R
radiant flux See flux, radiant.
radiation 1. Emission or transfer of energy in the form of electromagnetic waves or particles. 2. A group of nerve fibres that diverge in all directions from a point of origin. Example: the optic radiations.
See spectrum, electromagnetic.
radiation, black body The radiation emitted by a heated black body.
See colour temperature.
radiations, optic That part of the visual pathway which consists of axons arising in the lateral geniculate body and terminating in a fan-shaped manner in the visual area of the occipital lobe. As they emerge from the lateral geniculate body the inferior fibres loop forward in the temporal lobe before swinging back toward the occipital cortex. These fibres form what is called Meyer’s loop (or Archambault’s loop). They receive impulses from the inferior retinal quadrants (corresponding to the superior aspect of the contralateral visual field) and terminate on the inferior lip of the calcarine fissure. Syn. optic radiations of Gratiolet; geniculocalcarine pathway; geniculostriate pathway.
radiology A science dealing with techniques that use radiant energy (e.g. X-rays) for diagnosis and therapy.
See angiography, fluorescein; magnetic resonance imaging; tomography, computed.
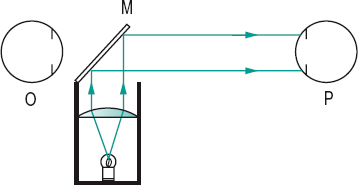
radiuscope Instrument used for measuring the radius of curvature of the surfaces of a contact lens. It is based on the Drysdale method. Syn. optical microspherometer.
See method, Drysdale’s; Toposcope.
Raman effect See effect, Raman.
Ramsden eyepiece See eyepiece, Ramsden.
ramus communicans See ganglion, ciliary; nerve, ophthalmic.
random-dot stereogram; E test See stereogram, random-dot.
randomized controlled trial See trial, randomized controlled.
range of accommodation See accommodation, range of.
ranibizumab See anti-VEGF drugs; macular degeneration, age-related; retinopathy, diabetic.
raphe, retinal See retinal raphe.
ratio, Arden See electrooculogram.
ratio, AV The ratio of the diameter of the retinal arteries to that of the retinal veins. It is usually around two-thirds. Deviations from this value may indicate a vascular disease (e.g. hypertension).
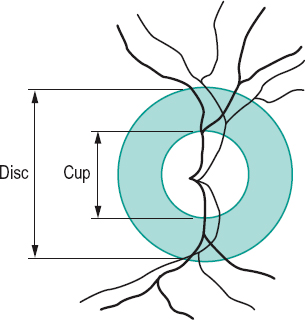
ratio, cup-disc (C/D) The ratio of the horizontal diameter of the physiological cup to that of the horizontal diameter of the optic disc. It should be less than 0.5. If it exceeds that value, or if there is a difference in ratio between the two eyes, or if there is a progressive enlargement of the cup, glaucoma may be suspected (Fig. R1).
See cup, glaucomatous.
Raubitschek chart See chart, Raubitschek.
ray In geometrical optics, a straight line representing the direction of propagation of light.
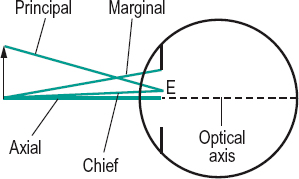
axial r. A ray that is coincident with the axis of an optical system.
chief r. A ray joining an object point to the centre of the entrance pupil of an optical system (Fig. R2).
emergent r. A ray of light in image space either after reflection (reflected ray) or after refraction (refracted ray).
extraordinary r. See birefringence.
incident r. A ray of light in object space that strikes a reflecting or refracting surface.
marginal r. A ray joining the axial point of an object to the edge or margin of an aperture or pupil (Fig. R2).
ordinary r. See birefringence.
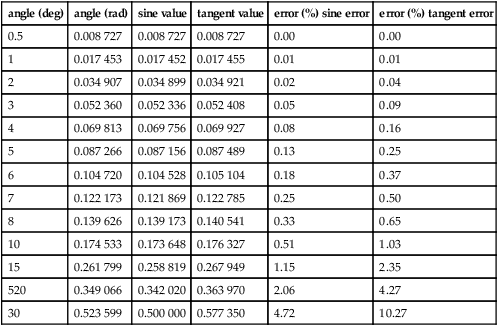
paraxial r. A light ray that forms an angle of incidence so small that its value in radians is almost equal to its sine or its tangent. (i.e. sin θ = θ or tan θ = θ. These are approximate expressions referred to as the paraxial approximation (or the gaussian approximation).
See optics, paraxial; paraxial region; theory, gaussian.
principal r. A ray joining the extreme off-axis object point to the centre of the entrance pupil or aperture (Fig. R2).
r. tracing Technique used in optical computation consisting of tracing the paths of light rays through an optical system by graphical methods or by using formulae. Nowadays, computer methods are used.
See sign convention.
Rayleigh criterion See criterion, Rayleigh.
Rayleigh equation A colour equation representing a match of yellow (usually 589 nm) with a mixture of red (usually 670 nm) and green (usually 535 nm). It is used to differentiate certain types of colour deficiencies. The anomaloscope is built on this principle.
See colour vision, defective.
Rayleigh scattering See scattering, Rayleigh.
reaction time The time interval between the onset of a stimulus and the response of a subject. Visual stimulations with a flash of light give rise to reaction times varying between 130 and 180 ms. This figure increases significantly with age.
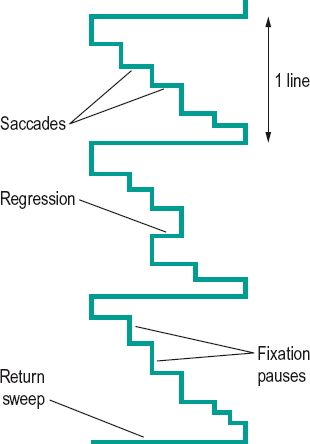
reading The act of viewing and interpreting letters, words, sentences, etc. It consists of a pattern of eye movements. The eyes proceed along a line in a series of step-like saccades, separated by fixation pauses during which information from the text is acquired. The amount of reading matter correctly identified during the fixation pause is called the span of recognition or the perceptual span. Most saccades are made from left to right, but some occur in the opposite direction (called regression) to return to text recently read but not yet fully perceived. At the end of the line the eyes make a return sweep to the next line of text (Fig. R3).
See movement, saccadic eye; test, developmental eye movement.
reading addition See addition, near.
reading distance; lens See under the nouns.
reading portion See segment of a bifocal lens.
Table R1
Differences between the sine and the tangent values of various angles (in degrees and radians). The error is calculated between the sine value and the value in radians and between the value in radians and the tangent value
| angle (deg) | angle (rad) | sine value | tangent value | error (%) sine error | error (%) tangent error |
| 0.5 | 0.008 727 | 0.008 727 | 0.008 727 | 0.00 | 0.00 |
| 1 | 0.017 453 | 0.017 452 | 0.017 455 | 0.01 | 0.01 |
| 2 | 0.034 907 | 0.034 899 | 0.034 921 | 0.02 | 0.04 |
| 3 | 0.052 360 | 0.052 336 | 0.052 408 | 0.05 | 0.09 |
| 4 | 0.069 813 | 0.069 756 | 0.069 927 | 0.08 | 0.16 |
| 5 | 0.087 266 | 0.087 156 | 0.087 489 | 0.13 | 0.25 |
| 6 | 0.104 720 | 0.104 528 | 0.105 104 | 0.18 | 0.37 |
| 7 | 0.122 173 | 0.121 869 | 0.122 785 | 0.25 | 0.50 |
| 8 | 0.139 626 | 0.139 173 | 0.140 541 | 0.33 | 0.65 |
| 10 | 0.174 533 | 0.173 648 | 0.176 327 | 0.51 | 1.03 |
| 15 | 0.261 799 | 0.258 819 | 0.267 949 | 1.15 | 2.35 |
| 520 | 0.349 066 | 0.342 020 | 0.363 970 | 2.06 | 4.27 |
| 30 | 0.523 599 | 0.500 000 | 0.577 350 | 4.72 | 10.27 |
reading slit See typoscope.
receptive field See field, receptive.
receptor See photoreceptor.
recession A surgical procedure used in strabismus in which an extraocular muscle is removed from its insertion and repositioned elsewhere on the globe, posteriorly to weaken it and anteriorly to strengthen it (called advancement procedure).
See resection; strabismus surgery.
recessive inheritance See inheritance.
reciprocal innervation See law of reciprocal innervation, Sherrington’s.
reciprocal metre See curvature of a surface.
reciprocity, law of See law, Bunsen–Roscoe.
von Recklinghausen’s disease See disease, von Recklinghausen’s.
recovery point See point, recovery.
rectus muscles See muscles.
recumbent spectacles See spectacles, recumbent.
recurrent corneal erosion See corneal erosion, recurrent.
red One of the hues of the visible spectrum evoked by stimulation of the retina by wavelengths beyond 630 nm. The complementary colours to red are blue-green (between 490.4 and 492.4 nm).
red blindness See protanopia.
red glass test See test, red glass.
red reflex See reflex, fundus.
red-green colour deficiency A general term indicating a colour vision deficiency, which is either of the deutan (green colour vision defect) or of the protan (red colour vision defect) type. These defects are mostly hereditary and affect both eyes equally. Most cases are inherited in X-linked recessive manner.
See colour vision, defective; rule, Kollner’s.
reduced eye; vergence See under the nouns.
refixation reflex See reflex, refixation.
reflectance A measure of reflection equal to the ratio of reflected luminous flux φ’ to the incident luminous flux φ, i.e. ρ = φ’/φ. Syn. reflection factor.
See Fresnel’s formula.
reflecting prism; telescope See under the nouns.
reflection Return or bending of light by a surface such that it continues to travel in the same medium.
angle of r. See angle of reflection.
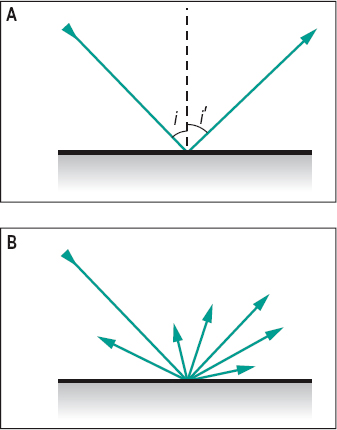
diffuse r. Reflection from a surface that is not polished and light is reflected in many or all directions (Fig. R4). Syn. irregular reflection.
See diffusion; glossmeter; matt surface.
direct r. See reflection, specular.
r. factor See reflectance.
irregular r. See reflection, diffuse.
law of r. See law of reflection.
mixed r. The simultaneous occurrence of diffuse and specular reflection.
regular r. See reflection, specular.
specular r. Reflection from a polished surface in which there is no scattering and light travels back in a definite direction (Fig. R4). Syn. direct reflection; regular reflection.
See microscope, specular.
surface r . Light reflected at a surface according to Fresnel’s formula.
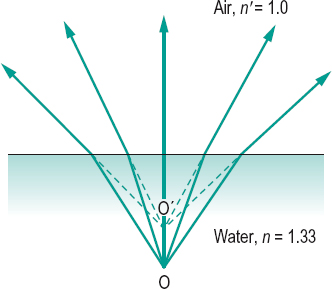
total r. Reflection occurring when light is incident at an angle greater than the critical angle. Syn. total internal reflection.
See prism, reflecting.
total internal r. See reflection, total.
reflector Any device that reflects light (e.g. glass-plate, prism, mirror).
reflex 1. Involuntary response to a stimulus. 2. Reflection or an image formed by reflection (e.g. corneal reflex).
accommodative r. See accommodation, reflex; reflex, near.
r. arc See reflex, pupil light.
blinking r. Blinking in response to various stimulations such as a light source or a mechanical threat.
See pathway, retinotectal.
cat’s eye r. A whitish, bright reflection observed in the normally black pupil in several conditions, such as leukocoria, retinoblastoma, Coats’ disease or persistent hyperplastic primary vitreous. It resembles the reflection from the tapetum lucidum of a cat when a light is shined at night.
consensual light r. See reflex, pupil light.
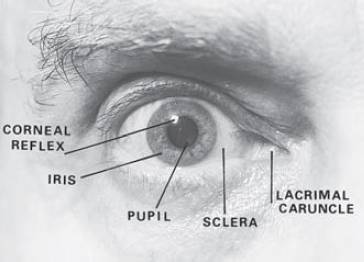
corneal r. 1. Blinking in response to a threat, or to tactile stimulation of the cornea, as for example when measuring objectively the corneal touch threshold. Associated responses include lacrimation and miosis. 2. Image formed by reflection of light from the cornea (Fig. R5).
See aesthesiometer; method, Hirschberg’s; method, Krimsky’s; pupillometer; strabismus, apparent.
direct light r. See reflex, pupil light.
eyeball compression r. See reflex, oculocardiac.
fixation r. Psycho-optical reflex consisting of an involuntary movement of the eye (or eyes) aimed at placing on the foveola the retinal image of an object that was formed in the retinal periphery.
See reflex, psycho-optical; reflex, re-fixation.
foveal r. Tiny reflection from the concave surface of the foveal depression of the retina seen in ophthalmoscopy. It is not usually visible in old eyes.
fundus r. Light reflected by the fundus of the eye, as seen in retinoscopy and ophthalmoscopy. It appears as a red glow in the plane of the pupil in retinoscopy. It is absent when the eye has a dense cataract. Syn. red reflex.
hemianopic pupillary r. In hemianopia, a loss of pupillary constriction when light falls on the blind side of the retina while pupillary constriction is maintained when light stimulates the unaffected side of the retina. Syn. Wernicke’s hemianopic pupil; Wernicke’s pupillary reaction; Wernicke’s pupillary reflex; Wernicke’s sign.
indirect light r . See reflex, pupil light.
lacrimal r. Secretion of tears in response to irritation of the cornea or conjunctiva as, for example, when first wearing contact lenses (hard in particular), but it may also be induced by eyestrain, glare, laughing, etc. Syn. lacrimation reflex; tearing reflex; weeping reflex.
See lacrimal apparatus; tear secretion; test, Schirmer’s.
lacrimation r. See reflex, lacrimal.
light r. 1. That light which appears in the pupil in retinoscopy. It is light reflected by the retina. Syn. retinoscopic light. 2. Any reflected light.
See reflex, pupil light.
near r. Reflex evoked by a blurred retinal image, as when fixating from far to near. It consists of three responses: (1) increased convexity of the crystalline lens; (2) constriction of the pupils; and (3) convergence of the eyes. This reflex is not a pure reflex since each of the three components can act independently of the other two; convergence by means of prisms, accommodation by means of lenses and miosis by light stimulation. Syn. accommodative reflex; near-triad reflex; synkinetic near reflex.
See accommodation, mechanism of; accommodation, reflex; accommodative response.
near-triad r. See reflex, near.
oculocardiac r. A decrease in pulse rate following compression of the eyeball or traction on the extraocular muscles during ocular surgery. It may produce a systolic cardiac arrest. Syn. Ascher’s phenomenon; Ascher’s reflex; eyeball compression reflex.
optokinetic r. See reflex, vestibulo-ocular.
postural r. A reflex which helps to maintain static or dynamic posture of the body, for example, the righting reflex, in which visual stimuli help to maintain a correct position of the head in space by activating the muscles of the neck and limbs.
See reflex, static eye.
psycho-optical r. Reflexes involving the eye which are mediated by the occipital cortex such as the accommodative, fixation, fusion, version and vergence reflexes.
pupil r. Any alteration of the pupil size in response to stimuli other than light (e.g. a sudden noise).
See reflex, pupil light.
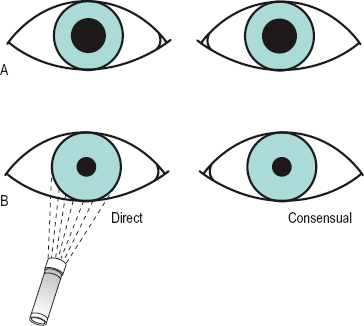
pupil light r. 1. Constriction of the pupil in response to light stimulation of the retina. The response of an eye to light stimulation can occur either with a light shining on it directly (the direct light reflex) or when the other eye is stimulated (the consensual or indirect light reflex). The reflex arc consists of four neurons beyond the ganglion cells. The first afferent neuron transmits nervous impulses from the retina to the two pretectal olivary nuclei, located on the lateral and anterior side of the superior colliculi, in response to light stimulation of the photoreceptors. The second neurons, called the internuncial neurons, connect each pretectal olivary nucleus to both Edinger–Westphal nuclei which form part of the oculomotor nuclei. The third efferent neurons connect the latter nuclei, via the third nerve (oculomotor nerve) to the ciliary ganglion where there is a synapse. The fourth efferent neurons connect the latter, via the short ciliary nerves, to the sphincter pupillae muscle of each iris and constrict the pupil. Light stimulation of the central region of the retina produces a greater pupillary response than peripheral stimulation. The efferent path for pupil constriction represents the parasympathetic innervation (Fig. R6). Note: recent research points to a different pathway for the second afferent neuron: almost all of the fibres from each pretectal olivary nucleus project to the contralateral Edinger–Westphal nucleus. 2. Dilatation of the pupil in response to a reduction of the light stimulation of the retina. It is effected by sympathetic innervation, which originates in the hypothalamus and descends down the brainstem to the ciliospinal centre (of Bulge), located between C8 and T2. From there fibres pass to the superior cervical ganglion in the neck, then efferent fibres ascend along the internal carotid artery until they join the ophthalmic division of the trigeminal nerve. The fibres reach the dilator pupillae muscle of the iris via the nasociliary and long ciliary nerves, which enter the eyeball behind the equator. Syn. light reflex.
See fibres, pupillary; pathway, retinotectal; pretectum; pupillary defect, efferent.
re-fixation r. This reflex occurs while fixating one object and another in the visual field attracts the attention. The eye then turns to fixate on the new object. This is a special case of the fixation reflex.
retinoscopic r. See reflex, light; retinoscope.
righting r. See reflex, postural.
static eye r . A higher order postural reflex which helps to maintain the eye static with respect to the visual environment by action on the extraocular muscles (possibly via the utricular receptors of the vestibular system) during head or body movements. Syn. compensatory eye movements.
r. tearing See reflex, lacrimal.
tonic neck r. Orientation of the head, eyes and body in response to proprioceptive information provided by the activity of the muscles of the neck.
See proprioception.
vergence r. A disjunctive fixation reflex in response to an object that moves closer or further than the original position of the fixation point.
See movements, disjunctive eye.
version r . A conjugate fixation reflex in response to an object moving in the same frontal plane.
See version.
vestibulo-ocular r. A conjugate movement of the eyes in the direction opposite to a head movement. This reflex is triggered by stimulation of the semicircular canals. It is aimed at maintaining a stable image on the retina during head movement. This reflex responds best at high velocities and frequencies of the visual stimulus. At low velocities and frequencies the stabilization of the retinal image is attempted by the optokinetic reflex, which is triggered only by retinal stimulation: this latter reflex complements the vestibulo-ocular reflex.
See nystagmus; optokinetic.
weeping r. See reflex, lacrimal.
Wernicke’s pupillary r. See reflex, hemianopic pupillary.
white pupillary r . See leukocoria.
refract 1. To bend a ray of light when it passes through a surface separating media of different refractive indices. 2. To measure the refractive state of the eye.
refracting angle See angle, prism.
refracting unit See phoropter.
refraction 1. The change in direction of the path of light as it passes obliquely from one medium to another having a different index of refraction (Fig. R7). 2. The process of measuring and correcting the refractive error of the eyes. Syn. refraction of the eye; sight testing (obsolete term). 3.
See refractive error.
See law of refraction.
angle of r . See angle of refraction.
binocular r. A clinical procedure in which the subjective measurement of refraction of each eye is performed while both eyes are viewing a test. The visual examination is thus carried out under more natural conditions than when one eye is closed; the sizes of the pupils are similar and the accommodationconvergence relationship is maintained.
There are various such methods; using polarized targets (e.g. Vectograph slides; Parallel-testing Infinity Balance test), using a septum (e.g. Turville Infinity Balance test), or fogging (e.g. Humphriss Immediate Contrast test). These methods give better results than refracting monocularly, especially in latent hyperopia, hyperopic anisometropia, pseudomyopia, cyclophoria, etc. and no additional step for binocular balancing is necessary.
See method, Humphriss; test, balancing; test, Turville, infinity balance; testing in parallel.
cycloplegic r. Assessment of the refractive state of the eye when accommodation has been totally or partially paralysed by a cycloplegic (e.g. cyclopentolate 1% eyedrops, or atropine 0.5 or 1% ointment). This may be carried out in children to reveal the full extent of a hyperopia or in the initial assessment of accommodative esotropia, but only occasionally in adults as fogging methods usually suffice for them.
See cycloplegia; strabismus, accommodative.
double r. The splitting of an incident ray into two (ordinary and extraordinary) by a birefringent medium.
See anisotropic; birefringence; prism, Nicol; prism, Wollaston.
dynamic r. Determination of the refractive state of the eye when accommodation is stimulated, as distinguished from static refraction which is the determination of the refractive state of the eye when accommodation is at rest or paralysed.
See refractive error; retinoscopy, dynamic.
error of r. See ametropia; refractive error.
r. of the eye 1. See refraction. 2. Refraction of light by the optical media of the eye. 3. Syn. for ametropia.
See ametropia; refractive error.
index of r. See index of refraction.
laser r. A method of subjective refraction in which the patient observes a slowly rotating drum, on the surface of which is perceived a speckle pattern resulting from illumination by a laser. The speckle pattern appears to move only when the eye is not focused for the fixation distance. If the perceived movement of the pattern is opposite to that of the drum, the eye is myopic and if the perceived movement of the pattern is in the same direction as the drum, the eye is hyperopic. Correction can be determined by placing a lens in front of the eye, which will neutralize the movement; at that point the eye is focused for the fixation distance. Astigmatism can be measured by rotating the drum in various meridians. The drum can be placed at infinity or at near (an allowance for the radius of curvature of the drum and the distance must then be made). This method can be useful for mass screening, especially children, as accommodation is not stimulated as much as with Snellen letters. It has been very useful as a research tool for accommodation studies where it is arranged as part of a Badal optometer.
manifest r. The refractive error or the process of determining it, when accommodation is at rest (but not paralysed).
See refraction, cycloplegic.
objective r. Measurement of the refraction of the eye that is not based on the patient’s judgements, as when using an objective optometer or a retinoscope.
See photorefraction.
static r. See refraction, dynamic; refractive error.
subjective r. Measurement of the refraction of the eye based on the patient’s judgements.
See method, fogging; optometer; test, duochrome; test, fan and block; test, plus 1.00 D blur.
refractionist One who measures and corrects the refractive state of the eye.
See optometrist.
refractive amblyopia See amblyopia.
refractive correction See correction.
refractive error The dioptric power (K) of the ametropia of the eye. It is equal to 1/k in dioptres, where k is the distance between the far point and either the spectacle plane (spectacle refraction), or the principal point of the eye, or the refracting surface of the reduced eye (ocular refraction), in metres. Thus
< ?xml:namespace prefix = "mml" />

when the eye is situated in air. Syn. ametropia (although this is not strictly so as ametropia is the anomaly); refraction of the eye; refractive status; static refraction.
See accommodation, far point of; experiment, Scheiner’s.
refractive index See index of refraction.
refractive surgery Surgical procedure aimed at correcting ametropia. Most procedures are performed on the cornea, but some involve either an intraocular lens implant, or more rarely crystalline lens extraction.
See epikeratoplasty; Intacs; keratomileusis; keratophakia; keratectomy, photorefractive; LASIK; LASEK.
refractive power See power, refractive.
refractivity See dispersion.
refractometer 1. An instrument for measuring the refractive index of transparent objects. There exist several types: Abbé’s refractometer, which is based on the measurement of the critical angle at the interface between a sample and a prism of known index of refraction and uses white light whereas that of Pulfrich, which is based on the same principle as Abbé’s, uses monochromatic light. As the refractive index of some materials is related to their water content, the handheld Atago CL-1 Soft lens Refractometer has been calibrated to provide a reading of the percentage of water content of soft contact lenses. 2.
See optometer.
refractometry 1. Measurement of the refractive error of the eye with a refractometer or optometer. 2. Measurement of the index of refraction of a medium with a refractometer (e.g. Abbé’s refractometer).
refractor See phoropter.
refractory period See potential, action.
Rieger’s syndrome See syndrome, Rieger’s.
Reis–Buckler dystrophy See dystrophy, Reis– Buckler.
Reiter’s disease See disease, Reiter’s.
relative afferent pupillary defect See pupil, Marcus Gunn.
relative amplitude of accommodation; convergence; scotoma See under the nouns.
reliability The extent to which multiple measurements of the same thing, made on separate occasions, yield approximately the same results. The reliability between two sets of scores can be assessed by determining the correlation coefficient (test-retest reliability coefficient).
See validity.
relief 1. Quality of an object or of different parts of a surface to stick out from the background or general plane in which it is situated. The perception of relief is a special case of depth perception. 2. A feeling of gladness that something unpleasant or painful has not occurred or has ceased.
See perception, depth; stereopsis.
relieving prism See prism, relieving.
remotum, punctum See accommodation, far point of.
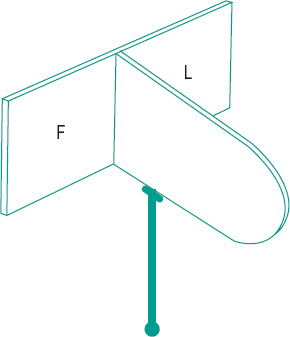
Remy separator A simple, handheld instrument for separating the vision of both eyes and commonly used for anti-suppression or divergence training. It consists of a vertical septum in the median plane, which is attached to, and divides a target holder at one end. The other end of the septum rests against the patient’s nose so that a target on either side of the septum is seen by only one eye (Fig. R8).
See suppression.
resection A surgical procedure used in strabismus in which a portion of an extraocular muscle is removed (usually at its insertion) and the muscle is reattached at or near the original site of insertion. This is carried out to shorten and strengthen the muscle.
See enophthalmos; recession; strabismus surgery.
residual astigmatism See astigmatism, residual.
residual error of refraction See over-refraction.
reserve of accommodation See addition, near.
reserve, convergence fusional See convergence, relative.
resolution, limit of The least separation of two images so that they are seen as separate when viewed through an optical instrument. This is usually evaluated in terms of the separation between the maximum of the intensity distribution curve of the diffraction pattern (or Airy’s disc) of the images; it is commonly assumed that two points will be resolved if the centre of one pattern falls on the first dark ring of the other. The limit of resolution is greater the larger the aperture of the system. Syn. resolving power; resolution threshold.
See criterion, Rayleigh; minimum separable.
resolution, spurious If the contrast sensitivity function (CSF) is measured when the eye is not in focus for the grating (e.g. due to a lack of correction or an erroneous correction), the CSF will suffer appreciably and fall much more rapidly with increasing spatial frequency towards zero contrast sensitivity. At this point the grating can no longer be resolved and appears a uniform grey. At spatial frequencies greater than this threshold value there may occur a phenomenon known as spurious resolution in which the CSF rises above zero. Thus, the grating may become visible again at higher spatial frequencies than that at which it first disappeared. Example: spurious resolution can be observed when looking at a radial grating (or star sector target) in which the spatial frequencies increase towards its centre. If the grating is held close to the eye with the accommodation relaxed one can see a grey annulus (and sometimes two) separating a zone (or two) of spurious resolution.
See function, contrast sensitivity.
resolution visual acuity See acuity, visual.
response, SILO An acronym for small in large out. It refers to the presumed change of the perceived size of a test object that a patient experiences, while maintaining fusion when convergence or divergence is varied. When convergence is increased, with BO prisms, the object may appear to become smaller and nearer. When divergence is increased with BI prisms the object may appear larger and further away. The SILO is not universal; children tend to respond that way, but adults commonly respond in the opposite way, that is, if the test object becomes smaller they report it as moving away from them. The acronym is then given as SOLI. The response is used in visual therapy as a feedback mechanism to patients about their performance.
See base setting; biofeedback; fusion, sensory.
restriction An interference in normal eye movement. This is most often due to the development of abnormal tissue that acts to limit free movement of the eye.
ret See retinoscopy.
reticule See graticule.
reticulosis See syndrome, Mikulicz’s.
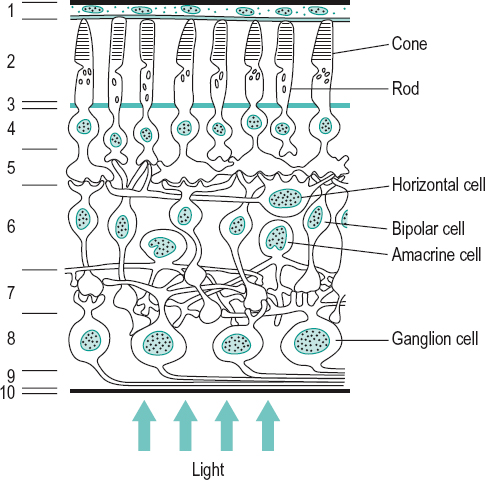
retina The light-receptive, innermost nervous tunic of the eye. It is a thin transparent membrane (about 125 μm near the ora serrata, 350 μm near the macula and 560 μm near the optic disc). The retina proper has an area of about 266 mm2. It lies between the vitreous body and the choroid, and extends from the optic disc to the ora serrata. Near the posterior pole and temporal to the optic disc is the macula, at the centre of which is the foveola which provides the best visual acuity. The retina contains at least 10 distinct layers, of which there are two synaptic layers. They are from the outermost layer to the innermost: (1) the pigment epithelium; (2) the layer of rods and cones; (3) the external limiting membrane; (4) the outer nuclear layer; (5) the outer molecular (outer plexiform) layer; (6) the inner nuclear layer (which contains the bipolar, amacrine and horizontal cells and nuclei of the fibres of Mueller); (7) the inner molecular (inner plexiform) layer; (8) the ganglion cell layer; (9) the nerve fibre (layer stratum opticum); and (10) the internal limiting membrane. The two synaptic layers where visual signals must synapse as they emerge from the rods and cones on their way to the optic nerve are the two molecular layers (5 and 7) (Fig. R9). The blood supply to the retina is composed of the capillaries from the central retinal artery, which supply the inner two-thirds of the retina up to the outer plexiform layer, and the choriocapillaris, which supplies the outer one-third. There is no retinal circulation in the foveola (avascular zone). A blood-retina barrier is created by the walls of the retinal capillaries which restrict the movement of molecules, which could be damaging to neural tissue or interfere with function, from the inside to the outside of the capillaries. The blood-retina barrier in the outer third of the retina is formed by the tight junctions of the retinal pigment epithelium cells.
See astrocytes; cup, optic; disc, optic; ectoderm; fundus, ocular; layer of Henle, fibre; macula; neurotransmitter; retina, neurosensory; retinitis; retinopathy; rhodopsin; transduction.
converse r. See retina, inverted.
fleck r. Term referring to a retina with multiple, small or yellow spots, which are seen in various conditions: actinic keratopathy, drusen, fundus albipunctatus, fundus flavimaculatus.
Table R2
Some approximate retinal dimensions
| diameter | |||
| structure | mm | degrees | distance from centre of foveola |
| foveola | 0.4 | 1.3 | |
| fovea centralis | 1.5 | 5.0 | |
| macula lutea | 4.0 | 14 | |
| optic disc* | |||
| horizontal | 1.8 | 6.0 | |
| vertical | 2.1 | 7.5 | |
| nasal disc margin | 5.5 mm or 18.5° | ||
| temporal disc margin | 3.5 mm or 12.5° | ||
| centre of disc | 4.6 mm or 15.5° |
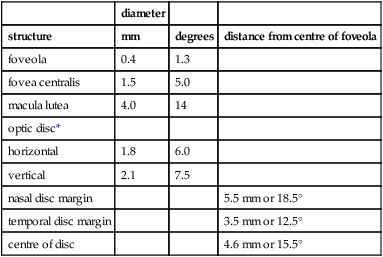
*The figures given for the size of the disc are those corresponding to the blind spot. Anatomically the optic disc is slightly smaller.
inverted r. Term referring to the fact that the retina of vertebrates is orientated so that the light has to pass through all the neuronal layers before reaching the photoreceptors. However, the retina of invertebrates is normally orientated so that light passes first through the photoreceptors as it traverses the retina: such a retina is called a verted or converse retina.
lattice degeneration of the r. A vitreoretinal degeneration usually found between the equator and the ora serrata leading to a thinning of the retina and characterized by a lesion made up of fine white lines and some pigmentation. It may result in holes or tears and in rhegmatogenous retinal detachment by which time the patient usually complains of floaters. The condition is most common in myopes and often found in patients with Marfan’s syndrome.
See retinal break; retinal detachment; retinoschisis; syndrome, Marfan’s.
leopard r. See fundus, leopard.
neurosensory r. This is composed of all the layers of the retina, except the outer pigmented layer (called retinal pigment epithelium). It comprises three main groups of neurons: (1) the photoreceptors, (2) the bipolar cells, and (3) the ganglion cells. In addition, there are other connecting neurons: the horizontal and amacrine cells. The neurosensory layer is derived embryologically from the inner layer of the optic cup whereas the pigmented layer is derived from the outer layer of the optic cup and they are separated by a potential space which facilitates their separation, as occurs in detached retina. Syn. sensory retina.
tessellated r. See fundus, tessellated.
tigroid r. See fundus, tessellated.
verted r. See retina, inverted.
retinal 1. Pertaining to the retina. 2. See rhodopsin.
retinal arterial occlusion Occlusion of the central retinal artery (CRAO) is characterized by a sudden loss of vision and a defective direct pupil light reflex. The retinal arterioles are constricted while the veins are full but a venous pulse is absent. The retina appears white and swollen, especially near the posterior pole, and the choroid is seen through it as a cherry-red spot (Fig. S12). If the occlusion persists the cherry-red spot disappears after several weeks, the retinal arterioles remain attenuated, eventually becoming white threads, and the optic disc becomes atrophic.
Occlusion is more frequently limited to one branch of the central retinal artery (BRAO). In this case, the clinical picture is limited to the area supplied by the branch and this is associated with a visual field defect in that region. Causes include retinal emboli due to a cardiovascular disease, systemic hypertension, temporal arteritis, oral contraceptives, syphilis, intravenous drug abuse or trauma. Treatment is urgent as there is an extremely serious risk of blindness.
See amaurosis fugax; angiography, fluorescein; atheroma; plaques, Hollenhorst’s; spot, cherry-red.
retinal break A full thickness opening in the neurosensory retina. It may be a hole, usually due to atrophy of the retina and often overlaid by an operculum; or a tear, horseshoe-shaped (U-shaped), round or slitlike, usually caused by posterior vitreous detachment in which the vitreous adheres to the retina and pulls it from the point of adherence during or just after an abrupt eye movement; or a giant retinal tear which involves 90° or more of the circumference of the globe and is commonly associated with Marfan’s syndrome or Stickler’s syndrome; or retinal dialysis which is usually the result of trauma. The patient may complain of photopsia, seeing floaters or flashes and some visual field defects and they may present with a vitreous haemorrhage. Management of retinal breaks includes localized laser photocoagulation (laser retinopexy) or cryopexy, a method of cryotherapy (freezing of the tissues causing local protein denaturation which leads to adhesion of the retina to the pigment epithelium), as the defect may lead to rhegmatogenous or tractional retinal detachment.
See macular hole; retinal dialysis; retinoschisis; sign, Shafer’s.
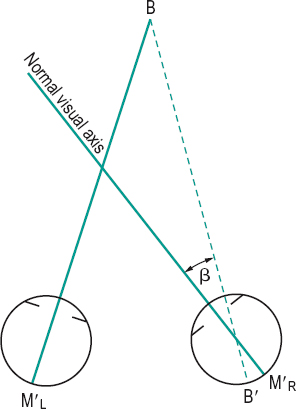
retinal correspondence, abnormal (ARC) A type of retinal correspondence in which the fovea of one eye is associated with an extrafoveal area of the other eye to give rise to a perception of a single object. This phenomenon is common in strabismus, but may also occur as a result of a macular lesion. ARC is often classified in three types: (1) Harmonious, in which the angle of anomaly is equal to the objective angle of deviation. This indicates that the ARC fully corresponds to the strabismus. (2) Unharmonious, in which the angle of anomaly is less than the objective angle of deviation. (3) Paradoxical, when the angle of anomaly is greater than the objective angle of deviation. ARC can be detected by examination with a major amblyoscope, with the after-image test, or by comparison between the objective and the subjective angles of deviation measured with the alternate cover test and either a Maddox rod or the von Graefe’s test, respectively (a difference between the objective and the subjective angles indicates ARC) (Fig. R10). Syn. anomalous retinal correspondence; retinal incongruity.
See diplopia, incongruous; diplopia, physiological; movement, phi; test, after-image; test, Bagolini’s.
retinal corresponding points Two points (or small areas), one in each retina, which when simultaneously stimulated give rise to the perception of a single object. These points share a common line of direction and this explains why stimulating them is perceived as arising from the same point in space. Syn. normal retinal correspondence (NRC).
See area, Panum’s; disparity, retinal; horopter; law of identical visual directions; test, after-image transfer.
retinal detachment (RD) Separation of the neurosensory retina from the pigment epithelium layer. There are three main types: rhegmatogenous retinal detachment, which is the most common type, exudative (serous or secondary) retinal detachment, and traction retinal detachment.
See cryotherapy; macular hole; metamorphopsia; photocoagulation; retina, lattice degeneration of the; retinal break; retinal dialysis; retinopathy, central serous; retinopathy of prematurity; striae retinae; syndrome, Ehlers–Danlos; syndrome, Marfan’s; syndrome, Stickler’s; ultrasonography; vitreoretinopathy, familial exudative; vitreous detachment.
exudative r. d. A separation of the sensory retina from the retinal pigment epithelium due to fluid accumulating in the subretinal space in the absence of a retinal break or preretinal traction following damage to the blood-retina barrier of the choriocapillaris. Common causes are choroidal tumour, posterior uveitis, exudative age-related macular degeneration, uveal effusion syndrome, Coats’ disease and central serous retinopathy. The patient notices a loss of vision in the area of the visual field corresponding to the detached area, reduced VA if the macula is involved, and floaters if there is an associated inflammation. The elevation is smooth and convex and the subretinal fluid shifts the area which is detached when the head moves (referred to as ‘shifting fluid’). Treatment is aimed at the primary cause. Syn. serous retinal detachment; secondary retinal detachment.
rhegmatogenous r. d. A separation of the sensory retina from the retinal pigment epithelium due to fluid from the vitreous entering the subretinal space through a tear or break in the retina. The retinal breaks are most commonly the result of posterior vitreous detachment (PVD), which is found in a large percentage of patients older than 70 years, in aphakic eyes, and in degenerative myopic eyes. Retinal breaks may also occur as a result of trauma and occasionally ocular surgery. The patient notices floaters, flashes, photopsia and a loss of vision in one area of the visual field corresponding to the detached area. Management may involve scleral buckling (indenting the sclera over the retinal break) and usually draining the subretinal fluid, or pneumatic retinopexy (the retinal break is sealed and the retina reattached using an intravitreal gas bubble).
tractional r. d. A separation of the sensory retina from the retinal pigment epithelium due to contraction of vitreoretinal fibroproliferative membranes, which pull the retina away from the pigment epithelium. The main causes are proliferative diabetic retinopathy, retinopathy of prematurity, sickle-cell retinopathy and perforating ocular injury. Ophthalmoscopically the detachment typically appears concave. The condition is often asymptomatic. Treatment is aimed at releasing the vitreoretinal traction.
See vitrectomy.
retinal dialysis A retinal tear at the ora serrata. It usually results from trauma, although some tears occur spontaneously. If the trauma is intense there may also be a retinal break at the optic disc but the most frequent location is in the lower temporal quadrant. The condition is most typically asymptomatic. However, as it often gives rise to retinal detachment, the patient may report some of the symptoms associated with the latter. Perimetry and binocular indirect ophthalmoscopy are essential in the examination of this condition. In some cases the tear does not progress, but because of the risk of retinal detachment, patients must be referred to a retinal specialist. Syn. retinal disinsertion.
See retinal break.
retinal disinsertion See retinal dialysis.
retinal disparity See disparity, retinal.
retinal embolism Obstruction of a retinal artery or arteriole by a clot (embolus), which may result in atrophy or blindness in the area of the retina affected.
See retinal arterial occlusion.
retinal glioma See retinoblastoma.
retinal hypoxia See hypoxia.
retinal illuminance Luminous flux incident on the retina. The simplified formula is

where L is the luminance of the stimulus in cd/m2 and S is the area of the pupil in mm2. The retinal illuminance T is then given in trolands. Retinal illuminance decreases with age due to absorption of the lens and to a reduction in pupil size. It may represent a reduction of as much as 30 fold in an 80-year-old eye as compared to a 20-year-old eye. Syn. retinal illumination.
See troland; vignetting.
retinal image, stabilized See stabilized retinal image.
retinal incongruity See retinal correspondence, abnormal.
retinal line See line, retinal.
retinal mosaic The pattern formed by the distribution of the retinal visual cells and their interspaces.
retinal necrosis, acute A necrotizing retinitis caused by the varicella-zoster virus or herpes simplex virus types 1 and 2, which may infect healthy individuals of any age. The patient usually presents with ocular discomfort, reduced visual acuity and floaters. The signs are those of anterior granulomatous uveitis. There are typically many areas of retinitis, which eventually coalesce ending in full thickness retinal necrosis. Treatment is with antiviral agents, followed by systemic steroids.
retinal necrosis, progressive outer A very rare and devastating necrotizing retinitis caused by the varicella-zoster virus, usually occurring in patients with AIDS. There is less inflammation than in acute form, many lesions on the retina eventually end in full thickness retinal necrosis and rapid progressive visual loss. The prognosis is usually poor.
retinal nerve fibre layer See glaucoma detection.
retinal pigment epithelium (RPE) A brown monolayer of cells of the retina situated next to the choroid composed of cells joined by tight junctions and filled with pigment, mainly melanin and lipofuscin (Fig. R9). Depending upon the amount of pigment, the fundus will appear dark or light. The main functions of the RPE are: control of the flow of fluid and nutrients entering the retina (blood-retina barrier), absorption of scattered light, visual pigment metabolism, vitamin A metabolism which contributes to visual pigment regeneration, ingestion and digestion of photoreceptor discs (phagocytosis), retinal adhesion and synthesis of growth factors of adjacent tissues. A dysfunction of this tissue can be detected with the electrooculogram.
See membrane, Bruch’s; syndrome, Usher’s.
retinal pigment epithelium, congenital hypertrophy of the (CHRPE) A benign congenital proliferation of the retinal pigment epithelium which may appear unilaterally as a dark-grey or black, round or oval lesion in the fundus (typical form) or in other cases as multiple smaller lesions grouped together and resembling ‘bear tracks’. In atypical form the lesions are bilateral. The latter is associated with familial adenomatous polyposis (an inherited condition characterized by neoplasms derived from epithelial tissue which appear as polyps throughout the rectum and colon and may become malignant) and its variants, Turcot syndrome (neuroepithelial tumours in the central nervous system) or Gardner’s syndrome (soft tissue tumours).
retinal pigment epithelium hyperplasia An abnormal proliferation of retinal pigment epithelium. This condition is thought to be due to persistent, abnormal traction on the RPE, causing it to proliferate. This finding has been noted along the vitreous base as well as in areas of inflammation and trauma. There is no particular visual significance to this lesion.
retinal raphe A horizontal line of demarcation, on the temporal side of the macula, separating the arcuate nerve fibres from the upper and lower retina.
See fibres, papillomacular; scotoma, arcuate; scotoma, Bjerrum’s.
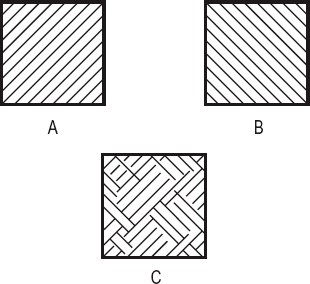
retinal rivalry When the two eyes are simultaneously or successively stimulated on corresponding retinal areas by dissimilar images (e.g. a green source to one eye and a red to the other, or lines orientated in one direction to one eye and in the other direction to the other), there results either an alternation of perception (complete or partial) or even a constant dominance of one eye. (Fig. R11) Syn. binocular rivalry.
See effect, Cheshire cat; suppression.
retinal slip See disparity, retinal.
retinal tear See retinal break.
retinal telangiectasia See disease, Coats’.
retinal vasculitis See disease, Eales’.
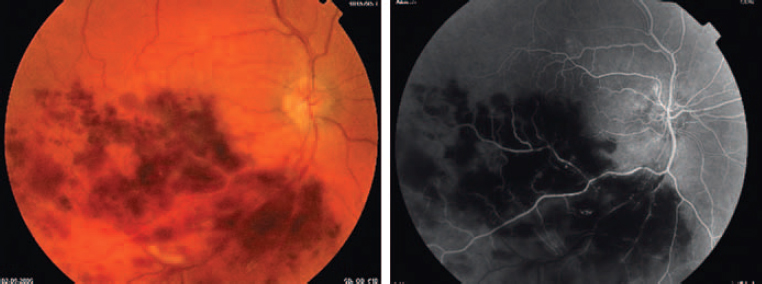
retinal vein occlusion Occlusion of the central retinal vein (CRVO) can be either non-ischaemic CRVO (venous-stasis retinopathy) which is the most common type, or ischaemic CRVO (haemorrhagic retinopathy). Predisposing causes are cardiovascular disease, systemic hypertension, diabetes or raised intraocular pressure. Non-ischaemic CRVO is characterized by some loss of vision, metamorphopsia, slight impairment of the pupil responses to light and partial or complete central scotoma due to macular oedema. The ophthalmoscopic picture shows retinal haemorrhages, flame-shaped in appearance and distributed throughout the whole fundus, dilated and tortuous veins and a swollen optic disc. In some cases cotton-wool exudates are also noted. When the condition affects young adults it is commonly referred to as papillophlebitis (optic disc vasculitis) in which the clinical picture is similar except that the pupillary responses to light are normal and the patient is often asymptomatic. Ischaemic CRVO, which usually affects older people, is a more severe type and the signs and symptoms are much more marked than in the non-ischaemic type.
Occlusion is more frequently limited to one branch of the central retinal vein (BRVO). In this case the clinical picture is limited to the retinal area drained by the occluded branch, but most patients will have some loss of vision depending on the extent of the macular oedema. Many eyes with BVRO have been found to be hyperopic. Treatment depends on the primary cause. Photocoagulation is used in some cases (Fig. R12).
See angiography, fluorescein; rubeosis iridis; vein, central retinal.
retinex A theory proposed to explain colour and brightness perception and constancies. It postulates that the colour of an object is not determined by the spectral composition of the light stimulus coming from an object, but is determined by information obtained from a comparison of three lightnesses generated by the light absorption of the three types of cone cell. The name of the theory ‘retinex’ reflects the fact that the perception of the image results from the retina and the cortex.
See pigment visual.
retinitis Inflammation of the retina. This usually follows inflammations of the vitreous body, retinal vessels and especially of the choroid. Retinitis leads to an exudation of cells into the vitreous body and, if serious, vision will be affected. If the inflammation affects the macular area there will be a loss of central vision. Haemorrhages and oedema (producing a blurring of the margins of the optic disc) are also usually present.
See retinal necrosis.
retinitis, cytomegalovirus (CMV retinitis) A rare, chronic, diffuse infection of the retina caused by the cytomegalovirus (CMV), a member of the herpesvirus group. It affects people with an impaired immune system as a result of either AIDS, organ transplantation or chemotherapy for some malignancies such as leukaemia. The signs are whitish retinal lesions, which look granular (not fluffy, cotton-wool spots). These lesions progress into retinal necrosis with absolute visual field loss in that area. The lesions are usually accompanied by haemorrhages. Eventually the lesions coalesce and involve the entire fundus, resulting in complete visual loss. In the initial phase of the disease most patients are usually asymptomatic while those with symptoms will complain of floaters, blurred vision, photopsia, scotomas, metamorphopsia, etc. In some cases, retinal detachment follows the disease. Treatment with dihydroxy propoxymethyl guanine and ganciclovir produces some regression of the disease.
See syndrome, acquired immunodeficiency.
retinitis pigmentosa (RP) A primary pigmentary dystrophy of the retina followed by migration of pigment. It is in most cases an inherited disease caused by abnormalities of many genes and characterized by night blindness (nyctalopia) and constricted visual fields. The inheritance can be autosomal dominant, autosomal recessive or X-linked. Many cases are caused by mutations in the rhodopsin gene (RHO). The condition is usually bilaterally symmetrical. The rod system is damaged but cones are also involved to some degree and the electroretinogram amplitude is subnormal. The disease usually begins in adolescence with night blindness, followed by a ring scotoma in the periphery that spreads until only a small contracted central field remains and vision is greatly reduced or completely lost. Ophthalmoscopic examination reveals a yellowish atrophy of the optic nerve, severe arterial attenuation and conspicuous pigment proliferation, which begins in the equatorial region. The areas of pigment have dense centres and irregular processes shaped like bone corpuscles. There are several variants (atypical RP) of pigment distributions and patterns throughout the fundus (e.g. in mainly one quadrant) or as retinitis punctata albescens (scattered white dots most numerous at the equator). Associated systemic syndromes include Bassen–Kornzweig, Kearns–Sayre, Laurence–Moon–Bardet–Biedl, Refsum’s and Usher’s. Syn. primary pigmentary retinal dystrophy.
See field, visual field; fundus, leopard; tritanopia; vision, tunnel.
retinitis proliferans See retinopathy, proliferative.
retinitis punctata albescens See retinitis pigmentosa.
retinitis, solar See retinopathy, solar.
retinoblastoma A congenital malignant tumour of the retina usually noted in the first two years of life, although in some cases it may not be until after age five years. It is the most common intraocular tumour of childhood. The condition is inherited in about 40% of all cases. The predisposing gene (RB1) is located on chromosome 13q14. Most individuals who inherit a mutant copy of the retinoblastoma gene sustain a second hit to the remaining normal copy of the gene and develop the disease. The most common ocular manifestations are leukokoria and strabismus and sometimes, red eye, glaucoma and orbital cellulitis. Diagnosis is usually made by the appearance of a greyish reflex of light observed at the pupil, although often by that time the pupil is fixed and the eye is blind. Computerized tomography is useful in imaging the tumour. Treatment includes external beam radiotherapy, photocoagulation, cryotherapy and chemotherapy while advanced tumours are managed by enucleation. Syn. retinal glioma.
See chromosome; penetrance; reflex, cat’s eye.
retinochoroiditis Inflammation of both the retina and the choroid.
See toxoplasmosis.
retinochoroidopathy, birdshot A bilateral, chronic condition which appears in middle-aged individuals, over 90% of whom are HLA-A29 positive, suggesting a genetic predisposition. The clinical picture is varied: multiple cream-yellow circular or oval spots spread throughout the posterior fundus, vitritis, cystoid macular oedema and eventually optic atrophy. Choroidal neovascularization (CNV) is a common complication. Symptoms are reduction of visual acuity, floaters, colour vision defects and nyctalopia. Treatment includes corticosteroids and/or immunosuppressants.
retinol See vitamin A deficiency.
retinopathy A disease of the retina.
See retinitis; tritanopia.
arteriosclerotic r. See arteriosclerosis.
background diabetic r. A progressive microangiopathy of the retinal vessels occurring in the early stage of diabetic retinopathy. It is characterized by microaneurysms, dot-blot haemorrhages, flame-shaped haemorrhages, hard exudates and retinal oedema. Retinal veins may also become dilated and tortuous. If the microvascular occlusion progresses there will be signs of ischaemia and multiple cotton-wool spots will appear, as well as more venous changes and maculopathy, producing the clinical picture of preproliferative diabetic retinopathy. If the macular oedema is not clinically significant the patient remains asymptomatic. Syn. non-proliferative diabetic retinopathy (NPDR).
central serous r. (CSR) An accumulation of serous fluid in the subretinal space, which leads to a retinal detachment. It usually occurs in the central area of the retina and results in a sudden blurring and/or distortion of vision. The condition typically affects stressed men between the ages of 20 and 45 years. It subsides by itself within a few months in most cases; otherwise photocoagulation may be necessary. Syn. central serous chorioretinopathy.
diabetic r. (DR) Retinal changes occurring in long standing cases of diabetes mellitus. It is the most common retinal vascular disease. In general, the severity of the retinopathy parallels the duration of the diabetes. The retinopathy is characterized by the presence of new blood vessels (neovascularization), which proliferate on or near the optic disc on the surface of the retina, microaneurysms (small round red spots) and sharply defined white or yellowish waxy exudates. Vitreous detachment is a likely outcome. If the vessels bleed, there can be a preretinal haemorrhage with visual loss. Both eyes are usually involved although to different degrees. Visual acuity may be unaffected unless the fovea is involved. After the condition has reached the stage of proliferative retinopathy, the principal treatment is with laser photocoagulation, which reduces the risk of further visual loss. Other treatments include intravitreal injections of a corticosteroid (e.g. triamcinolone) or of an anti-VEGF drug such as bevacizumab or ranibizumab. Low vision aids may be needed afterward. Syn. diabetic retinitis; proliferative diabetic retinopathy (PDR).
See angiography, fluorescein; diabetes; maculopathy, diabetic; microaneurysm; retinopathy, proliferative.
haemorrhagic r. See retinal vein occlusion.
hypertensive r. Retinal changes occurring as a result of systemic hypertension (essential hypertension). Most cases are chronic but in a very small percentage of patients it is acute (malignant hypertension). The condition is characterized by local and/or generalized narrowing of the arterioles, changes at arteriovenous crossings (Salus’ sign) and ‘copperwire’ arteriolar light reflex (grades 1 and 2). As the condition progresses, flame-shaped haemorrhages, cotton-wool exudates, oedema and changes at arteriovenous crossings (Gunn’s crossing sign) appear (grade 3) and at the most advanced stage (grade 4) the arteriolar reflex becomes ‘silver-wire’ and papilloedema occurs. Patients are usually asymptomatic. Malignant hypertension (accelerated hypertension), which is typically found in young patients, is more damaging with involvement of the choroidal arteries (hypertensive choroidopathy), along with Elschnig’s spots and Siegrist’s streaks, optic neuropathy and exudative retinal detachment. Note: the grading of hypertensive retinopathy is the Keith–Wagener–Barker classification.
See arteriosclerosis; exudate; hypertension; macular star; sphygmomanometer.
non-proliferative r. See retinopathy, background diabetic.
pigmentary r. A term commonly used as a synonym of retinitis pigmentosa.
r. of prematurity (ROP) A bilateral retinal disease which commonly affects premature infants exposed to high ambient oxygen concentrations. It is characterized by proliferation and tortuosity of blood vessels, usually with haemorrhages and retinal detachment accompanied by an accumulation of fibrous tissue on the surface of the retina. Some of the infants may develop cicatricial complications, which may be innocuous or may progress to cover the central region of the retina and cause blindness. Other complications may be myopia or glaucoma. This condition is less common nowadays. Syn. retrolental fibroplasias (RLF).
See leukocoria.
proliferative r. Neovascularization of the retina extending into the vitreous with connective tissue proliferation surrounding the vessels. The vessels usually arise from a retinal vein near an arteriovenous crossing at the posterior pole and from the surface of the optic disc. It occurs as a result of certain inflammatory conditions and in diabetes. Visual acuity may be affected. Syn. retinitis proliferans.
See fibrosis, preretinal macular; retinopathy, diabetic; vitrectomy.
solar r. Macular damage caused by fixating the sun without adequate protection, usually viewing a solar eclipse, but also in people staring at the sun as part of sun worship or psychosis. The retina presents at first with retinal oedema, which may develop into an atrophy of the tissue and produce a circumscribed hole or cyst in the fovea. This latter event results in a permanent central scotoma. There is no specific treatment but the condition can be prevented by wearing very dense light filters or viewing through photographic films. Syn. eclipse retinopathy; foveomacular retinitis; solar retinitis.
See actinic; macular hole.
toxaemic r. of pregnancy Sudden angiospasm of retinal arterioles, later followed by the typical picture of advanced hypertensive retinopathy. Restitution follows rapidly after the pregnancy has reached full term.
venous-stasis r. See retinal vein occlusion.
retinopexy See retinal break.
retinoschisis A vitreoretinal degeneration characterized by splitting of the retina into two layers. It occurs either as a hereditary disease or as an acquired condition (70% of these patients are hyperopic). The X-linked hereditary condition (called juvenile retinoschisis) affects only males and usually involves the macula with loss of central vision. The congenital condition is characterized by a splitting of the nerve fibre layer from the retina whereas the acquired form, which is the most common, results in a splitting at the outer plexiform layer. The latter usually begins in the temporal periphery appearing as a coalescence of microcystoid degenerations with a smooth transparent elevation and associated with an absolute scotoma. The condition may spread to involve the entire peripheral fundus. Holes in the two layers are common and are a sign of progression. The inner layer contains blood vessels and sometimes has small whitish flakes on it, which are called ‘snowflakes’.
retinoschisis, juvenile See retinoschisis.
retinoscope An instrument for determining objectively the refractive state of the eye. It consists of a light source, a condensing lens and a mirror. The mirror is either semitransparent or has a hole through which the retinoscopist can view the patient’s eye along the retinoscope’s beam of light. A patch of light is formed on the patient’s retina and by moving that patch in a given direction and observing the direction in which it appears to move after refraction by the patient’s eye, the retinoscopist can determine whether the patient’s retina is focused in front of, at, or behind the retinoscope’s sight hole. If the light reflected from the patient’s fundus (called the retinoscopic reflex or light reflex) and observed in the patient’s pupil through the retinoscope moves in the same direction as the movement of the mirror (this is referred to as a with movement), the eye is hyperopic. If the reflex moves in the opposite direction to that of the mirror (against movement), the eye is myopic. Sometimes it is impossible to see a clear movement one way or the other but only a bipartite reflex, showing opposite movements in the two sectors of the pupils (this is called a split reflex or a scissors movement). The refractive error is determined by placing lenses of various powers in front of the patient’s eye until no movement is seen, i.e. the whole pupil is either illuminated or dark and the image of the patient’s retina is then conjugate with the plane of the retinoscope’s sight hole. When this phenomenon occurs the neutral point has been reached. The neutral point is measured for each principal meridian of the eye if it is astigmatic. To arrive at the patient’s error of refraction the dioptric power corresponding to the distance between patient and retinoscope (called the working distance) is subtracted from the total lens power used to obtain neutralization. The amount of dioptric power subtracted is called the allowance. (Fig. R13) Syn. skiascope.
See band, retinoscopic; chromoretinoscopy; reflex, fundus; velonoskiascopy.
spot r. A retinoscope that projects a circular beam of light upon the patient’s retina.
streak r. A retinoscope that projects into the patient’s eye an oblong streak, which can be adjusted in width and rotated in various meridians. It is more efficient than the spot retinoscope in determining astigmatism.
retinoscopic artifact An error encountered in determining the refractive error by retinoscopy. This error is due to the fact that the retinal layer which reflects the retinoscopic light is not situated within the photoreceptors (where an image must be formed to appear in focus) but in front of them. Retinoscopic light is reflected by the vitreous-retina interface due to the difference in their refractive indices (that difference may not exist in some species and in old eyes). Consequently retinoscopic results tend to be more hyperopic or less myopic than is actually the case. The smaller the eye the greater the error because the thickness of the retina is nearly constant across species. This error is equal to about 0.25 D in young human adults, about 1 D in infant eyes and can reach some 8 D in very small animals. Syn. retinoscopic error; small eye artifact (so called because the effect is much greater for small eyes than for large eyes).
retinoscopy (ret) The determination of the refractive state of the eye by means of a retinoscope. Syn. skiascopy; shadow test.
See chromoretinoscopy.
dynamic r. Retinoscopy performed with the patient fixating binocularly a near object such as a letter, a word, or a picture mounted on, or held close to, the retinoscope and wearing the distance correction. No working distance lens power is subtracted or added to the finding since the plane of regard is at the same distance as the retinoscope. Syn. book retinoscopy (this term is restricted to the case when the patient is reading a text); cognitive retinoscopy (when the patient fixates a single letter or reads some words); near point retinoscopy.
See accommodation, lag of; accommodation, objective; retinoscopy, MEM; retinoscopy, Mohindra’s technique of; retinoscopy, static.
MEM r. A type of dynamic retinoscopy in which the retinoscope is held in the same plane as the near fixation target and lenses are interposed very briefly in front of one eye, while the other eye fixates the target. The aim of the method is to estimate the fundus reflex motion without disturbing the accommodative stance, that is, by leaving each lens in front of one eye for less than one second, until the neutral point is achieved. The results in non-presbyopic subjects generally show a lag of accommodation of 0 to +0.75 D. Note: MEM is an acronym of ‘monocular estimate method’.
Mohindra’s technique of r. Retinoscopy performed in a darkened room at 50 cm (20 inches) with the patient fixating the retinoscope light monocularly (the other eye being occluded). Distance retinoscopic refraction is derived by adding –1.00 D (to take into account the working distance and the state of accommodation in the dark) to the value found by near retinoscopy. The technique is used in paediatric optometry. Syn. monocular near retinoscopy.
See accommodation, resting state of; retinoscopy, dynamic; retinoscopy, MEM.
near point r. See retinoscopy, dynamic; Mohindra’s technique of.
static r. Retinoscopy performed with the patient fixating a target at distance or with accommodation paralysed.
retinotectal pathway See pathway, retinotectal.
retinotopic map Term referring to the fact that the precise spatial arrangement of the retina is maintained throughout the visual pathway.
See geniculate bodies, lateral; pathway, visual.
retraction syndrome, Duane’s See syndrome, Duane’s.
retractor muscles, eyelid See muscle, levator palpebrae superioris; muscles, Müller’s palpebral.
retrobulbar Behind the eyeball as, for example, retrobulbar optic neuritis.
retrobulbar block See injection, retrobulbar.
retrobulbar optic neuritis See neuritis, optic.
retrography See mirror writing.
retro-illumination See illumination, retro-.
retrolental fibroplasia See retinopathy of prematurity.
retrolental space of Berger See postlenticular space, Berger’s.
retroscopic angle See angle, retroscopic.
retrospective study See study, retrospective.
reverse-geometry contact lens See lens, reverse-geometry contact; lens, ortho-k.
reversed image See image, inverted.
reversible spectacles See spectacles, reversible.
rhegmatogenous retinal detachment See retinal detachment, rhegmatogenous.
rheumatoid arthritis See arthritis, rheumatoid.
rhinoconjunctivitis, allergic See conjunctivitis, allergic.
rhodopsin Visual pigment contained in the outer segments of the rod cells of the retina and involved in scotopic vision. When light stimulates the retina, the chromophore of the pigment molecule ‘11-cis’ retinal (which is vitamin A aldehyde) isomerizes to ‘all-trans’ retinal. This leads to other chemical transformations which carry on even in the absence of light. The first stage is prelumirhodopsin, then lumirhodopsin and finally metarhodopsin (of which there are two types). This last transformation may lead to the breakdown of the molecule into retinal and opsin. The molecule is regenerated by recombining retinal and opsin with some enzymes. The absorption spectrum of rhodopsin has a maximum around 498 nm. The isomerization from ‘11-cis’ to ‘all-trans’ also gives rise to the process of transduction in which the membrane potential covering the pigment molecules in the outer segment changes towards a hyperpolarization of the cell. This is the first step in the nervous response to a light stimulation of the retina. Syn. visual purple (not used any more); erythropsin.
See adaptation, dark; bleaching; potential, receptor; spectrum, absorption; transduction.
rhythm, circadian The characteristic of some processes to repeat at approximately 24-hour intervals. Examples: intraocular pressure is at its lowest every evening and highest every morning; corneal sensitivity is at its lowest every morning and highest every evening. Syn. diurnal cycle (provided the variation in activity or behaviour is more or less divided equally between night and day).
See melanopsin.
Riddoch phenomenon See phenomenon, Riddoch.
Rieger’s syndrome See syndrome, Rieger’s.
rigidity, ocular The resistance of the coats of the eye to indentation. This factor is taken into account in the tables used when determining the intraocular pressure by means of an indentation tonometer such as that of Schiötz. The tables are based on an eye of average ocular rigidity but if the eye has high or low rigidity, an error is introduced into the readings: means of minimizing this effect have been devised.
See tonometer, impression.
Riley–Day syndrome See syndrome, Riley–Day.
rim That part of a spectacle frame which partly or completely surrounds the lens.
rimexolone See antiinflammatory drug.
rimless fitting Fitting an edged lens to a rimless mount. The process may include drilling, slotting, strap adjustment, etc. (British Standard).
See lens groove; spectacles, rimless.
rimless spectacles See spectacles, rimless.
ring Any line, object or structure that is circular in shape.
anterior limiting r. of Schwalbe A bundle of connective tissue and elastic fibres forming the junction between the anterior termination of the trabecular meshwork and Descemet’s membrane of the cornea. If it is unusually thickened or prominent, it is called posterior embryotoxon. Syn. line of Schwalbe.
See gonioscopy, direct; syndrome, Axenfeld’s; syndrome, Rieger’s.
Coat’s white r. A small, oval or circular, whitish-grey ring opacity in the cornea found at the level of Bowman’s layer, usually near the periphery. It is composed of a deposition of iron, possibly located at the site of a previous foreign body injury. No treatment is necessary.
Fleischer’s r. A narrow ring of brownish or greenish pigment containing iron, deposited in the epithelium of the cornea and surrounding (completely or partially) the base of the cone in keratoconus. It is not always present in that disease. Syn. Fleischer’s line.
Kayser–Fleischer r. A ring of pigment granules containing copper located in Descemet’s membrane around the periphery of the cornea. It has a brown or greyish-green colour to the unaided eye or golden brown to reddish colour when viewed through the slit-lamp and appears in nearly all cases of Wilson’s disease.
Landolt r. See Landolt ring.
Newton’s r’s. Circular, concentric interference fringes surrounding a point of contact when two glass surfaces are pressed together. The thicker the air film separating the two surfaces the greater the number of concentric rings.
scleral r. The appearance of a white patch of sclera adjacent to the optic disc when the retinal pigment epithelium and the choroid do not extend to the optic disc.
Soemmering’s r. Lens remnants found within the periphery of the capsular bag. It may occur as a result of trauma, but more commonly following extracapsular cataract extraction. The pupillary area is usually left relatively free.
See after-cataract; pearls, Elschnig’s.
Vossius’ r. An annulus-shaped opacity imprinted on the anterior lens capsule and containing pigment from the posterior epithelium of the iris. It occurs as a result of a blunt trauma to the eye in which the aqueous pressure throws the iris forcefully against the lens. The ring is usually located sufficiently off-axis not to impair vision.
Wessley r. A disc-shaped greyish opacity made up of inflammatory cells consisting of antigen-antibody complexes located in the corneal stroma. It is seen in stromal interstitial keratitis resulting from a herpes simplex virus or disciform keratitis. The ring may attract neovascularization. Syn. immune ring of Wessley.
Riolan muscle See muscle of Riolan.
Risley prism See prism, rotary.
river blindness See onchocerciasis.
Rizzuti’s sign See sign, Rizzuti’s.
rod-free area See foveola.
rod monochromat See monochromat.
rod spherule The onion-shaped synaptic terminal of a rod photoreceptor located in the outer molecular (plexiform) layer of the retina. There is a deep pit (invagination) in the base of the terminal, which contains the dendrites of bipolar and horizontal cells, often two of each. The neurotransmitter is glutamate, which is stored in vesicles contained in the terminal, and when the photoreceptors are stimulated by light the release of glutamate is decreased.
See cell, rod; hyperpolarization; neurotransmitter.
Roenne nasal step When scotomata occur above and below the fixation point they meet in the nasal field and form a horizontal step-like defect. It is one of the signs of glaucoma.
room, Ames A specially constructed room in which all the visible features have been distorted to make the room appear rectangular from one specific point of observation. In particular, the back wall of the room appears perpendicular to the line of sight, with left and right corners appearing equidistant to the observer, although in reality one corner is much further away. To an observer looking into the room, people of identical heights standing one in each corner of the room appear of clearly different height. The person standing in the far away corner does indeed produce a smaller retinal image, but since the observer believes that they are at the same distance, the person standing closer ‘must be larger’. The Ames room demonstrates how perceived distance influences perceived size. Syn. Ames distorted room.
See illusion, moon; perception, depth.
room, leaf A cubical box, about 2 metres square, with its walls vertical and one open side. The interior surfaces are covered with artificial leaves of various sizes, which stick out in a random manner. An observer looking binocularly into the room from the centre of the open side will see its cubical shape due to stereopsis. However, monocularly the room appears almost flat as the monocular cues to depth perception are almost completely eliminated in this room. The leaf room is used to detect and measure spatial distortions resulting from aniseikonia. It can also be used to demonstrate spatial distortion using meridional size lenses.
See lens, aniseikonic; perception, depth.
rosacea, acne See acne rosacea.
rosacea keratitis See keratitis, rosacea.
rose bengal An iodine derivative of fluorescein having vital staining properties but unlike fluorescein it is a true histological stain, which binds strongly and selectively to cellular components. The colour of this stain is red. It has the disadvantage of causing some pain in a good percentage of eyes. It stains dead or degenerated epithelial cells but not normal cells and is used to help in the diagnosis of corneal abrasion, keratitis, keratoconjunctivitis sicca, lagophthalmos, etc.
See fluorescein; lissamine green.
Rosenmuller, valve of See valve of Rosenmuller.
rotary prism See prism, rotary.
Roth’s spots See spots, Roth’s.
rouge A powder consisting of iron oxide, used to polish lenses, metals, etc.
roughing Grinding of the surface of a lens to the approximate curvature and thickness with a coarse abrasive.
See blocking; smoothing; surfacing.
rubeosis iridis Neovascularization of the iris characterized by numerous coarse and irregular vessels on the surface and stroma of the iris. The new blood vessels may cover the trabecular meshwork, cause peripheral anterior synechia and give rise to secondary glaucoma. The most frequent causes are diabetes mellitus and central retinal vein occlusion.
See glaucoma, neovascular; iritis; retinal vein occlusion.
Rubin’s vase An ambiguous drawing, which may be perceived either as a vase or as two human profiles facing each other (Fig. R14). See figure, Blivet; Necker cube; Schroeder’s staircase.

rule 1. A guiding principle governing an action or a procedure. 2. A rigid, graduated rod for measuring length.
Javal’s r. A relationship that relates corneal astigmatism to the total astigmatism of the eye. It states that
where At and Ac are the total and corneal astigmatism, respectively. This relationship is relatively accurate in predicting the total astigmatism of the eye when corneal astigmatism is greater than 2 D. For smaller amounts of corneal astigmatism, a more appropriate version of Javal’s rule is
Kestenbaum’s r. A procedure designed to estimate the power of the addition needed to read ordinary newsprint (about Jaeger 5 or N7–8) in low vision patients. It consists of dividing the denominator of the Snellen visual acuity fraction by its numerator (i.e. 1/Snellen visual acuity). Example: if the Snellen visual acuity is 6/60 (20/200) the power of the add will be +10 D, which corresponds to a magnification of 10/4 = 2.5×. Syn. Kestenbaum’s formula.
Kollner’s r. Lesions of the outer retinal layers and changes in the ocular media produce a blue-yellow colour vision defect, whereas lesions of the inner retinal layers, the optic nerve and the visual pathway produce a red-green defect. Examples: age-related maculopathy causes a blue-yellow defect; optic neuritis causes a red-green defect. There are exceptions to this rule, particularly during the evolution of a disease. Syn. Kollner’s law.
near point r. A device for measuring the near points of accommodation and convergence. The RAF rule consists of a graduated four-sided bar on which is mounted a movable target holder which can be moved in the median plane of the head. The bar is calibrated in centimetres and dioptres (Fig. R15).
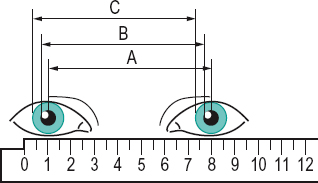
PD r. A ruler calibrated in millimetres used for measuring the interpupillary distance. Some have the zero point in the middle and the gradations on each side to measure two half-distances thus taking into account facial asymmetry. Many PD rules also have facilities for measuring frames (Fig. R16). Syn. pupillometer (although it is an incorrect use of this term, it is frequently used as a synonym).
Table R3
Power of the addition required (and corresponding focal length) to read ordinary newsprint (about J5 or N8) in low vision patients, for various acuities. The add is calculated according to Kestenbaum’s rule and is an estimate
| Acuity at 40 cm | Snellen equivalent at 40 cm | power of add (D) | focal distance of add (cm) | |
| (m) | (ft) | |||
| 40/80 | 6/12 | 20/40 | +2 | 50 |
| 40/100 | 6/15 | 20/50 | +2.5 | 40 |
| 40/120 | 6/18 | 20/60 | +3 | 33 |
| 40/140 | 6/21 | 20/70 | +3.5 | 29 |
| 40/160 | 6/24 | 20/80 | +4 | 25 |
| 40/200 | 6/30 | 20/100 | +5 | 20 |
| 40/250 | 6/38 | 20/125 | +6.25 | 16 |
| 40/320 | 6/48 | 20/160 | +8 | 12.5 |
| 40/400 | 6/60 | 20/200 | +10 | 10 |
| 40/500 | 6/75 | 20/250 | +12.5 | 8 |
| 40/600 | 6/90 | 20/300 | +15 | 6.7 |
| 40/800 | 6/120 | 20/400 | + 20 | 5 |
| 40/1200 | 6/180 | 20/600 | + 30 | 3.3 |
| 40/1600 | 6/240 | 20/800 | + 40 | 2.5 |
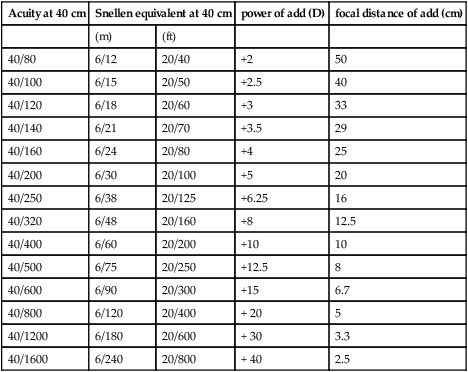

Prentice’s r. See law, Prentice’s.
Prince’s r. A device for determining the location of the near point of accommodation and the amplitude of accommodation. It consists of a ruler scaled in dioptres on one side and in millimetres on the other. One end of the ruler is held against the face and a test card is moved along the ruler towards the eye until a blur is noticed. The amplitude of accommodation in dioptres represents either the ocular accommodation (if the reference point is the cornea) or the spectacle accommodation (if the reference point is the spectacle plane).
Rx Traditionally this symbol, which is an abbreviated form of the Latin word recipe, meaning ‘take’, appears before the main part of a prescription. It is nowadays commonly used as a synonym for prescription.
See prescription.