RAY TUBE CURRENT
Technique Description
ECG-Based Reduction in Tube Current
During cardiac imaging, the x-ray tube current can be switched off or greatly reduced during systolic phases of the cardiac cycle significantly decreasing radiation dose. In patients with low, stable heart rates, data acquisition can be confined to a limited portion of the RR interval using prospectively ECG-triggered axial techniques. Average effective radiation doses of 2 to 3 mSv have been reported using these techniques to image the coronary arteries.2,3
Axial imaging is associated with increased sensitivity to arrhythmia, owing to prospective referencing of the ECG signal, and increased examination times, owing to incrementing the patient table between acquisitions. It is often necessary to acquire data during the entire cardiac cycle using a helical mode and retrospectively reference image reconstruction to a simultaneously recorded ECG signal. Although ECG-gated helical techniques require continuous x-ray exposure, tube current outside the phase of interest can be reduced to decrease patient radiation dose significantly. Effective radiation doses can easily exceed 15 mSv4 using helical imaging without ECG-based dose modulation, but can be reduced 50% or more depending on patient heart rate,5 the minimum tube current value,6 and the duration of the full tube current window.7
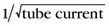
Size-Based Reduction in Tube Current
The x-ray tube current can be reduced for slimmer patients. Attenuation of the incident x-ray beam decreases with the thickness of the tissue between the x-ray source and the detector such that less radiation exposure is required to penetrate thinner tissues and achieve desired image noise (Fig. 10-1). Patients can be assigned to size categories based on visual inspection, weight, body mass index, or cross-sectional body measurements from scout images,8 and the tube current can be adjusted manually to a predefined value. Weight-adapted tube current protocols were shown to reduce coronary CT angiography dose by 18% in men and 26% in women9 at one institution.
Automatic methods of online adaptation of tube current to patient size can also be used to reduce dose. The tube current can be modulated along the x, y, and z directions during scanning based on local tissue thickness without sacrificing image noise. Tube current is reduced at projection angles and table positions requiring less x-ray penetration. Online, anatomic-based tube current modulation has been shown to reduce radiation exposure to the thorax by 20% compared with a fixed tube current while maintaining image noise.10
Pitfalls and Solutions
ECG-Based Reduction in Tube Current
Helical data acquisition with retrospective ECG gating is less susceptible to cardiac motion artifacts and provides an alternative to axial imaging at high or irregular heart rates. ECG-based tube current modulation is prescribed before scanning, however, so changes in heart rate could result in unintended reduction of the tube current during a desired phase of reconstruction for a given cardiac cycle. Some CT systems allow adjustment of the full tube current duration, increasing the utility of ECG-based tube current modulation for patients with high or irregular heart rates because the optimal reconstruction phase is less predictable.7 For patients with severe arrhythmia, some systems temporarily suspend or permanently switch off ECG-based tube current modulation if beat-to-beat variation exceeds a threshold value during data acquisition, virtually eliminating the risk of improperly timed downward modulation of the tube current.
TECHNIQUE TO REDUCE TUBE VOLTAGE
Indications
Selection of a reduced x-ray tube voltage is indicated in thin patients to reduce radiation dose.
Technique Description
As with x-ray tube current, x-ray tube voltage can be reduced according to patient size to avoid unnecessary exposure to slimmer patients, while still achieving acceptable image noise. Size can be assessed as described previously, and tube voltage can be adjusted accordingly. A more recent study showed a tube voltage of 100 kVp could be used to obtain diagnostic quality coronary CT angiography images from patients of normal weight with a 25% decrease in average effective dose compared with a tube voltage of 120 kVp; the average effective dose was decreased by 50% and diagnostic image quality was maintained when tube current was also reduced.11
Pitfalls and Solutions
Hounsfield unit (HU)–dependent analysis of cardiac CT images is affected by changes in tube voltage because of associated changes in tissue attenuation characteristics. Automatic bolus timing methods rely on the attenuation of enhanced blood within a specified region of interest to reach a predefined threshold before initiating the scan. Because iodine absorption increases with a decrease in tube voltage, iodinated contrast material appears brighter on 100 kVp images compared with 120 kVp images. This may necessitate a higher threshold with automatic bolus timing to prevent premature initiation of the scan if the contrast injection protocol is unchanged. Alternatively, it may be possible to reduce iodinated contrast media volume at 100 kVp compared with 120 kVp, but maintain blood pool opacification.12 Additionally, attenuation-based characterization of tissues typically relies on HU thresholds or ranges established with 120 kVp imaging that may not be appropriate at 100 kVp. Affected cardiac applications include, but are not limited to, quantification of coronary artery calcium, characterization of coronary artery plaque, and differentiation of simple fluid and blood products or soft tissue.
TECHNIQUE TO INCREASE BEAM PITCH (FOR HELICAL SCANNING)
TECHNIQUE TO INCREASE RECONSTRUCTED SLICE THICKNESS
Technique Development
The reconstructed slice thickness determines the number of absorbed x-ray photons contributing to the CT image. An increase in the reconstructed slice thickness increases the number of x-ray photons contributing to each image allowing a decrease in the number of absorbed x-ray photons (i.e., decrease in radiation dose) to achieve the same image noise (Fig. 10-2). Noise is proportional to 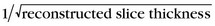 such that a 3 mm thick image has 73% less noise than a 1 mm thick image. The decrease in tube current and radiation dose made possible by an increase in reconstructed slice thickness comes at a cost of decreased spatial resolution. The reconstruction of thicker slices is inappropriate for evaluation of small cardiac anatomy such as the coronary arteries.
such that a 3 mm thick image has 73% less noise than a 1 mm thick image. The decrease in tube current and radiation dose made possible by an increase in reconstructed slice thickness comes at a cost of decreased spatial resolution. The reconstruction of thicker slices is inappropriate for evaluation of small cardiac anatomy such as the coronary arteries.
Pitfalls and Solutions
KEY POINTS
 ECG-based tube current modulation can be used most aggressively in patients with low, stable heart rates.
ECG-based tube current modulation can be used most aggressively in patients with low, stable heart rates. The nominal tube current can be reduced for smaller patients before imaging, but anatomic-based, online modulation has limited utility for cardiac imaging.
The nominal tube current can be reduced for smaller patients before imaging, but anatomic-based, online modulation has limited utility for cardiac imaging. Decreasing the tube voltage can reduce radiation dose and is appropriate in smaller patients, but affects the attenuation properties of tissues.
Decreasing the tube voltage can reduce radiation dose and is appropriate in smaller patients, but affects the attenuation properties of tissues.Kalara MK, Maher MM, Toth TL, et al. Strategies for CT radiation dose optimization. Radiology. 2004;230:619-628.
Kubo T, Lin PP, Stiller W, et al. Radiation dose reduction in chest CT: a review. AJR Am J Roentgenol. 2008;190:335-343.
McNitt-Gray MF. AAPM/RSNA physics tutorial for residents: topics in CT. Radiation dose in CT. RadioGraphics. 2002;22:1541-1553.
Paul JF, Abada HT. Strategies for reduction of radiation dose in cardiac multislice CT. Eur Radiol. 2007;17:2028-2037.
Primack AN, McCollough CH, Bruesewitz MR, et al. Relationship between noise, dose, and pitch in cardiac multi-detector row CT. RadioGraphics. 2006;26:1785-1794.
1 Einstein AJ, Henzlova MJ, Rajagopalan S. Estimating risk of cancer associated with radiation exposure from 64-slice computed tomography coronary angiography. JAMA. 2007;298:317-323.
2 Earls JP, Berman EL, Urban BA, et al. Prospectively gated transverse coronary CT angiography versus retrospectively gated helical technique: improved image quality and reduced radiation dose. Radiology. 2008;246:742-753.
3 Husmann L, Valenta I, Gaemperli O, et al. Feasibility of low-dose coronary CT angiography: first experience with prospective ECG-gating. Eur Heart J. 2008;29:191-197.
4 Hausleiter J, Meyer T, Hermann F, et al. Estimated radiation dose associated with cardiac CT angiography. JAMA. 2009;301:500-507.
5 Jakobs T, Becker CR, Ohnesorge B, et al. Multislice helical CT of the heart with retrospective ECG gating: reduction of radiation exposure by ECG-controlled tube current modulation. Eur Radiol. 2002;12:1081-1086.
6 Stolzmann P, Scheffel H, Schertler T, et al. Radiation dose estimates in dual-source computed tomography coronary angiography. Eur Radiol. 2008;18:592-599.
7 Leschka S, Scheffel H, Desbiolles L, et al. Image quality and reconstruction intervals of dual-source CT coronary angiography: recommendations for ECG-pulsing windowing. Invest Radiol. 2007;42:543-549.
8 McCollough CH, Ulzheimer S, Halliburton SS, et al. A multi-institutional, multi-manufacturer, international standard for the quantification of coronary artery calcium using cardiac CT. Radiology. 2007;243:527-538.
9 Jung B, Mahnken AH, Stargardt A, et al. Individually weight-adapted examination protocol in retrospectively ECG-gated MSCT of the heart. Eur Radiol. 2003;13:2560-2566.
10 Mulkens TH, Bellinck P, Baeyaert M, et al. Use of an automatic exposure control mechanism for dose optimization in multi-detector row CT examinations: clinical evaluation. Radiology. 2005;237:213-223.
11 Leschka S, Stolzmann P, Schmid FT, et al. Low kilovoltage cardiac dual-source CT: attenuation, noise, and radiation dose. Eur Radiol. 2008;18:1809-1817.
12 Sigal-Cinqualbre AB, Hennequin R, Abada HT, et al. Low-kilovoltage multi-detector row chest CT in adults: feasibility and effect on image quality and iodine dose. Radiology. 2004;231:169-174.

 such that a 20% reduction in tube current results in a 12% increase in image noise.
such that a 20% reduction in tube current results in a 12% increase in image noise.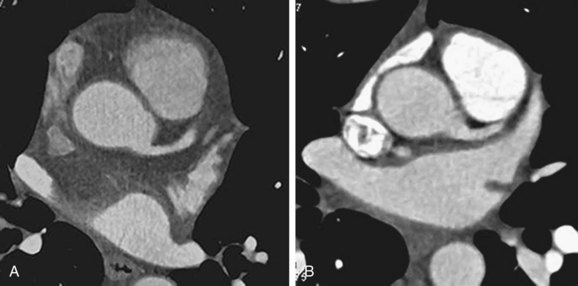
 FIGURE 10-1
FIGURE 10-1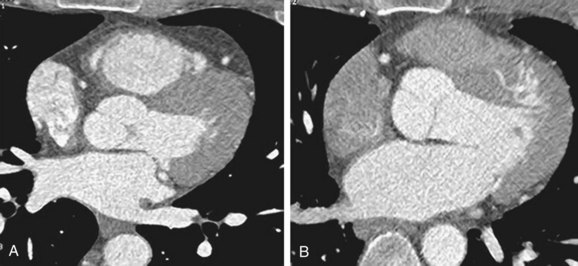
 FIGURE 10-2
FIGURE 10-2



