Radiation dose, dosimetry and dose limitation
Dose units
Radiation-absorbed dose (D)
| SI unit: | joules/kg (J/kg) |
| Special name: | Gray (Gy) |
| Subunit names: | milligray (mGy) (× 10−3) |
| microgray (µGy) (× 10−6) |
Equivalent dose (HT)
For example, alpha particles (see Ch. 18) penetrate only a few millimeters in tissue, lose all their energy and are totally absorbed, whereas X-rays penetrate much further, lose some of their energy and are only partially absorbed. The biological effect of a particular radiation-absorbed dose of alpha particles would be considerably more severe than a similar radiation-absorbed dose of X-rays.
| X-rays, gamma rays and beta particles | WR = 1 |
| Fast neutrons (10 keV – 100 keV) and protons | WR = 10 |
| Alpha particles | WR = 20 |
The equivalent dose (HT) in a particular tissue is therefore calculated as follows:Equivalent dose (HT) = radiation-absorbed dose (D) × radiation weighting factor (WR) in a particular tissue
| SI unit: | joules/kg (J/kg) |
| Special name: | Sievert (Sv) |
| Subunit names: | millisievert (mSv) (× 10−3) |
| microsievert (µSv) (× 10−6) |
For X-rays, the radiation weighting factor WR = 1, therefore the equivalent dose (HT) in a particular tissue, measured in Sieverts, is equal to the radiation-absorbed dose (D), measured in Grays.
Effective dose (E)
The tissue weighting factors recommended by the ICRP in 1990 and revised in 2007 are shown in Table 6.1.
Table 6.1
The tissue weighting factors (WT) recommended by the ICRP in 1990 and revised in 2007
| Tissue | 1990 WT | 2007 WT |
| Bone marrow | 0.12 | 0.12 |
| Breast | 0.05 | 0.12 |
| Colon | 0.12 | 0.12 |
| Lung | 0.12 | 0.12 |
| Stomach | 0.12 | 0.12 |
| Gonads | 0.20 | 0.08 |
| Bladder | 0.05 | 0.04 |
| Oesophagus | 0.05 | 0.05 |
| Liver | 0.05 | 0.04 |
| Thyroid | 0.05 | 0.04 |
| Bone surface | 0.01 | 0.01 |
| Brain | * | 0.01 |
| Kidneys | * | 0.01 |
| Salivary glands | – | 0.01 |
| Skin | 0.01 | 0.01 |
| Remainder tissues | 0.05* | 0.12† |
*Adrenals, brain, upper large intestine, small intestine, kidney, muscle, pancreas, spleen, thymus and uterus.
†Adrenals, extrathoracic airways, gallbladder, heart wall, kidney, lymphatic nodes, muscle, pancreas, oral mucosa, prostate, small intestine wall, spleen, thymus and uterus/cervix.
Effective dose (E) = ∑ Equivalent dose (HT) in each tissue × relevant tissue weighting factor (WT)
| Special name: | sievert (Sv) |
| Subunit names: | millisievert (mSv) (× 10−3) |
| microsievert (µSv) (× 10−6) |
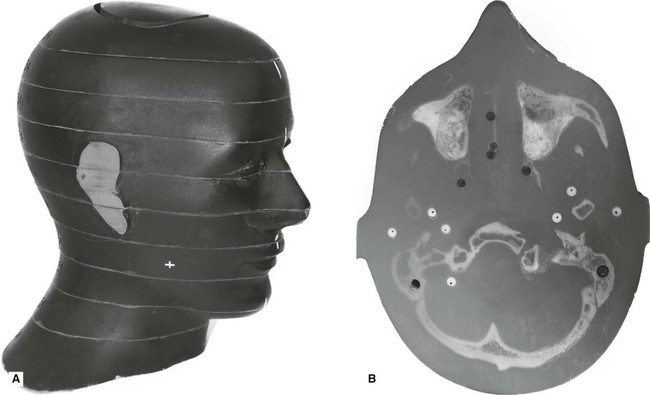
One way of calculating the effective dose is by using a tissue equivalent anthropomorphic phantom with dosimeters placed in the most radiosensitive regions, as shown in Fig. 6.1.
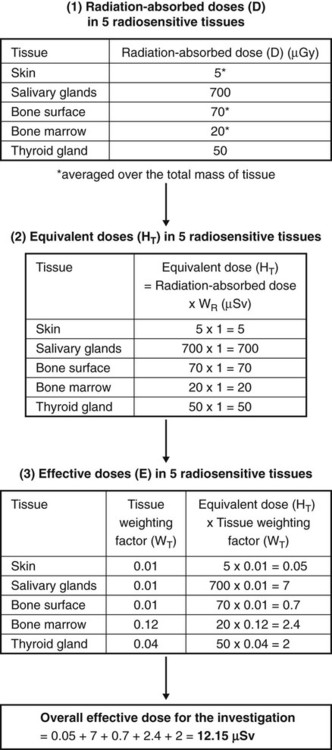
As individual doses are very small from any one examination, a number of radiographic exposures are repeatedly performed (e.g. ten times) using typical exposure factors (time, kV and mA), for that particular examination. The dosimeters are then ‘read’ to give a measurement of the radiation-absorbed dose (D) in the individual tissues. Using this data both the equivalent dose (HT) and the effective dose (E) may be calculated, as shown in the simplified flow diagram shown in Fig. 6.2.
When the simple term dose is applied loosely, it is the effective dose (E) that is usually being described. Effective dose can thus be thought of as a broad indication of the risk to health from any exposure to ionizing radiation, irrespective of the type or energy of the radiation or the part of the body being irradiated. A comparison of effective doses from different investigations is shown in Table 6.2.
Table 6.2
Typical effective doses for a range of dental and routine medical examinations
| X-ray examination | Effective dose (E) (mSv) |
| Bitewing/periapical radiograph | 0.0003–0.022 |
| Panoramic radiograph | 0.0027–0.038 |
| Upper standard occlusal | 0.008 |
| Lateral cephalometric radiograph | 0.0022–0.0056 |
| Skull radiograph (posteroanterior, PA) | 0.02 |
| Skull radiograph (lateral) | 0.016 |
| Chest (posteroanterior, PA) | 0.014 |
| Chest (lateral) | 0.038 |
| CT head | 1.4 |
| CT chest | 6.6 |
| CT abdomen | 5.6 |
| CT mandible and maxilla | 0.25–1.4 |
| Barium swallow | 1.5 |
| Barium enema | 2.2 |
| Dento-alveolar cone beam CT (CBCT) | 0.01–0.67 |
| Craniofacial cone beam CT (CBCT) | 0.03–1.1 |
Based broadly on the 2011 HPA publication Frequency and Collective Dose for Medical and Dental X-ray Examinations in the UK, the 2011 SEDENTEXCT publication Radiation Protection: Cone Beam CT for Dental and Maxillofacial Radiology and the 2013 Selection Criteria for Dental Radiography.
Dose limits
The dose limits for each group are based on the principle that the risk to any worker who receives the full dose limit will be such that the worker will be at no greater risk than a worker in another hazardous, but non-radioactive, environment. By way of example, Table 6.3 shows the previous and current annual dose limits in force in the UK.
Table 6.3
The previous annual dose limits and those currently in force in the UK
| Old dose limits | Current dose limits | |
| Classified workers | 50 mSv | 20 mSv |
| Non-classified workers | 15 mSv | 6 mSv |
| General public | 5 mSv | 1 mSv |
Dose rate
This is a measure of the dose per unit time, e.g. dose/hour, and is sometimes a more convenient, and measurable, figure than the total annual dose limits shown in Table 6.3.
| SI unit: | microsievert/hour (µSv h–1) |
Estimated annual doses
• Natural background radiation
– Cosmic radiation from the earth’s atmosphere
– Gamma radiation from the rocks and soil in the earth’s crust
– Ingestion of radioisotopes, e.g. 40K, in certain foods
– Inhalation of radon gas and its decay products, 222Rn is a gaseous decay product of uranium that is present naturally in granite. As a gas, radon diffuses readily from rocks through soil and can be trapped in poorly ventilated houses and then breathed into the lungs.
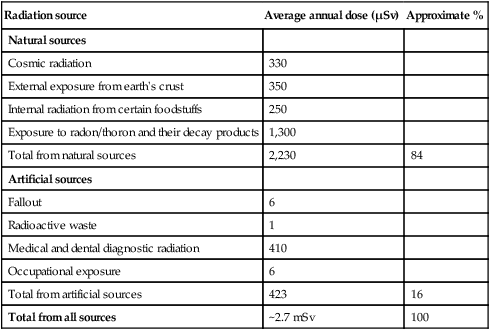
• Artificial background radiation
The Radiation Protection Division of the Health Protection Agency has estimated the annual doses from these various sources in the UK as illustrated in Table 6.4. As shown, an individual’s average dose from natural background radiation is estimated at about 2.23 mSv per year (84%) with and additional 0.423 mSv (16%) from artificial sources (total average dose approximately 2.7 mSv) including dental radiography. In the USA natural background radiation is estimated at approximately 3.2 mSv per year with an additional 3.0 mSv from artificial sources (total average dose 6.2 mSv). These figures are useful to remember when considering the magnitude of the doses associated with various diagnostic procedures, as shown previously in Table 6.2.
Table 6.4
| Radiation source | Average annual dose (µSv) | Approximate % |
| Natural sources | ||
| Cosmic radiation | 330 | |
| External exposure from earth’s crust | 350 | |
| Internal radiation from certain foodstuffs | 250 | |
| Exposure to radon/thoron and their decay products | 1,300 | |
| Total from natural sources | 2,230 | 84 |
| Artificial sources | ||
| Fallout | 6 | |
| Radioactive waste | 1 | |
| Medical and dental diagnostic radiation | 410 | |
| Occupational exposure | 6 | |
| Total from artificial sources | 423 | 16 |
| Total from all sources | ~2.7 mSv | 100 |
Dose limitation
• No practice shall be adopted unless its introduction produces a positive net benefit (Justification)
• All exposures shall be kept as low as reasonably practicable (ALARP), taking economic and social factors into account (Optimization)
• The dose equivalent to individuals shall not exceed the limits recommended by the ICRP (Limitation).
For the purposes of dose limitation, the ICRP has divided the population into three groups:
Patients
Radiographic investigations involving patients are divided into four subgroups:
• Examinations directly associated with illness
• Systematic examinations (periodic health checks)
• Examinations for occupational, medico-legal or insurance purposes
Examinations directly associated with illness
• There are no set dose limits
• The decision to carry out such an investigation should be based on:
– A correct assessment of the indications
– The way in which the results are likely to influence the diagnosis and subsequent treatment
– The clinician having an adequate knowledge of the physical properties and biological effects of ionizing radiation (i.e., adequately trained).
• The number, type and frequency of the radiographs requested or taken (selection criteria) are the responsibility of the clinician. Evidence-based selection criteria recommendations have been published in different countries in recent years to provide guidance in this clinical area of radiation protection. In the UK, the booklet Selection Criteria for Dental Radiography is published and regularly updated by the Faculty of General Dental Practice of the Royal College of Surgeons of England (3rd Edition published in 2013). National selection criteria documentation should be regarded as essential reading for all dentists. An overview of these practical radiation protection recommendations are reproduced in Chapter 7.
Examinations for occupational, medico-legal or insurance purposes
In the UK the 2001 Guidance Notes emphasize that the need for, and the usefulness of, these examinations should be critically assessed when deciding whether they are justified. They also recommend that these types of examinations should be requested only by medical/dental practitioners and that the patient’s consent should be obtained.
Radiation workers
The ICRP maximum dose limits for each group as shown in Table 6.3 is based on the principle that the risk to any worker who receives the full dose limit will be such that the worker will be at no greater risk than a worker in another hazardous, but non-radioactive, environment.
The main features of each group of radiation workers are summarized below:
Non-classified workers (most dental staff)
• Receive low levels of exposure to radiation at work (as in the dental surgery).
• The annual dose limits are 3/10 of the classified workers’ limits. Provided the Local Rules are observed, all dental staff should receive an annual effective dose of considerably less than the limit of 6 mSv. Hence, the regulations in the UK suggest the setting of ‘Dose Constraints’. These represent the upper level of individual dose that should not be exceeded in a well-managed practice, and for dental radiography the following recommendations are made:
| 1 mSv | for employees directly involved with the radiography (operators) |
| 0.3 mSv | for employees not directly involved with the radiography and for members of the general public. |
In addition to the above dose limits, the legal person must ensure that the dose to the fetus of any pregnant member of staff is unlikely to exceed 1 mSv during the declared term of the pregnancy.
• Personal monitoring (see Chapter 7) is not compulsory in the UK, although it is recommended if the risk assessment indicates that individual doses could exceed 1 mSv per year. The 2001 Guidance Notes state that in practice this should be considered for those staff whose weekly workload exceeds 100 intraoral or 50 panoramic images, or a pro-rata combination of each type of examination.
The radiation dose to dentists and their staff can come from:
The main practical radiation protection measures to limit the dose that workers receive are described in Chapter 7.
General public
This group includes everyone who is not receiving a radiation dose either as a patient or as a radiation worker, but who may be exposed inadvertently, for example, someone in a dental surgery waiting room, in other rooms in the building or passers-by. The annual dose limits for this group have been lowered to 1 mSv, as shown in Table 6.3 although the suggested dose constraint is 0.3 mSv (see earlier). The general public is at risk from the primary beam and the main practical radiation protection measures to limit the dose are described in Chapter 7.
To access the self assessment questions for this chapter please go to www.whaitesessentialsdentalradiography.com