74. Pyelonephritis
Definition
Pyelonephritis is a potentially organ-threatening, fatal inflammation of the kidney and renal pelvis secondary to a bacterial infection that begins in the interstitial tissues and rapidly extends to involve the renal tubules and glomeruli, culminating in the renal blood vessels.
Incidence
Approximately 250,000 cases of pyeolonephritis occur each year in the United States. About 192,000 of these cases require hospitalization. There have been no discernable racial or ethnic predilections, but females strongly outnumber males.
Etiology
The root cause of pyelonephritis is bacterial infection/invasion of the kidney parenchyma (see box below). Finding the cause of pyelonephritis requires determining the following: (1) which pathogens are typically cultured and their frequency; (2) whether the urinary tract infection is complicated; and (3) which pathogenic organism is involved in the complicated urinary tract infection. A complicated urinary tract infection (UTI) is defined as one occurring along with an additional factor that reduces the efficacy of antimicrobial therapy and leads to therapy failure, relapses, or persistence of infection.
Causative Organisms in Pyelonephritis
• Citrobacter species
• Coagulase-negative Staphylococci
• Enterobacter species
• Enterococci
• Escherichia coli
• Group B Streptococci
• Klebsiella species
• Proteus mirabilis
• Pseudomonas aeruginosa
• Staphylococcus aureus
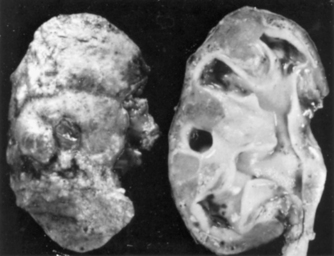 |
| Pyelonephritis. Chronic pyelonephritis. The surface (left) is irregularly scarred. The cut section (right) reveals characteristic dilation and blunting of calyces. |
Signs and Symptoms
• Anorexia
• Chills
• Fever (sometimes)
• Malaise
• Mild-to-moderate or severe pain
• Nausea
• Rigor
• Tachycardia
• Unilateral or bilateral flank pain
• Vomiting
Medical Management
The mainstay of medical care of the patient with pyelonephritis is supportive. It consists of rest, antipyretics, analgesics (oral or parenteral), antiemetics (oral or parenteral), dysuric relief using urinary tract analgesics, and oral or parenteral fluid to maintain proper hydration. However, these palliative measures may not be sufficient. Hospitalization may become necessary to intensify treatment because of the inability to tolerate oral intake, poor treatment compliance, poor treatment follow-up, unstable vital signs, increasing severity of signs and symptoms, pregnancy, and co-morbidity problems (e.g., diabetes mellitus, an acquired immunodeficiency). Patient treatment should be parenteral until observable clinical improvement is demonstrated, usually requiring 14 days of treatment.
Surgical intervention is not typically required except to preserve the function of the kidney or as a life-saving measure. Surgical intervention may become necessary to alleviate situations that lend themselves to recurrent infections and/or renal damage. These may include congenital anomalies, urogenital tract fistula, hypertrophic prostate, renal calculus (calculi), and vesicoureteral reflux. Surgical intervention may become emergent if the patient is febrile, has positive blood culture results for more than 48 hours, exhibits deterioration in condition, or appears toxic for more than 3 days (72 hours).
Complications
• Acute renal failure
• Chronic renal failure/damage
• Emphysematous cystitis
• Emphysematous pyelonephritis
• Obstructing calculus
• Phrenic abscess
• Renal capillary necrosis
• Renal cortical abscess (renal carbuncle)
• Renal corticomedullary abscess
• Sepsis syndromes
• Staghorn calculus
• Xanthogranulomatous pyelonephritis
Anesthesia Implications
The nature or etiology of the patient’s presentation to the operating room is an important factor for formulation of the anesthetic plan. The patient with pyelonephritis may present for emergent surgical intervention to rectify any of several conditions, such as emphysematous pyelonephritis or cystitis, phrenic abscess, or xanthogranulomatous pyelonephritis (see Complications above). The patient may be significantly febrile and dehydrated. Dehydration may result from the accompanying nausea and vomiting. Antibiotic therapy may be ongoing, and the anesthetist must be vigilant to adhere to the administration schedule for the antibiotics. Electrolyte imbalances, particularly potassium, are to be expected and may be partially the result of the significant emesis the patient may have. Both electrolyte concentrations and fluid balance should be determined preoperatively and corrective measures initiated as soon as possible. The patient may be septic, depending on the emergent condition precipitating the surgical intervention. The anesthetist should induce general anesthesia using the classic rapid sequence technique.
The anesthetist must ensure adequate intravenous access. Ideally, two large-bore IV catheters would be started before anesthesia to initiate adequate fluid resuscitation, maintain antibiotic administration schedule, and/or administer any vasopressors or vasoactive medications that may be required. Significantly febrile patients may require active cooling measures. The anesthetist may need to administer cooled IV fluid, apply cool packs to the axillae and/or groin, and use a forced-air cooling blanket to reduce the patient’s temperature.
Frequently, the patient with pyelonephritis presenting emergently to the operating room requires complete or partial nephrectomy. As such, it may be necessary to place the patient in a lateral decubitus position. The anesthetist must take care to ensure proper positioning of the patient to prevent potential nerve injury. The anesthetist must also be acutely aware of the patient’s respiratory status, especially the presence of any pulmonary co-morbidity factors that may be exacerbated by placing the patient in a lateral decubitus position. For example, pneumonia in a lobe of the dependent lung in the lateral position may reduce gas exchange and/or exacerbate any shunting that may be present.
Factors Associated with Complicated Urinary Tract Infection
• Acquired immunodeficiency syndrome
• Acute renal colic
• Age over 65 years
• Analgesic abuse
• Bladder abscess
• Congenital immunodeficiency syndrome
• Diabetes mellitus
• Fistulae
• Foreign bodies (e.g., stents or calculi)
• Gross hematuria
• Hematogenous spread
• Infant/neonate
• Infected renal calculi
• Neurogenic bladder
• Neutropenia
• Nosocomial infection
• Obstruction
• Pregnancy
• Prior renal stones
• Renal impairment
• Renal transplant
• Resistant bacterial infection
• Sickle cell disease
• Tuberculosis
• Urinary diversion procedures
• Vesicoureteral reflux
• Yeast/fungal infection







